Infectious diseases specialists diagnose and treat infections from bacteria, viruses, fungi, and parasites, focusing on fevers, antibiotics, and vaccines.
Send us all your questions or requests, and our expert team will assist you.
Diagnosing Hepatitis A requires a synthesis of clinical observation, epidemiological history, and precise laboratory investigation. Because the initial presentation mimics many other acute viral illnesses, the clinician relies on specific cues to refine the differential diagnosis. The medical history is the first step, where the physician evaluates the timeline of symptoms, looking for the classic progression from a flu-like prodrome to the onset of jaundice.
Crucially, the epidemiological context often provides the strongest leads. Clinicians investigate recent travel history to regions with intermediate or high endemicity, potential exposure to known outbreaks, and consumption of high-risk foods such as raw shellfish or unwashed produce. Social history is also relevant; inquiries regarding household contacts, sexual practices, and occupational environments (such as food service or healthcare) help assess risk. The assessment also involves a review of the patient’s vaccination status; a documented complete vaccination series renders a diagnosis of acute Hepatitis A highly improbable, prompting the search for alternative etiologies.
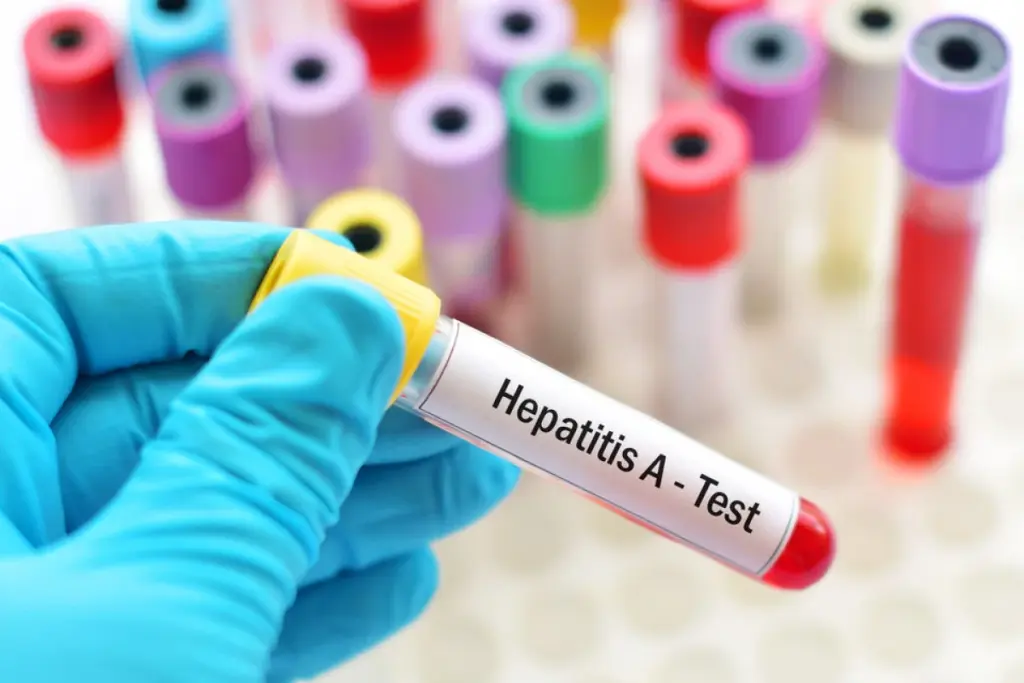
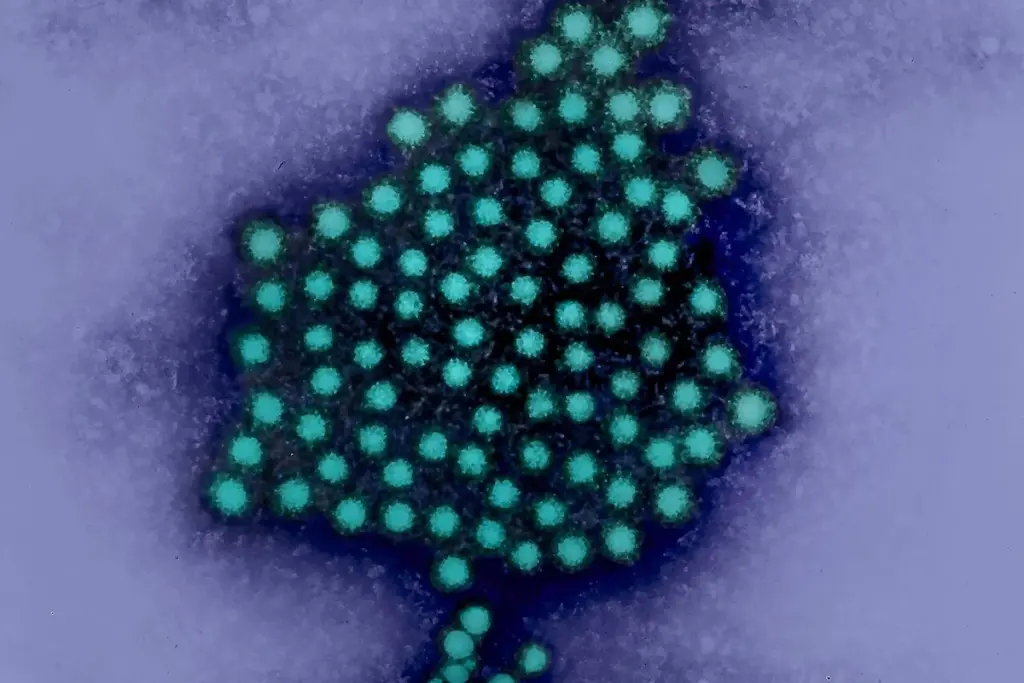
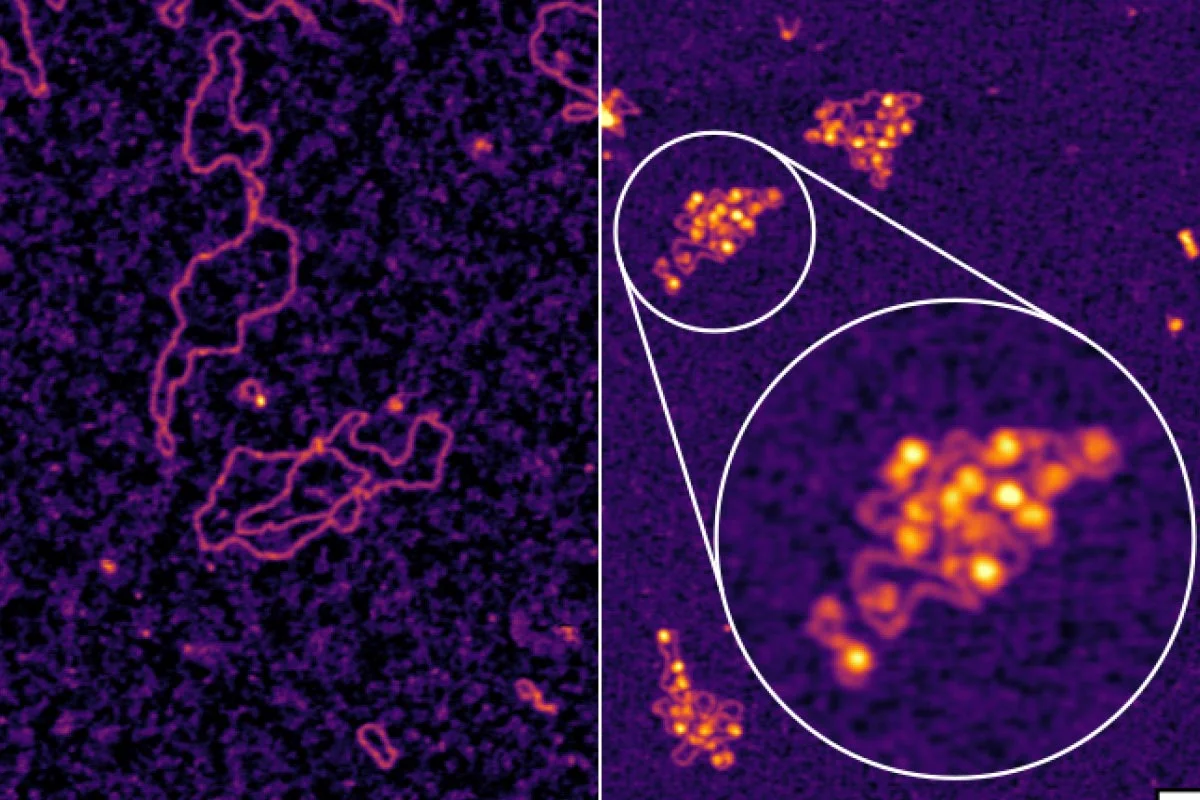
While clinical suspicion may be high, the definitive diagnosis of Hepatitis A is purely serological. The human immune system responds to the virus by producing specific antibodies, which can detect and differentiate acute infection from past exposure.

To assess the severity of the hepatic injury, a comprehensive Liver Function Test (LFT) panel is utilized. These biochemical markers provide a quantitative measure of liver cell damage and functional impairment.
The diagnostic process involves ruling out other conditions that present with acute liver injury. The clinician must distinguish Hepatitis A from:
In the rare event of severe or fulminant hepatitis, the evaluation shifts to intensive monitoring of organ failure. Frequent assessment of coagulation parameters (INR), electrolytes, renal function (creatinine), and mental status (for hepatic encephalopathy) becomes mandatory. In these scenarios, the diagnostic focus expands to determining the prognosis and the potential necessity for liver transplantation. Imaging modalities such as CT scans may be used to assess liver volume and exclude other abdominal pathologies in critically ill patients.

A confirmed diagnosis of Hepatitis A triggers a public health protocol. Laboratories and clinicians are typically mandated to report cases to local health authorities. This initiates contact tracing and surveillance procedures to identify the source of the infection (e.g., a specific restaurant or food product) and to offer post-exposure prophylaxis to close contacts, thereby preventing wider community outbreaks.
Send us all your questions or requests, and our expert team will assist you.
A positive IgM antibody test indicates that a person has a recent or current infection with Hepatitis A. IgM antibodies are the body’s first response to the virus. If this test is positive, it confirms that the Hepatitis A virus causes the patient’s symptoms.
A positive IgG antibody test means that a person is immune to Hepatitis A. This immunity could result from a past infection from which they have recovered, or from successful vaccination. A positive IgG result (with a negative IgM result) means the person is protected and does not have the active disease.
An abdominal ultrasound is performed to rule out other causes of liver pain and jaundice. While it cannot diagnose Hepatitis A directly, it helps doctors rule out gallstones blocking the bile ducts or other structural problems in the liver or gallbladder.
No. The symptoms of Hepatitis A—such as fever, nausea, and jaundice—are very similar to those of other liver diseases, including Hepatitis B, Hepatitis C, and drug-induced liver injury. Specific blood tests to detect antibodies to the virus are the only way to confirm the diagnosis accurately.
The liver produces proteins that help the blood to clot. In severe Hepatitis A, the liver may become so damaged that it stops making these proteins efficiently. Doctors monitor blood clotting tests (like PT/INR) to assess liver function; if the blood takes too long to clot, it is a warning sign of potential liver failure.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)