Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.
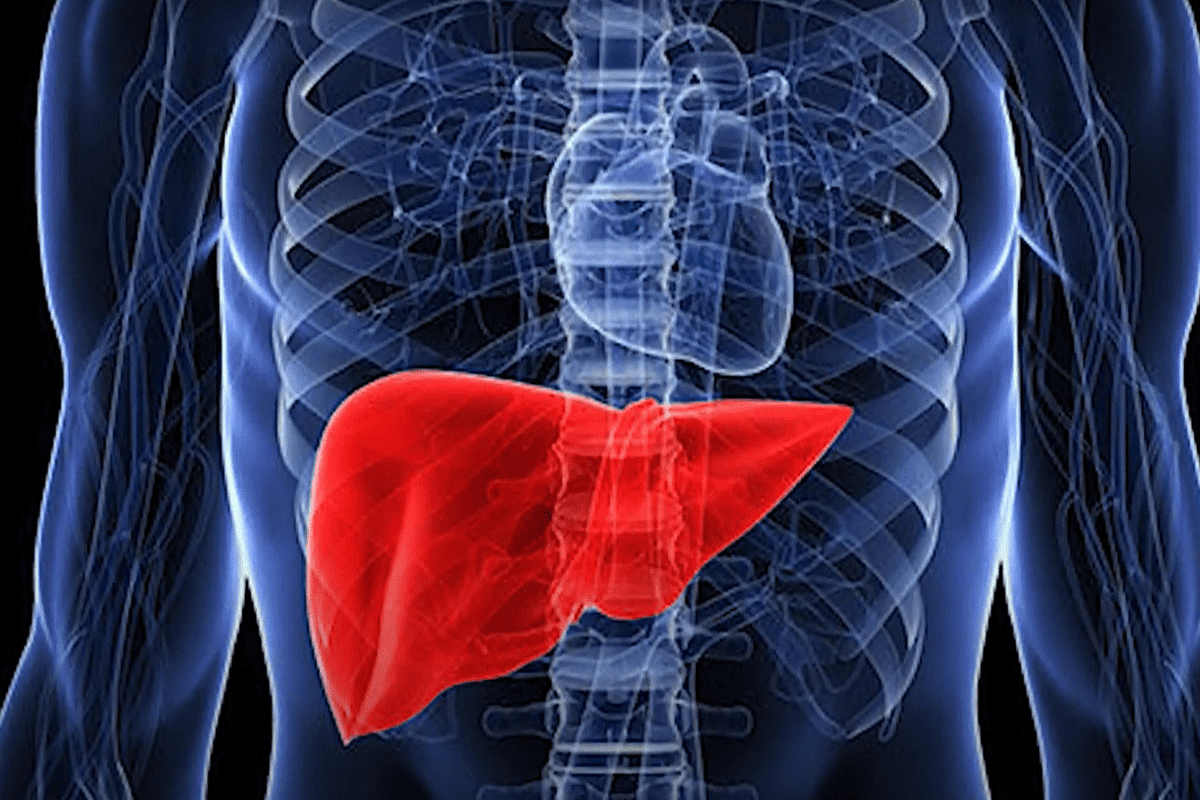
The liver is the largest internal organ in the body and carries out more than five hundred essential functions. Located in the upper right part of the abdomen and protected by the rib cage, it serves as the main center for metabolism. The liver has a unique structure with two blood supplies: oxygen-rich blood comes from the hepatic artery, while nutrient-rich blood from the digestive tract comes through the portal vein. This setup lets the liver process almost everything we eat, breathe, or absorb, filter out toxins, and make important proteins before sending blood back into circulation.
Hepatocytes are the main working cells in the liver and are grouped into hexagonal lobules. They produce bile, which helps digest fats and absorb vitamins A, D, E, and K. The liver also manages the body’s energy by storing extra glucose as glycogen and releasing it when needed. It makes blood-clotting factors to stop bleeding from small injuries and produces albumin, a protein that keeps fluid levels balanced in the blood and helps prevent swelling.
Understanding the complexity of hepatic function is essential to grasping the gravity of liver malignancies. When cancer develops within this sophisticated network, it does not merely disrupt a localized area; it compromises the systemic stability of the entire organism. The liver’s remarkable capacity for regeneration, the ability to grow back tissue after injury, is a double-edged sword. While it allows recovery from acute damage, chronic injury creates a cycle of constant inflammation and repair, fostering an environment prone to genetic errors and subsequent neoplastic transformation.
Liver cancer is broadly categorized based on the origin of the malignant cells. Primary liver cancer originates directly from the tissues of the liver itself. In contrast, secondary or metastatic liver cancer spreads to the liver from another primary site, such as the colon or breast. The distinction is paramount, as the biological behavior, treatment protocols, and prognoses differ vastly. Hepatocellular Carcinoma (HCC) is the most prevalent form of primary liver cancer, accounting for the vast majority of cases globally. It arises from the hepatocytes, the primary functional cells described previously.
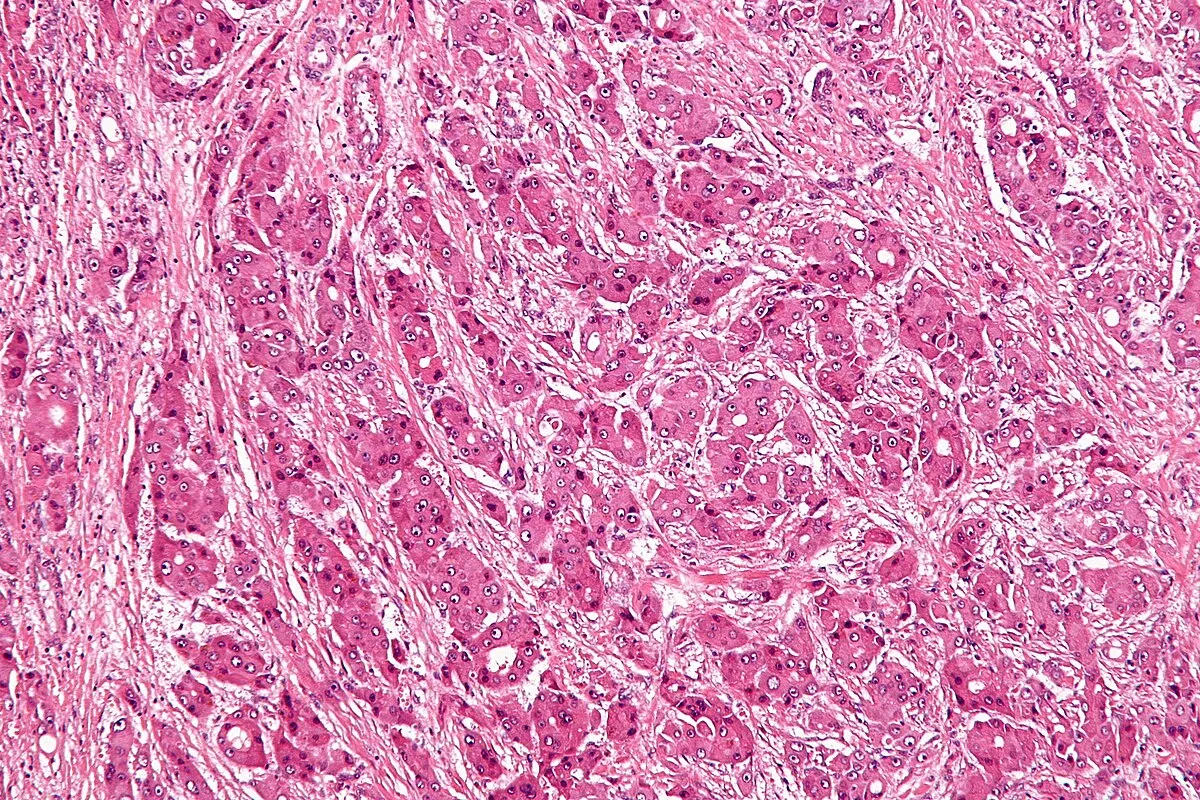
Hepatocellular Carcinoma develops because of changes in the liver’s environment. Normally, liver cells grow in a controlled way, but long-term inflammation and scarring disrupt this balance. Over time, genetic mutations build up, causing cells to grow out of control. Cancerous liver cells may still do some normal jobs, like making bile, which can make tumors look greenish. These tumors also have many blood vessels, drawing blood from the hepatic artery, which helps doctors spot and treat them using imaging and certain procedures.
Intrahepatic Cholangiocarcinoma is the second most common type of primary liver cancer. It starts in the cholangiocytes, which are the cells lining the bile ducts, not in the main liver cells. These tumors are usually more fibrous and have fewer blood vessels than HCC, and they often grow along the bile ducts, causing blockages. Other rare types include Hepatoblastoma, which mostly affects children, and Angiosarcoma, a fast-growing cancer from the liver’s blood vessels. Each type needs its own treatment approach.
Liver cancer is a major health problem around the world and is one of the top causes of cancer deaths. The number of cases varies by region, mostly because of differences in risk factors like viral hepatitis. East Asia and Sub-Saharan Africa have had the highest rates due to common Hepatitis B infections. However, as more people get vaccinated against Hepatitis B, the number of new cases in younger people in these areas is starting to level off or drop.
Conversely, Western nations are witnessing a concerning rise in liver cancer incidence. This increase is primarily attributed to the growing epidemic of metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease. The parallel rise in obesity and type 2 diabetes rates creates a new population at risk, independent of viral infection. This metabolic-driven tumorigenesis presents new challenges for public health systems, as the population at risk is vast and often asymptomatic until late stages.
Liver cancer affects more than just survival rates. It often strikes people during their working years, leading to serious economic and social problems. Treating liver cancer is complicated and needs advanced medical care, like special imaging, surgery, and transplants. This means people without access to these resources may have worse outcomes. To tackle this problem, we need a worldwide approach that includes not just new treatments, but also prevention through vaccination, antiviral medicines, and healthy lifestyle changes.
It usually takes many years for a healthy liver to become cancerous. Most liver cancers develop after cirrhosis, which is the final stage of long-term liver damage. In cirrhosis, healthy liver tissue is replaced by scar tissue that can’t do the liver’s job. This scarring changes the liver’s structure, blocks blood flow, and makes it work poorly. The few healthy cells left try to regrow in this harsh environment, which leads to more mistakes in their DNA.
Cirrhosis is the biggest risk factor for Hepatocellular Carcinoma, but it’s not always needed for cancer to develop. Sometimes, especially with Hepatitis B or non-alcoholic steatohepatitis, liver cancer can start even if there isn’t much scarring. Hepatitis B can insert its DNA into liver cells, causing cancer before cirrhosis happens. Because cancer can develop without severe scarring, it’s important to carefully monitor all high-risk patients.
The progression involves a stepwise accumulation of molecular alterations. Pre-cancerous nodules, known as dysplastic nodules, often precede frank carcinoma. These nodules exhibit cellular atypia and architectural distortion but have not yet invaded the surrounding tissue. Distinguishing these high-grade dysplastic nodules from early, small hepatocellular carcinomas is one of the most challenging aspects of hepatology. It often requires high-resolution imaging and, in some cases, biopsy. Understanding this sequence allows clinicians to intervene at the earliest possible stage, where curative options are most viable.


Send us all your questions or requests, and our expert team will assist you.
A liver cyst is a fluid-filled sac within the liver that is almost always benign and non-cancerous. These are very common and typically do not require treatment unless they become large enough to cause pain. Liver cancer, on the other hand, is a solid growth of malignant cells that invades tissue and can spread to different parts of the body.
Yes, the liver is the only internal organ capable of regenerating. If a portion of the liver containing a tumor is surgically removed (resection), the remaining healthy liver tissue can grow back to near its original size within a few weeks to months, provided the underlying liver is not too severely damaged by cirrhosis.
No. Hepatocellular carcinoma is a cancer that starts in the liver cells (primary liver cancer). Liver metastases are cancers that began elsewhere in the body, such as the colon or lung, and have spread to the liver. This distinction is crucial because the primary cancer type determines the treatment; for example, colon cancer spread to the liver is treated like colon cancer, not liver cancer.
Not necessarily. While fatty liver disease increases the risk of developing inflammation and eventually cirrhosis, which can lead to cancer, the majority of people with fatty liver do not develop cancer. However, managing the condition through diet and exercise is vital to prevent the progression to more serious liver damage.
The liver has a massive functional reserve and no pain receptors inside the organ itself. A tumor can grow to a substantial size without affecting the liver’s overall function or causing pain. Symptoms often do not appear until the cancer stretches the capsule covering the liver or affects nearby organs, leading to late-stage diagnoses.


Accurate diagnosis is key for liver health. A CT liver scan takes many images from different angles. This gives a full view of what’s inside.
immunotherapy vs chemotherapy Cancer treatment is tough, and protecting your liver during chemotherapy is key for your health. Chemotherapy can harm the liver, but there
For those dealing with liver or bile duct issues, the thought of liver stent surgery can be scary. But, thanks to recent advancements, this procedure

Managing hepatic drainage well is key for those with bile flow issues. At Liv Hospital, we focus on keeping liver health top-notch. We use the

When bile flow from the liver is blocked, it can cause serious symptoms. These can include jaundice, itching, and pain in the abdomen. At Liv

At Liv Hospital, we know how vital bile duct stent placement is. It helps treat many liver and digestive problems. By putting in plastic or

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)