Rheumatology treats musculoskeletal and autoimmune diseases, including arthritis, lupus, gout, and vasculitis.
Send us all your questions or requests, and our expert team will assist you.
Rheumatology is a Sherlock Holmes-style specialty. There is rarely a single test that confirms a diagnosis; instead, rheumatologists rely on clinical criteria a combination of symptoms, physical findings, and test results. At Liv Hospital, we utilize comprehensive immunological panels and high-resolution imaging to catch these diseases in their earliest, most treatable phases.

The rheumatologist performs a specialized exam:
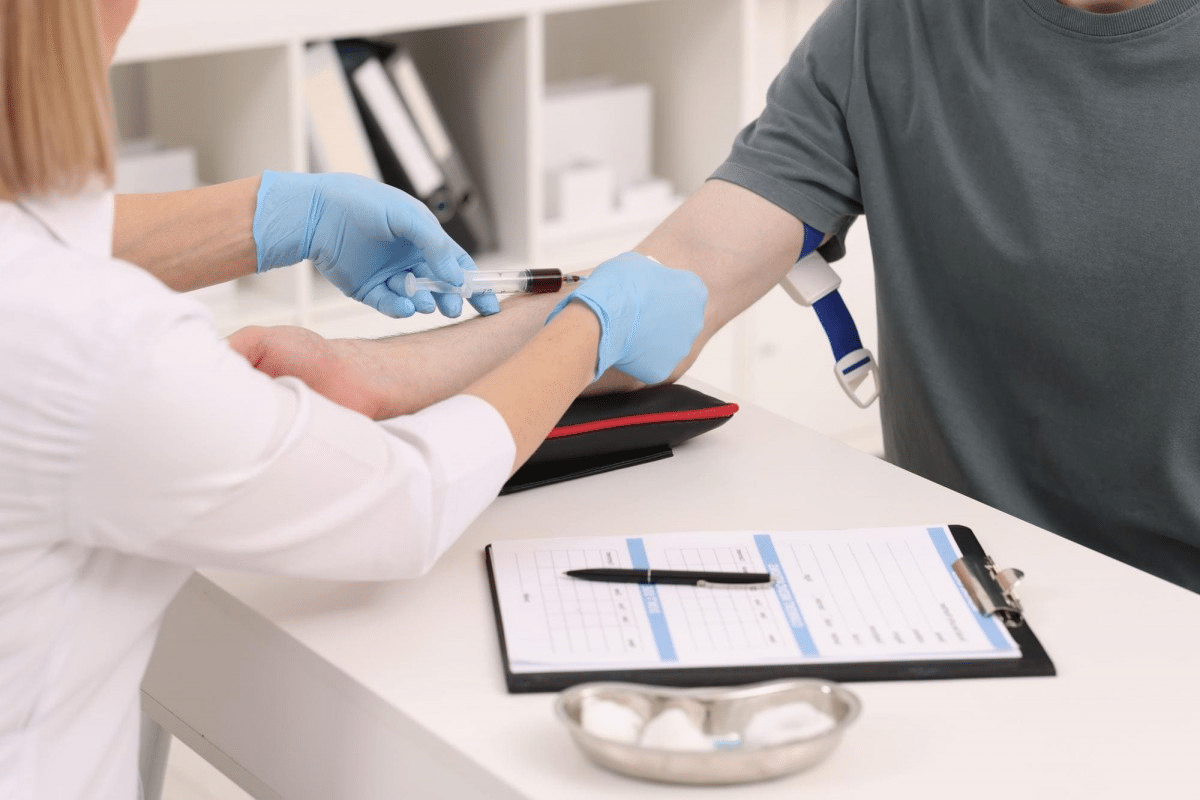
Blood tests look for markers of inflammation and specific autoantibodies.

Rheumatologists use scoring systems to “stage” disease activity and monitor treatment success.
Send us all your questions or requests, and our expert team will assist you.
Yes. While diet cannot “cure” these conditions, it supports management.
“Treat to Target” is the modern philosophy of rheumatology care. Instead of just managing symptoms, the doctor and patient set a specific goal usually remission (no symptoms) or low disease activity. Medication is adjusted aggressively and frequently until that specific target is reached to prevent long-term damage.
Not necessarily. Rheumatology is a “Sherlock Holmes-style” specialty because diagnosis relies on clinical criteria—a combination of symptoms and physical findings—rather than a single test. In early stages, X-rays may appear normal, and some patients have “seronegative” conditions where typical markers don’t show up in blood work. This is why specialized exams like Musculoskeletal Ultrasound are used to find inflammation that tests might miss.
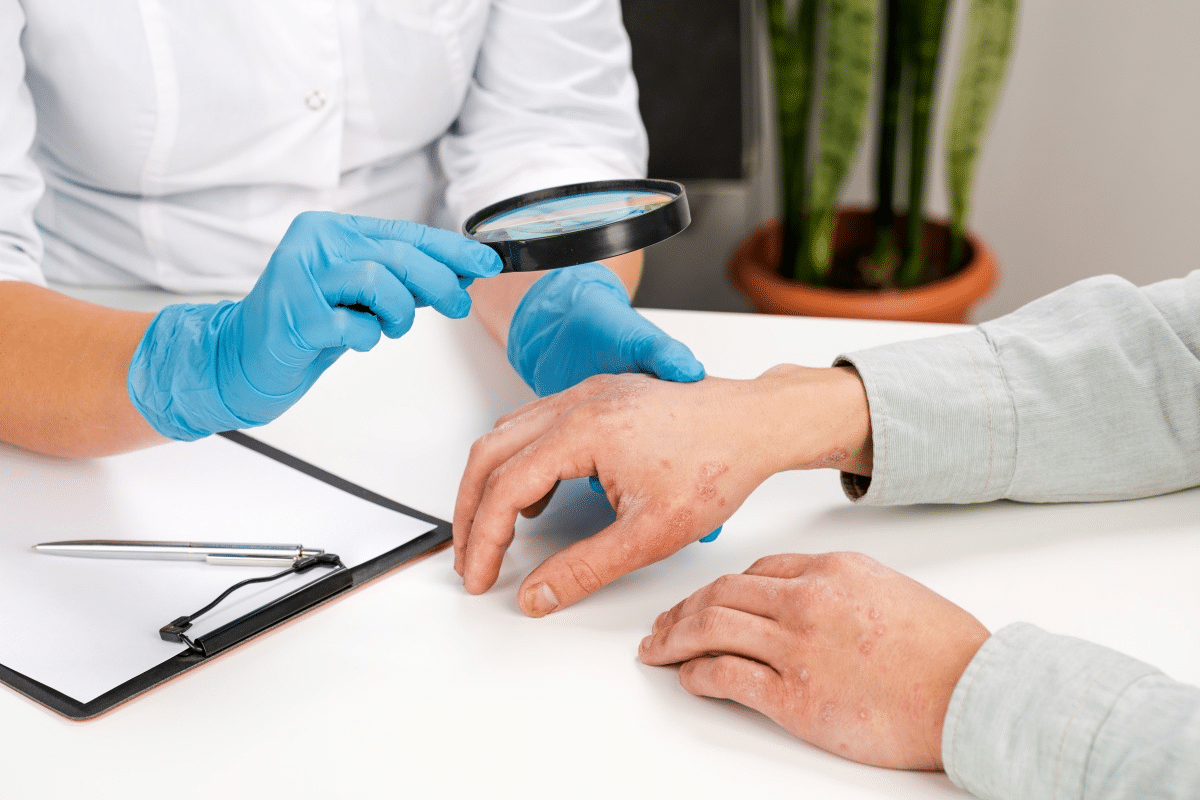
Many rheumatic diseases affect more than just the joints. For example, nail pitting can be a sign of psoriasis (linked to Psoriatic Arthritis), and skin tightening is a key indicator of Scleroderma. Examining these areas helps the doctor see the full picture of a systemic autoimmune condition.


Osteoporosis is a bone disease that affects millions. It makes bones weak, raising the risk of fractures. Bisphosphonate treatment is a key way to fight
Rheumatoid arthritis (RA) is a chronic condition that leads to progressive joint damage and deformity. At Liv Hospital, we focus on understanding RA’s progressive nature.
Explaining how do doctors check for arthritis using a combination of physical exams, patient history, and blood tests. Rheumatoid arthritis can be hard to spot
For decades, lupus has been a mystery to many, affecting millions globally. New research has found a key part of its puzzle: an imbalance of

Systemic lupus erythematosus (SLE) is a complex autoimmune disease. It can lead to life-threatening complications. About 10-15% of people with lupus die early because of

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)