Explore the various ways neurological disorders are managed. From medication to physical rehabilitation, find out who needs treatment and the costs involved.
We're Here to Help.
Get in Touch.
Send us all your questions or requests, and our expert team will assist you.
Neurological Treatment and Rehabilitation: Restoring Function
In the past, a neurological diagnosis often came with a limited prognosis. Today, the landscape of neurological treatment has shifted dramatically from “supportive care” to active recovery and functional restoration. At Liv Hospital, we do not view brain and nerve damage as static; we see a system with the potential to heal and rewire.
Our approach combines acute medical intervention (stopping the damage) with next-generation rehabilitation technology (retraining the brain). For international patients, this means access to therapies—such as robotic exoskeletons and comprehensive stroke protocols—that may be difficult to access or prohibitively expensive in their home countries.
How Do We Treat Acute Neurological Disorders?

The first phase of treatment is stabilization and damage control. Our Neurology Department works 24/7 to manage acute crises using international protocols.
- Stroke Intervention (Thrombectomy): For ischemic strokes, “clot-busting” drugs (tPA) are just the beginning. Liv Hospital’s neuro-interventionalists perform Mechanical Thrombectomy, threading a catheter into the brain to physically remove the clot. This procedure can save brain tissue even up to 24 hours after symptom onset in selected patients.
- Seizure Management: For epilepsy that resists standard medication, we utilize Vagus Nerve Stimulation (VNS) and advanced pharmacotherapy mapping to stabilize electrical activity without severe side effects.
- Autoimmune Protocols: For conditions like Multiple Sclerosis (MS) or Myasthenia Gravis, we utilize plasmapheresis (plasma exchange) and the latest monoclonal antibody therapies to halt the immune system’s attack on the nerves.
Advanced Interventional Therapies for Pain and Tremor

When medication alone is insufficient, we bridge the gap between neurology and surgery with minimally invasive interventions.
- Botox® for Chronic Migraine: For patients suffering from 15+ headache days a month, we follow a specialized injection protocol (the PREEMPT protocol). By injecting botulinum toxin into specific sites around the head and neck, we can block pain transmission for up to 3 months.
- Occipital Nerve Blocks (GON Block): A rapid-relief option for severe cluster headaches and migraines, delivering anesthetic directly to the major nerve at the base of the skull.
- Deep Brain Stimulation (DBS) Management: While the electrode implantation is surgical, the “programming” of the device is a fine art managed by our neurologists. We adjust the electrical impulses to silence tremors in Parkinson’s disease and Essential Tremor, allowing patients to reduce their medication dosage significantly.
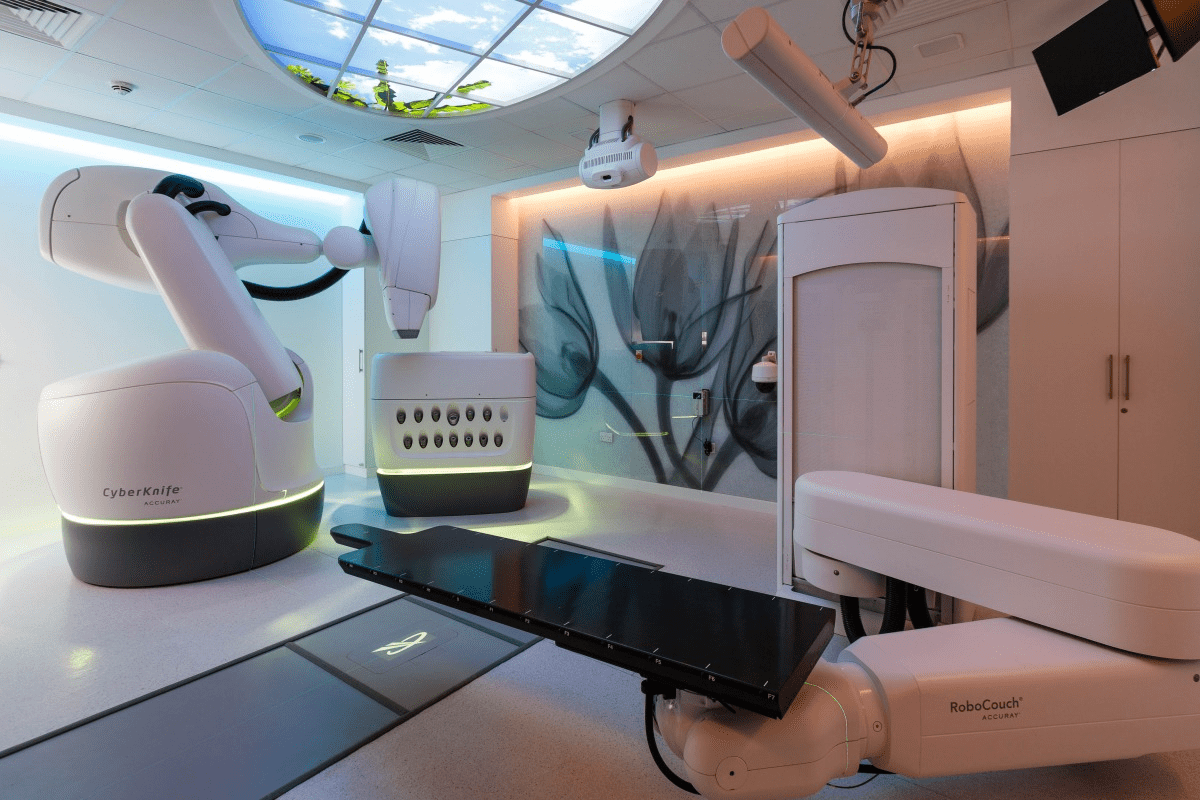
The Power of Robotic Rehabilitation
Rehabilitation is no longer just about “exercise”; it is about hacking the brain’s neuroplasticity. Liv Hospital is one of the few centers in the region equipped with a full suite of Robotic Rehabilitation tools designed to help patients walk and move again.
- Lokomat® (Walking Robot): This robotic exoskeleton attaches to the patient’s legs while they are suspended over a treadmill. It forces the legs into a perfect walking pattern, sending signals back to the spinal cord and brain to “remind” them how to walk. It is critical for stroke and spinal cord injury recovery.
- Armeo® (Arm & Shoulder Robot): A robotic arm support that gamifies therapy. Patients play video games using their impaired arm, which detects even the tiniest muscle activation and amplifies it, rebuilding neural pathways through thousands of repetitions.
- Cyberdyne HAL: A wearable cyborg-type suit that detects faint bio-electric signals on the skin surface to assist voluntary movement, bridging the gap between intention and action.
Regenerative Medicine: The Future of Neurology
Liv Hospital is a pioneer in the regulated application of Regenerative Medicine for neurological conditions. Our GMP-standards Stem Cell Production Center allows us to offer cellular therapies for conditions that have limited conventional options.
- Stem Cell Therapy: We evaluate suitable candidates (such as those with Cerebral Palsy or certain degenerative conditions) for mesenchymal stem cell applications aimed at reducing inflammation and promoting neural repair.
- Note: Candidates are selected through a rigorous ethical and medical review by our Scientific Council.
The "Return to Life" Program for International Patients
We understand that traveling for neurological care is a major decision. Our treatment plans are designed to be intensive and efficient to maximize your time in Turkey.
- Arrival & Assessment: Day 1 includes 3 Tesla MRI, lab work, and a physical assessment by the rehabilitation board.
- Intensive Therapy Block: Patients typically engage in 3–5 hours of therapy daily, combining robotic sessions, hydrotherapy, and manual physiotherapy.
- Family Training: We train caregivers on how to assist with transfers, exercises, and medication management before you return home.
- Discharge & Digital Follow-up: You leave with a digital copy of your records and a 6-month video follow-up schedule.

Lifestyle Modifications as Treatment
Lifestyle modification is a powerful form of treatment that complements medical interventions. For many conditions, changing daily habits is as effective as medication in preventing recurrence and managing symptoms.
Effective modifications include:
- Adopting heart healthy diets to prevent stroke
- Identifying and avoiding migraine triggers
- Maintaining regular sleep schedules for epilepsy
- engaging in mental stimulation for cognitive health
Surgical Interventions and Referrals
While neurologists do not perform surgery, they recognize when it is the best option and refer patients to neurosurgeons. They act as a bridge ensuring patients get the physical interventions they need when medicine is not enough.
Surgical options include:
- Deep Brain Stimulation for Parkinson’s disease
- Surgery to remove seizure focal points in epilepsy
- Procedures to remove blood clots in stroke
- Spinal surgeries to relieve nerve compression
Emerging Therapies and Research
Neurology is a rapidly advancing field with constant research into new therapies offering hope for previously untreatable conditions. Clinical trials and new technologies are expanding the toolkit available to doctors.
Areas of innovation include:
- Gene therapies for inherited disorders
- Immunotherapies for autoimmune conditions
- Neuroprotective agents for degenerative diseases
- Stem cell research for nerve regeneration
The Cost of Neurological Care
The cost of neurological care varies significantly depending on location and complexity but is generally considered a high cost specialty. This is due to the need for advanced imaging technology and long term chronic management.
Cost factors include:
- Consultation fees ranging widely globally
- High costs for diagnostic scans like MRI
- Ongoing expenses for specialized medications
- Medical tourism options offering lower costs in some regions
30 Years of Excellence
Trusted Worldwide
With patients from across the globe, we bring over three decades of medical
Book a Free Certified Online
Doctor Consultation

Reviews from 9,651
4,9
Worth a look
Was this article helpful?
We're Here to Help.
Get in Touch.
Send us all your questions or requests, and our expert team will assist you.
FREQUENTLY ASKED QUESTIONS
Can physical therapy really help the brain heal?
Physical therapy cannot reverse the brain damage but it retrains the brain and body allowing patients to regain significant function and independence.
Are neurological medications safe
All medications have side effects but neurologists carefully balance the risks and benefits monitoring patients closely to ensure safety.
How long does rehabilitation take
Rehabilitation is different for everyone it can take weeks months or even be a lifelong process of maintenance depending on severity.
Is surgery always an option for epilepsy
No surgery is only an option for specific types of epilepsy where the seizures originate from a single area that can be safely removed.
What is deep brain stimulation?
It is like a pacemaker for the brain where implanted electrodes send electrical impulses to control abnormal movements in Parkinson’s.

RELATED NEWS
Can Stress Cause Seizures: Amazing Relief
Can Stress Cause Epilepsy? Understanding the Connection Between Stress and Seizures <image1> Did you know that stress can trigger seizures in some individuals? Research shows
Crucial Life Expectancy: Side Effects of 5-Day Radiation
A recent study in the Radiation Oncology journal found that 13% of patients died within 30 days after getting palliative radiotherapy for bone metastases. Another

Pictures of Scars from Carotid Artery Surgery
Choosing to have a carotid endarterectomy is a big decision. It’s important to know what to expect during recovery. Did you know that almost 100,000

What Causes A Lump Inside Of Cheek In Mouth And When To Worry?
Finding a lump inside your cheek can be scary. But knowing what it might be and when to see a doctor can help. At Liv
How To Get A Bone Graft Operation: Complete Guide
When serious bone damage happens, like from fractures or disease, our body might not heal on its own. That’s when a bone graft operation is

How To Use Cadaver Bone Grafts For Bone Replacement Graft
Cadaver bone grafts have changed orthopedic surgery a lot. They help patients who need bone replacement because of injuries, diseases, or surgery problems. Johns Hopkins




