Identify the symptoms of neurological disorders early. Learn about the causes including genetics and lifestyle to better understand your risks and health.
Send us all your questions or requests, and our expert team will assist you.
Neurological Symptoms and Risk Factors: When to Seek Help
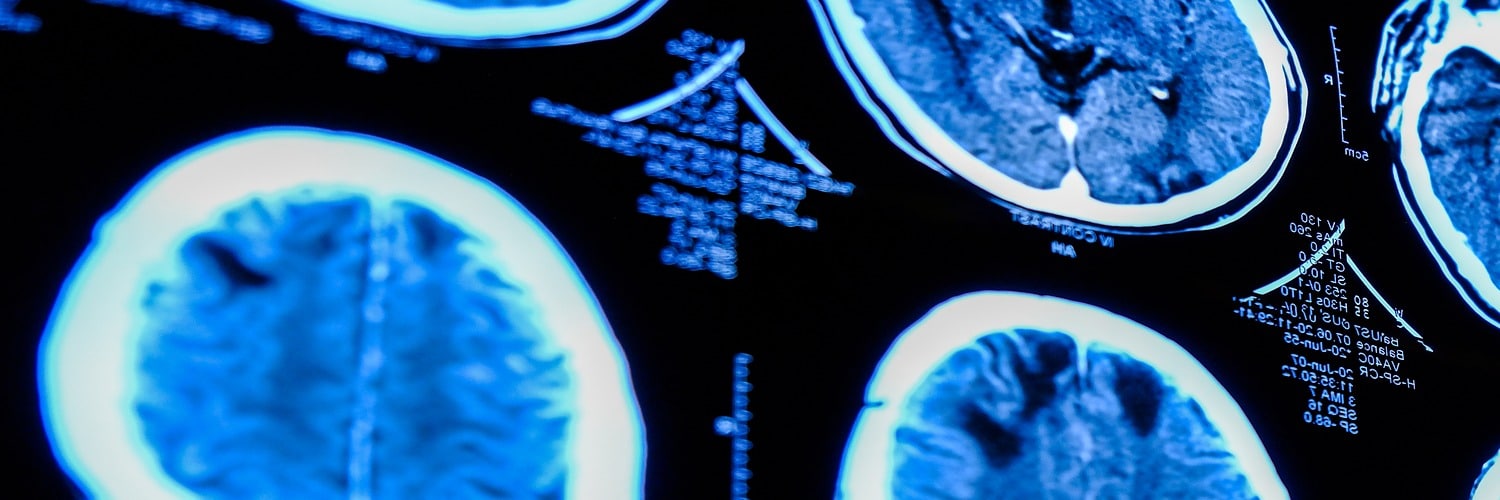
The nervous system is the body’s “electrical wiring,” and when a connection is frayed or broken, the signals can be confusing. Neurological symptoms vary widely because they depend entirely on which part of the brain, spine, or peripheral nerves is affected. For some patients, the sign is a sudden, thunderclap headache; for others, it is a gradual tingling in the toes. At Liv Hospital, we educate our international patients to recognize these signals early, as timely intervention is often the key to preserving function.
What are the Most Common Neurological Symptoms?

Because the nervous system controls everything from muscle movement to conscious thought, symptoms can be physical, cognitive, or sensory.
Key warning signs include:

How to Recognize a Stroke: The F.A.S.T. Protocol
A stroke is a “brain attack” where blood flow is cut off. It is the most critical emergency in neurology. Liv Hospital recommends every patient memorize the F.A.S.T. acronym to save lives:
Time is Brain: For every minute a stroke is left untreated, millions of neurons die. Liv Hospital’s Stroke Center is equipped for rapid mechanical thrombectomy to restore blood flow, but patients must arrive quickly.
Differentiating Pain: Migraine vs. Tension Headache
Not all headaches are created equal. Distinguishing between a common tension headache and a neurological condition like a migraine is essential for proper treatment.
Feature | Tension Headache | Migraine |
Pain Type | Dull, aching pressure (like a tight band). | Throbbing or pulsing pain. |
Location | Usually entire head or forehead. | Often on one side of the head. |
Severity | Mild to moderate. | Moderate to severe (incapacitating). |
Associated Symptoms | Rarely involves other symptoms. | Nausea, vomiting, sensitivity to light/sound. |
Warning Signs | None. | May be preceded by an “aura” (visual flashes). |
Signs of Peripheral Nerve Damage (Neuropathy)
Peripheral neuropathy is damage to the nerves outside the brain and spinal cord. It is a common complication of diabetes but can also result from chemotherapy or infections.
Symptoms typically start in the furthest points of the body (toes and fingers) and move inward:
What Causes Neurological Disorders?
Neurological conditions are rarely caused by a single factor. They are often a combination of genetic predisposition and environmental triggers.
Primary Risk Factors:

Differentiating Pain: Migraine vs. Tension Headache
You do not need to wait for a catastrophe to seek help. We recommend a consultation if you experience:
For international patients, Liv Hospital offers a “Neurological Check-Up” package designed to screen for these silent risks before they become emergencies.
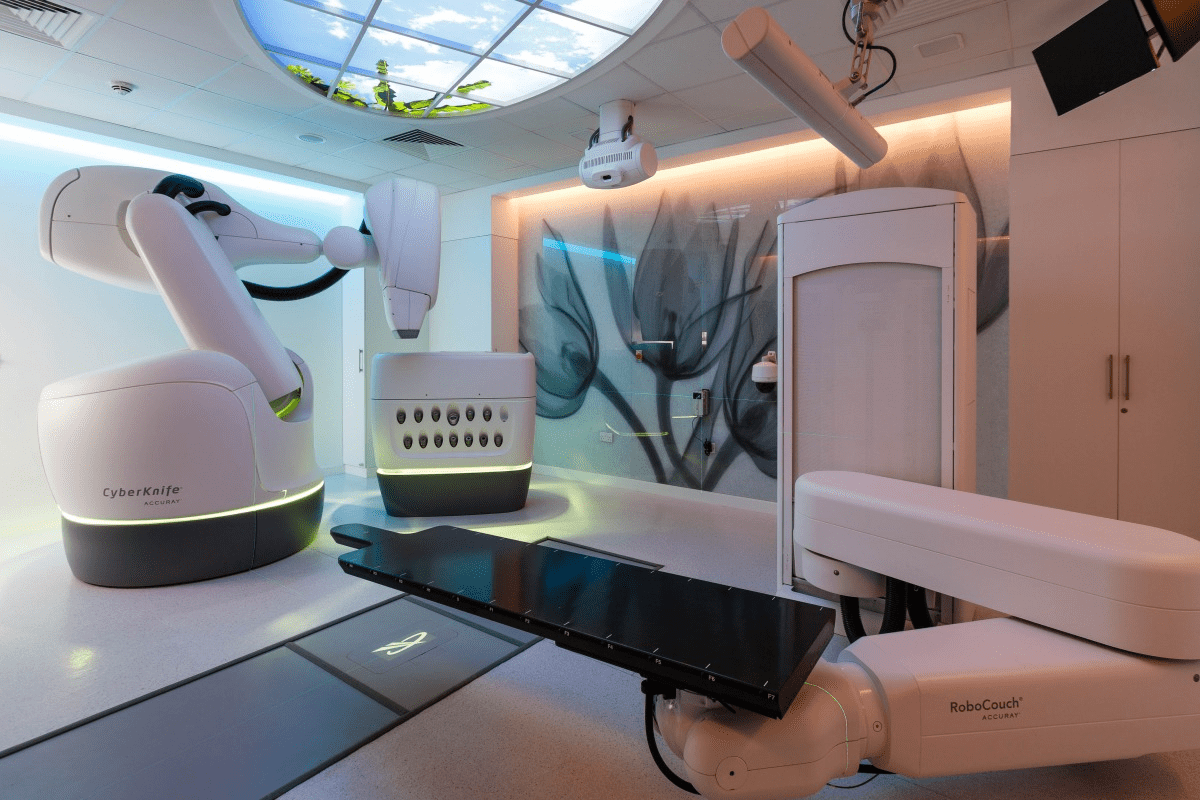
“Once a risk is identified, we move to solutions. Explore Treatment and Rehabilitation.”
Send us all your questions or requests, and our expert team will assist you.
A neurologist focuses on diagnosing and managing nervous system disorders through medication and therapy. In contrast, a neurosurgeon performs surgical procedures to treat physical causes like tumors or herniated discs.
In most healthcare systems and insurance plans, a referral from a primary care physician is required to ensure that your symptoms warrant a specialized neurological evaluation.
The doctor will take a detailed medical history, listen to your symptoms, and perform a physical examination to assess reflexes, strength, sensation, and coordination, and localize the problem.
Yes, severe anxiety and stress can manifest physical symptoms such as dizziness, numbness, tremors, and headaches, which can mimic organic nervous system disorders.
While genetic factors play a role, research suggests that a healthy lifestyle, including regular exercise, a balanced diet, social engagement, and cognitive stimulation, can significantly lower the risk or delay the onset of dementia.

Can Stress Cause Epilepsy? Understanding the Connection Between Stress and Seizures <image1> Did you know that stress can trigger seizures in some individuals? Research shows
A recent study in the Radiation Oncology journal found that 13% of patients died within 30 days after getting palliative radiotherapy for bone metastases. Another

Choosing to have a carotid endarterectomy is a big decision. It’s important to know what to expect during recovery. Did you know that almost 100,000

Finding a lump inside your cheek can be scary. But knowing what it might be and when to see a doctor can help. At Liv
When serious bone damage happens, like from fractures or disease, our body might not heal on its own. That’s when a bone graft operation is

Cadaver bone grafts have changed orthopedic surgery a lot. They help patients who need bone replacement because of injuries, diseases, or surgery problems. Johns Hopkins

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)