Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.

Surgical oncology is the oldest and most fundamental part of cancer treatment. It has grown from simply removing tumors to a science that uses data and knowledge of biology to control cancer. Today, surgical oncology is more than just taking out tumors. It combines surgery with an understanding of tumor biology, genetics, and how the body works as a whole. This field focuses on the surgical treatment of tumors, especially cancers, and covers all stages of care from diagnosis and staging to removing tumors, reducing tumor size, and providing relief to improve quality of life.
Today’s surgical oncologist combines technical skill with a strong understanding of cancer biology. Success is no longer just about removing what can be seen, but about making sure no cancer cells are left at the edges while keeping as much healthy tissue as possible. This approach, called organ preservation, depends on knowing how tumors interact with their surroundings and spread. Surgeons now see tumors as complex structures that use the body’s resources to grow. The goal in surgery is to break the tumor’s support systems, block its spread, and lower the amount of cancer so the body’s immune system or other treatments can finish the job.
From a cellular biology and regenerative medicine viewpoint, surgical oncology affects how the body maintains balance. Every cut made during surgery starts a series of healing and inflammatory reactions. How the surgeon handles tissue, the tools used, and how the area is rebuilt all affect the local environment. It is now recognized that surgery can temporarily weaken the immune system by releasing certain chemicals. Because of this, modern surgical oncology aims to reduce this stress response by using less invasive methods and recovery plans that help prevent conditions that could let cancer spread after surgery.

The main idea behind curative surgery is to remove the main tumor before it spreads throughout the body. This is based on the idea that cancer usually spreads first to nearby lymph nodes and then to other organs. Although we now know some cancers can spread earlier, controlling the main tumor is still very important. Taking out the main tumor stops it from sending more cancer cells into the body. Also, removing most of the tumor, called cytoreduction, can make the remaining cancer cells grow faster, which often makes them easier to treat with chemotherapy or radiation.
The interface between the tumor and the healthy host tissue is defined as the surgical margin. This is not a sharp line but a zone of biological interaction. The tumor microenvironment at the margin is rich in cancer-associated fibroblasts, immune cells, and extracellular matrix remodeling enzymes. Achieving a negative margin, or R0 resection, means removing this entire complex. If microscopic cells are left behind (R1 resection), the altered stromal environment, rich in growth factors released during wound healing, can actually stimulate these residual cells to grow more aggressively. Therefore, the surgical strategy is dictated by the biology of the margin; knowing whether a tumor pushes against tissues or infiltrates them determines how wide the excision must be.
Molecular Dynamics of the Surgical Field

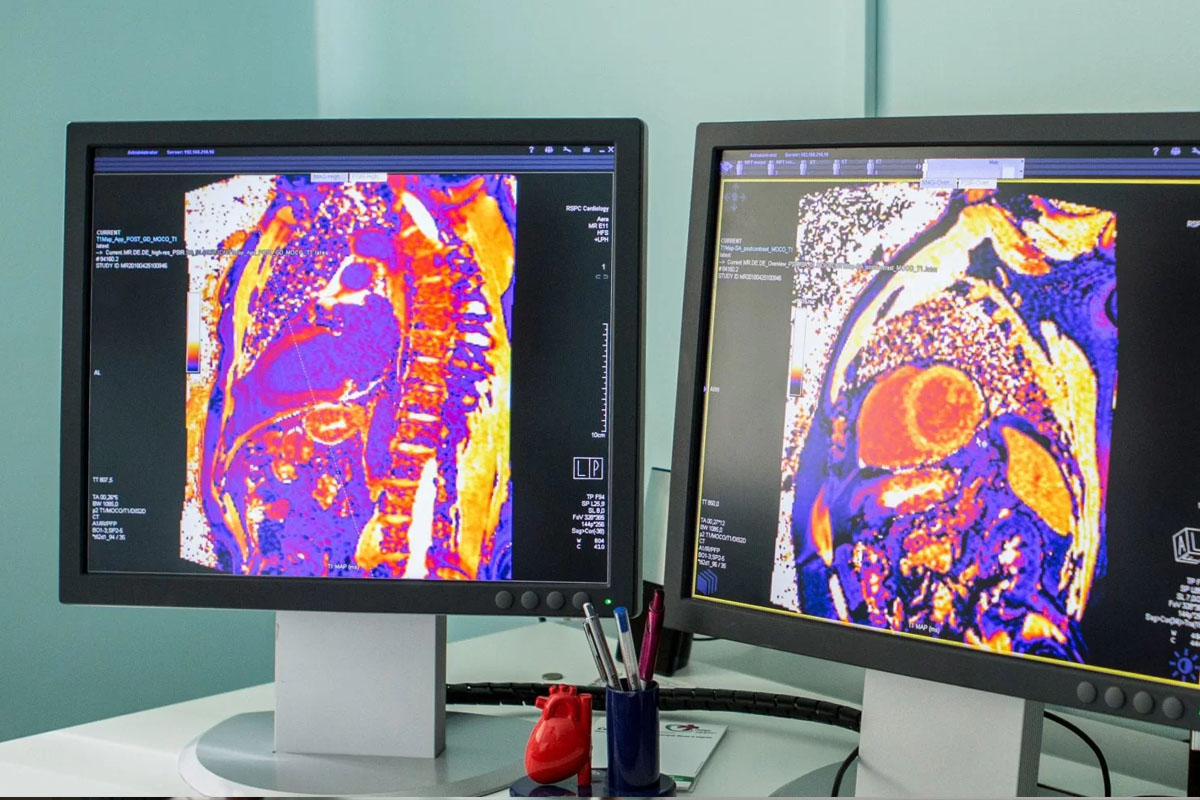
Global biotechnology has revolutionized surgical oncology through the development of precision guidance systems. The era of exploratory surgery has been replaced by image-guided intervention. Fluorescence-guided surgery utilizes tumor-specific contrast agents, such as indocyanine green or 5-ALA, which accumulate in metabolically active cancer cells. When illuminated with near infrared light, the tumor glows, allowing the surgeon to visualize microscopic extensions of the disease that are invisible to the naked eye. This real-time molecular imaging integrates biotechnology directly into the sterile field, enhancing resection precision and reducing the risk of positive margins.
Bioengineering has also changed how surgeons rebuild the body after removing large tumors. Sometimes, this means reconstructing complex parts like the jaw, breast, or esophagus. Today, doctors use materials like acellular dermal matrices, tissue transplants, and 3D-printed scaffolds with the patient’s own stem cells. These methods help restore both appearance and function, allowing the new tissue to work naturally with the patient’s body instead of just patching the area.
Modern surgery often uses advanced energy devices instead of just scalpels. These tools use things like ultrasonic vibration, radiofrequency, or plasma to cut tissue and stop bleeding at the same time. For example, ultrasonic shears use friction to change proteins and seal blood vessels, causing less damage than older methods. Protecting nearby healthy tissue is very important to keep nerves and other important structures working properly.
Key Physiological Functions Preserved

Send us all your questions or requests, and our expert team will assist you.
Curative surgery is performed when the tumor is localized, and there is a high probability of removing all cancer cells from the body, aiming for a complete cure and long-term survival. Palliative surgery is performed when the cancer has spread and cannot be cured, with the primary goal of relieving symptoms such as pain, obstruction, or bleeding to improve the patient’s quality of life.
A surgical margin is the rim of healthy appearing tissue surrounding the tumor that is removed along with the cancer. Pathologists examine this rim under a microscope to ensure no cancer cells touch the outer edge. A clean or negative margin suggests that all the tumor has been removed, while a positive margin indicates that cancer cells remain in the body.
Inoperable usually means that a tumor cannot be removed safely because it has invaded vital structures like major blood vessels or the heart, or because the patient is too frail to withstand the stress of surgery. It does not necessarily mean the cancer is untreatable, as radiation or chemotherapy may still be effective options.
Robotic surgery provides surgeons with high-definition 3D vision, magnification, and instruments with a greater range of motion than the human hand. This allows for more precise dissection in tight spaces, leading to less blood loss, less pain, shorter hospital stays, and potentially better nerve and functional preservation compared to traditional open surgery.
Cytoreductive surgery, also known as debulking, is the removal of as much of the tumor as possible when complete removal is not feasible. This is often done in ovarian cancer or certain sarcomas to reduce the number of cancer cells, making the remaining cells more responsive to chemotherapy and radiation.

Cancer metastasis is a complex process. It involves the spread of malignant tumors to other parts of the body. Knowing where cancer spreads first is
Lung cancer is a common cancer worldwide and has a high death rate, largely because it often metastasizes. Where lung cancer first spreads is key

Over 2 million PET scans are done every year in the U.S. to aid in tumor detection. These scans help find tumors and evaluate lung


Nearly 70 million ultrasound procedures happen every year in the United States. A big part of these are transvaginal ultrasounds for checking health. Many people
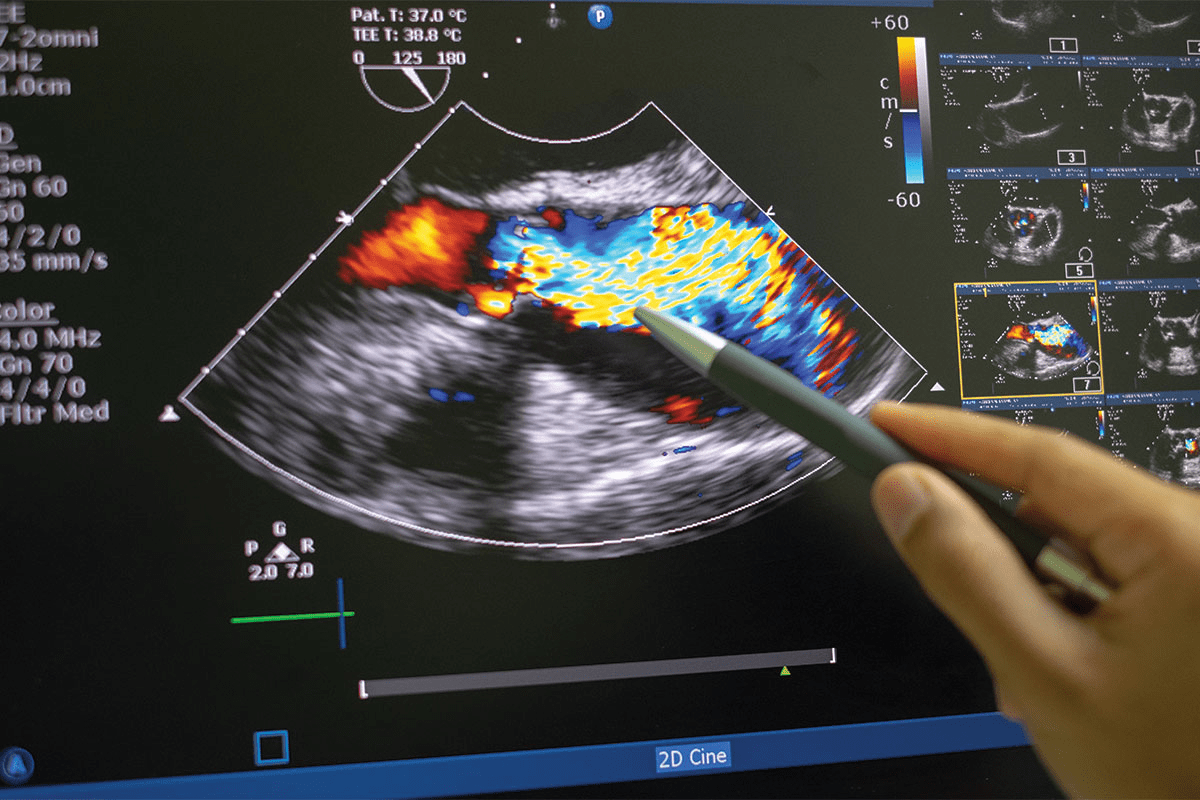
Ultrasound technology is key in finding cancers early. A recent study showed ultrasound can spot cancerous tumors very accurately. This change is big for cancer

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)