Last Updated on November 26, 2025 by Bilal Hasdemir

This article will give you a full look at the main causes of prostate problems. It will help you understand the risks and how to deal with them.
Key Takeaways
- Prostate problems are common among men over 50.
- Aging, hormonal changes, and lifestyle factors contribute to prostate issues.
- Understanding risk factors is key to maintaining prostate health.
- Early detection and prevention are critical for managing prostate problems.
- Lifestyle changes can help reduce some prostate health risks.
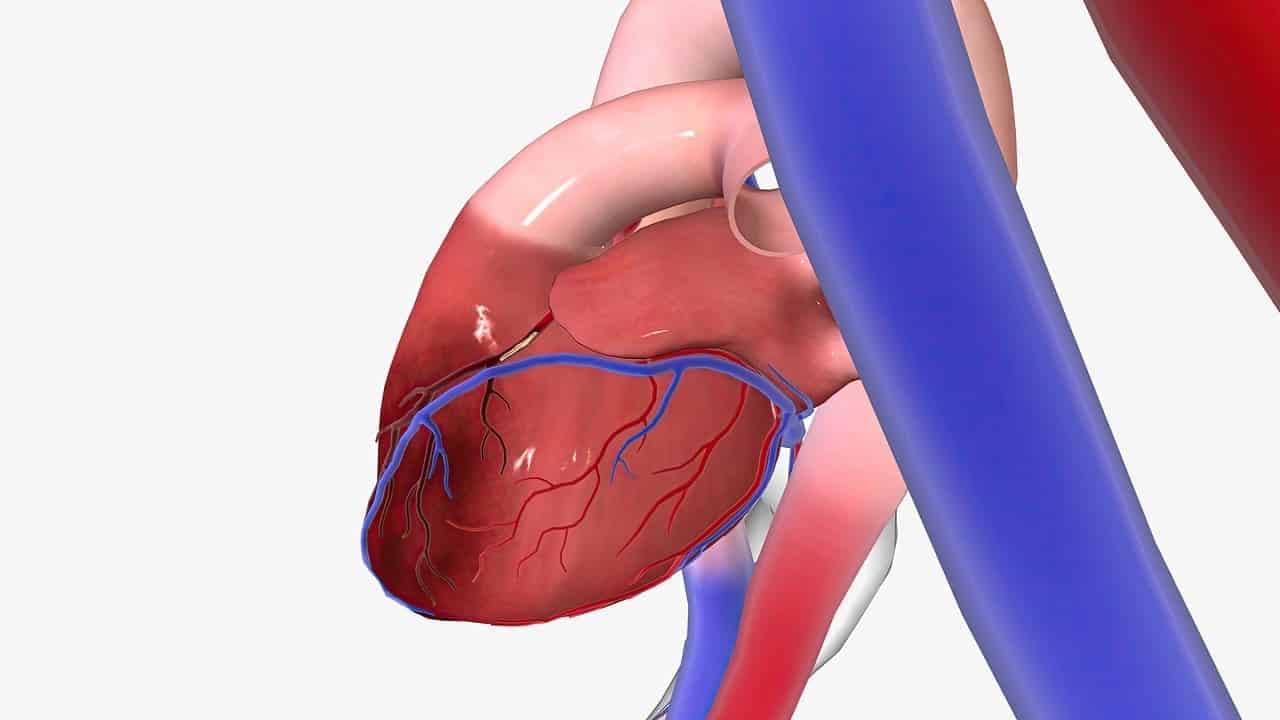
The Prostate Gland: Structure and Function
It’s important to know about the prostate gland’s structure and function. This small, walnut-sized organ is below the bladder and in front of the rectum. It plays a key role in the male reproductive system.
Anatomy and Location of the Prostate
The prostate gland is in a specific spot in the male pelvis. It surrounds the urethra, which carries urine out of the body. Any changes in the prostate can affect how we urinate.
The prostate has glandular tissue, fibrous tissue, and smooth muscle. The glandular tissue makes prostatic fluid, a big part of semen. This fluid is full of nutrients and proteins that help sperm.
The Prostate’s Role in Male Reproductive Health
The prostate gland is key in making semen. Semen is a mix of fluids from different parts of the male body. The prostate’s fluid gives sperm the nutrients they need to survive and move.
“The prostate’s secretions are essential for maintaining the viability of sperm, thereof playing a critical role in fertility.”
When a man ejaculates, the prostate gland contracts. It releases its fluids into the urethra. This is important for sperm to be nourished and move well.
Normal Changes Throughout a Man’s Lifetime
The prostate gland changes a lot over a man’s life. It starts to grow during puberty because of male hormones. As men get older, the prostate’s size and function can change.
| Age Group | Prostate Changes | Potential Impact |
| Puberty to Early Adulthood | Growth under hormonal influence | Development of reproductive capability |
| Middle Age to Older Age | Potential enlargement (BPH) | Urinary symptoms, possible impact on quality of life |
As men get older, they face higher risks of prostate problems like BPH and cancer. Knowing about these changes helps keep the prostate healthy and deal with any issues.
Overview of Common Prostate Conditions

Many conditions can affect the prostate, from non-cancerous growths to cancer. Knowing about these is key to keeping the prostate healthy. It helps spot problems early.
Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia, or BPH, is a non-cancerous growth of the prostate. It’s common in older men, causing trouble with urination. Symptoms include weak urine flow and needing to urinate often.
The exact reason for BPH isn’t known. But, it’s thought to be linked to hormonal changes that happen as men get older.
Prostatitis: Acute and Chronic Forms
Prostatitis is inflammation of the prostate gland. It can be caused by infection or other factors. There are acute and chronic forms of prostatitis.
Acute prostatitis is usually due to a bacterial infection. It can cause severe symptoms like pain, fever, and trouble urinating. Chronic prostatitis may not have a clear cause. It can last a long time, causing ongoing discomfort and urinary problems.
Prostate Cancer: Types and Prevalence
Prostate cancer is a common cancer in men, mainly in older ages. There are different types, with adenocarcinoma being the most common. Risk factors include age, family history, and genetics.
Early detection through screening is key for effective treatment. It helps manage prostate cancer well.
Prostatic Intraepithelial Neoplasia (PIN)
Prostatic Intraepithelial Neoplasia, or PIN, is abnormal cell growth in the prostate. It’s considered precancerous. PIN is found during biopsies and is divided into low-grade and high-grade.
High-grade PIN increases the risk of prostate cancer. So, it’s important to keep an eye on it.
Age as the Primary Risk Factor
We know that age is a big factor in prostate health problems. As men get older, the chance of prostate issues grows. We’ll look at how aging affects the prostate, the cell changes, and the link between age and prostate diseases.
Prostate Changes in Men Over 40
Men over 40 often see changes in their prostate. This can include a bigger prostate, known as BPH, causing urinary problems. BPH and other prostate issues get more common with age, making it a big health worry for older men.
Age-Related Cellular Mechanisms
Aging changes the prostate at the cell level, leading to possible problems. Hormone changes, like testosterone turning into DHT, are key in prostate growth and age-related issues.
Statistical Correlation Between Age and Prostate Disorders
There’s a clear link between aging and prostate diseases. The table below shows how BPH and prostate cancer rates change with age.
| Age Group | Prevalence of BPH | Prevalence of Prostate Cancer |
| 40-49 | 20% | 0.5% |
| 50-59 | 40% | 2% |
| 60-69 | 60% | 5% |
| 70+ | 80% | 10% |
It’s important to understand how age affects prostate health. Early detection and management of prostate issues are key. Regular check-ups and knowing the risks of aging can help men keep their prostate healthy.
Hormonal Influences on Prostate Health

Hormones, like testosterone and its derivatives, greatly affect prostate health. The prostate gland is very sensitive to these changes. This sensitivity can cause issues such as benign prostatic hyperplasia (BPH) and prostate cancer.
Testosterone and Dihydrotestosterone (DHT) Effects
Testosterone is a key male hormone that impacts prostate health. It turns into dihydrotestosterone (DHT) through an enzyme called 5-alpha-reductase. DHT is stronger than testosterone and linked to prostate problems.
Studies show that high DHT levels raise the risk of BPH and prostate cancer. The relationship between testosterone and DHT with the prostate is complex. While they’re vital for prostate function, too much can cause growth and possibly cancer.
Hormonal Imbalances and Prostate Growth
Too much DHT can cause prostate enlargement, known as BPH. This is common in older men. It leads to symptoms like frequent urination and weak flow.
As men age, hormonal changes affect prostate health. Lower testosterone levels can increase the risk of prostate issues.
Androgen Receptors and Their Role
Androgen receptors are key in how testosterone and DHT affect the prostate. These receptors are proteins in prostate cells that bind to androgens. This interaction is vital for prostate health but can lead to disease if not balanced.
“The androgen receptor is a key regulator of prostate cell growth and survival, and its dysregulation is implicated in the development of prostate cancer.”
Understanding androgen receptors and their interaction with hormones is vital. It helps in finding effective treatments for prostate issues.
Genetic Predisposition and Family History
Research shows that genetics and family history play big roles in prostate health. Knowing these factors can help spot who’s at higher risk. This knowledge guides how to prevent problems.
Hereditary Risk Patterns
Men with a family history of prostate cancer face a higher risk. The risk grows with more relatives affected and their age at diagnosis. We’ll look into the hereditary patterns that raise this risk.
Key Hereditary Factors:
- First-degree relatives (father or brother) with prostate cancer
- Multiple family members affected across generations
- Early onset of prostate cancer in family members
Specific Genetic Markers for Prostate Cancer
Some genetic markers up the risk of prostate cancer. These include BRCA1 and BRCA2 gene mutations and other genetic changes. We’ll talk about these markers and their role in risk assessment.
| Genetic Marker | Description | Risk Implication |
| BRCA1 | Tumor suppressor gene | Increased risk of prostate and breast cancer |
| BRCA2 | Tumor suppressor gene | Higher risk of prostate, breast, and ovarian cancer |
| HOXB13 | Homeobox gene | Associated with early-onset prostate cancer |
Family History as a Predictive Factor
A family history of prostate cancer is a strong risk factor. Men with a first-degree relative with prostate cancer are at higher risk. This risk grows with more relatives affected. We’ll see how family history guides doctors in clinical practice.
Understanding genetics and family history helps doctors assess risk better. They can then suggest the right screening and prevention steps.
The Main Causes of Prostate Problems
Prostate problems in men come from many sources. These include physical, lifestyle, and genetic factors. Knowing these causes is key to preventing and treating prostate issues.
Primary Physiological Factors
Physical factors are a big part of prostate problems. These include:
- Age: The risk of prostate issues goes up after 40.
- Hormonal Changes: Hormone levels, like testosterone and DHT, can impact prostate health.
- Genetic Predisposition: Family history and genetics can make men more likely to have prostate problems.
Interplay Between Multiple Causative Elements
Prostate problems often come from a mix of factors. For example:
- Lifestyle choices, like diet and exercise, can affect prostate health.
- Genetics can work with environmental factors to raise prostate risk.
- Hormonal imbalances can get worse with obesity and metabolic syndrome.
Root Causes vs. Contributing Factors
It’s important to know the difference between root causes and contributing factors. Root causes directly lead to prostate issues, like genetic mutations or hormonal imbalances. Contributing factors, like lifestyle choices or environmental exposures, can make problems worse in people who are already at risk.
Understanding prostate problem causes helps doctors create better treatment plans. By tackling both root causes and contributing factors, men can lower their risk of prostate issues. This improves their overall health.
Lifestyle Factors Affecting Prostate Health
Keeping a healthy lifestyle is key for prostate health. Our daily habits and choices greatly affect our well-being, including our prostate.
Dietary Patterns and Nutritional Impact
Eating a balanced diet with fruits, vegetables, and whole grains is good for the prostate. Foods high in antioxidants, like tomatoes, and omega-3 fatty acids in fish, can lower prostate risks. It’s wise to eat less processed meats and foods with lots of saturated fats.
- Eat a variety of colorful fruits and vegetables.
- Choose whole grains over refined ones.
- Eat less processed and red meats.
Physical Inactivity and Sedentary Behavior
Being active is good for health and prostate health. Sedentary behavior increases prostate risks, like BPH. Doing moderate exercise, like brisk walking, for 30 minutes a day can help.
- Do at least 150 minutes of moderate exercise weekly.
- Add strength training to your routine.
- Try to sit less.
Smoking, Alcohol, and Substance Use
Smoking and too much alcohol harm prostate health. Smoking raises prostate cancer risk, and too much alcohol causes health issues. Cutting down on alcohol and quitting smoking is important for prostate health.
- Quit smoking or don’t start.
- Drink alcohol in moderation.
- Avoid illegal substances.
Stress and Sleep Quality
Chronic stress and poor sleep hurt health, including prostate health. Stress management techniques, like meditation, can help. Good sleep habits, like a regular sleep schedule, are also key.
- Do stress-reducing activities often.
- Keep a regular sleep schedule.
- Make your sleep area restful.
By choosing wisely, men can support their prostate health and overall well-being.
Obesity, Metabolic Syndrome, and Inflammation
The connection between obesity, metabolic syndrome, and prostate health is clear. Metabolic health is key to avoiding prostate problems.
Body Weight and Prostate Health Connection
Studies show a strong link between body weight and prostate health. Obesity raises the risk of prostate cancer and aggressive forms. This is due to inflammation and hormonal imbalances from excess fat.
Keeping a healthy weight is vital for prostate health. Men with higher BMIs face more prostate issues. This shows the need for weight management.
Metabolic Disorders and BPH Development
Metabolic syndrome increases the risk of Benign Prostatic Hyperplasia (BPH). It includes high blood pressure, high blood sugar, and abnormal lipids. The causes are complex, involving insulin resistance, inflammation, and hormonal changes.
Men with metabolic syndrome often face BPH symptoms like frequent urination. Managing metabolic health can reduce these risks.
Chronic Inflammation Pathways
Chronic inflammation is a major factor in prostate issues like prostatitis and cancer. Obesity and metabolic syndrome cause chronic inflammation, affecting prostate health.
Understanding chronic inflammation can lead to new treatments. Lifestyle changes like diet and exercise are key to reducing inflammation and keeping the prostate healthy.
Insulin Resistance and Hormonal Effects
Insulin resistance, a sign of metabolic syndrome, affects hormone levels. It increases dihydrotestosterone (DHT), leading to prostate growth and BPH.
Improving insulin sensitivity through diet, exercise, and medication can help. This reduces hormonal effects that harm the prostate.
Infections and Inflammatory Triggers
Prostatitis is an inflammation of the prostate gland. It can be caused by different infections. We will look at how these infections affect prostate health and lead to various forms of prostatitis.
Bacterial Infections Leading to Acute Prostatitis
Acute prostatitis often comes from bacterial infections. Escherichia coli is a common cause. We will talk about how to treat these infections and why quick medical help is important.
| Bacteria Type | Common Symptoms | Treatment Approach |
| Escherichia coli | Painful urination, fever | Antibiotics |
| Klebsiella | Urinary tract pain, chills | Antibiotics, supportive care |
Chronic Bacterial and Non-bacterial Prostatitis
Chronic prostatitis can be caused by ongoing bacterial infections or non-bacterial factors. We will look at the differences between these two types and their treatment options.
Chronic bacterial prostatitis involves recurring bacterial infections. Non-bacterial prostatitis, or chronic pelvic pain syndrome, causes pain without bacterial infection signs.
Sexually Transmitted Infections and Prostate Health
STIs can harm prostate health. We will discuss how STIs like chlamydia and gonorrhea can cause prostatitis. We will also talk about how to prevent these infections.
Practicing safe sex and getting regular STI tests are key to prostate health. People at risk should talk to their healthcare providers for advice.
Urinary Tract Infections and Ascending Bacteria
UTIs can lead to bacteria affecting the prostate. We will explore the link between UTIs and prostatitis. We will also discuss how to stop bacteria from moving up.
Treating UTIs quickly is vital to avoid prostatitis. If UTI symptoms don’t go away, seek medical help.
Understanding infections’ role in prostatitis helps us manage and prevent it. Effective treatment and prevention are essential for prostate health.
Racial and Ethnic Risk Factors in the United States
Racial and ethnic differences are key in prostate cancer risk and outcomes in the U.S. Prostate cancer affects men from many backgrounds. But, its impact varies across racial and ethnic groups.
Higher Incidence in African American Men
African American men face a higher risk of prostate cancer. Studies show they are often diagnosed younger and with more aggressive cancer. The reasons for this disparity are complex, involving genetics and environment.
Genetic vs. Socioeconomic Factors
The debate on prostate cancer disparities focuses on genetics versus socioeconomic factors. While genetics play a part, socioeconomic factors like healthcare access and lifestyle also matter. Understanding these factors is key to addressing disparities.
Disparities in Prostate Cancer Outcomes
There are also disparities in prostate cancer outcomes. African American men have higher incidence and mortality rates. To address these, we need better screening access, quality care, and awareness among high-risk groups.
Addressing racial and ethnic disparities in prostate cancer is complex. By understanding these differences and striving for equitable healthcare, we can improve outcomes for all men with prostate cancer.
Medical Conditions Linked to Prostate Issues
Prostate health is tied to overall health. Conditions like diabetes and heart disease play a big role. As we get older, the risk of prostate problems grows. Certain medical conditions can make this risk worse. We’ll look at how different health issues affect the prostate.
Diabetes and Prostate Health Correlation
Research shows diabetes and prostate health are closely linked. Men with diabetes face a higher risk of prostate issues, like BPH and cancer. The reasons are complex, involving insulin resistance, hormonal changes, and inflammation.
Managing diabetes is key for both overall health and prostate health. Making lifestyle changes, like diet and exercise, can help reduce these risks.
Cardiovascular Disease Connection
Cardiovascular disease and prostate health are connected. Heart disease can raise the risk of prostate problems. This is because of shared risk factors like smoking and obesity. Inflammation from heart disease can also worsen prostate conditions.
It’s important to manage heart disease risk to protect the prostate. A heart-healthy lifestyle, including a balanced diet and exercise, is essential. Avoiding tobacco products is also important.
Hypertension and Prostate Problems
Hypertension, or high blood pressure, is linked to prostate problems. The exact reasons are not clear, but it may cause prostate enlargement and inflammation. It’s vital to manage high blood pressure through lifestyle changes and, if needed, medication.
Autoimmune Conditions and Inflammation
Autoimmune conditions can cause chronic inflammation, affecting prostate health. Conditions like rheumatoid arthritis and lupus can raise the risk of prostatitis or worsen prostate issues. Understanding this link is important for treatment plans.
Managing autoimmune conditions requires a broad approach. This includes medication, lifestyle changes, and regular check-ups. By controlling inflammation and managing autoimmune diseases, we can protect prostate health.
Environmental Factors and Toxin Exposure
Exploring prostate issues, we see the big role of environmental toxins and chemicals. The world around us greatly affects our health. Studies show how important environmental factors are for prostate health.
Endocrine-Disrupting Chemicals
Endocrine-disrupting chemicals (EDCs) mess with our hormone system. They’re in plastics, pesticides, and some industrial chemicals. Research shows EDCs can harm prostate health by messing with our hormones. This might lead to BPH or prostate cancer.
Occupational Hazards and Chemical Exposure
Some jobs expose people to chemicals that raise prostate problem risks. For example, workers in pesticide or heavy metal industries face higher risks. Knowing the hazards and taking steps to prevent them is key.
Pesticides and Agricultural Compounds
Pesticides and agricultural compounds might harm prostate health. Studies link them to prostate cancer and other issues. These chemicals can damage cells or mess with hormones.
Heavy Metals and Industrial Pollutants
Heavy metals like cadmium and lead, and industrial pollutants, are being studied. They can build up in our bodies and harm prostate cells. Lowering exposure to these toxins is vital for prostate health.
In summary, environmental toxins and exposure are big factors in prostate health. Knowing these risks and reducing exposure can help prevent prostate problems.
Diagnostic Approaches and Treatment Options
Understanding how to diagnose and treat prostate problems is key. We’ll look at the latest ways to find prostate issues and the treatments for BPH, prostatitis, and prostate cancer.
Screening Methods for Prostate Problems
Screening for prostate issues often uses a few tests. The Prostate-Specific Antigen (PSA) test is a common first step. It checks for PSA levels in the blood. High levels might mean prostate problems, like cancer.
Another important test is the Digital Rectal Examination (DRE). A healthcare provider feels the prostate gland for any oddities.
Medical Interventions for BPH
Treating BPH depends on how bad the symptoms are. For mild cases, just watching and waiting might be advised. But for more serious symptoms, doctors might prescribe alpha-blockers or 5-alpha-reductase inhibitors.
In some cases, surgery like Transurethral Resection of the Prostate (TURP) is needed.
Treating Prostatitis: Acute vs. Chronic
Treating prostatitis changes based on if it’s acute or chronic. Acute bacterial prostatitis gets treated with antibiotics. Chronic prostatitis, which can be bacterial or non-bacterial, might need a longer antibiotic course or other treatments like alpha-blockers.
Prostate Cancer Treatment Approaches
Prostate cancer treatment varies a lot. It depends on the cancer’s stage, how aggressive it is, and the patient’s health. Treatment options range from active surveillance for low-risk cancers to surgery, radiation, and hormone therapy for more serious cases.
| Condition | Treatment Options |
| BPH | Watchful waiting, Alpha-blockers, 5-alpha-reductase inhibitors, TURP surgery |
| Acute Prostatitis | Antibiotics |
| Chronic Prostatitis | Antibiotics, Alpha-blockers, Pain relief medications |
| Prostate Cancer | Active surveillance, Surgery, Radiation therapy, Hormone therapy |
Knowing about these diagnostic methods and treatments is important for prostate health. Always talk to a healthcare professional to find the best treatment for you.
Preventive Strategies for Optimal Prostate Health
Keeping your prostate healthy starts with a proactive approach. This includes eating right, staying active, and getting regular check-ups. By doing these things, you can lower your risk of prostate problems and keep your prostate in top shape.
Dietary Recommendations for Prostate Health
Eating well is key to a healthy prostate. Include foods full of antioxidants like fruits and veggies to fight oxidative stress. Tomatoes, for example, are packed with lycopene, which may help prevent prostate cancer. Also, add healthy fats from nuts and olive oil to your diet for prostate support.
Try to eat less processed meats and dairy, as they can increase prostate risks. Instead, focus on whole grains, lean proteins, and a variety of colorful veggies. These foods give your prostate the nutrients it needs to stay healthy.
| Food Group | Recommended Foods | Benefits for Prostate Health |
| Fruits and Vegetables | Tomatoes, berries, cruciferous vegetables | Rich in antioxidants, lycopene, and other nutrients |
| Healthy Fats | Nuts, olive oil, fatty fish | Supports overall health and reduces inflammation |
| Whole Grains | Brown rice, quinoa, whole wheat bread | Provides fiber, vitamins, and minerals |
Exercise and Weight Management Guidelines
Regular exercise is vital for a healthy weight and lower prostate risks. Aim for 150 minutes of moderate exercise or 75 minutes of vigorous exercise weekly. Activities like brisk walking, cycling, or swimming can boost your health and prostate well-being.
Combining diet and exercise helps manage weight and prostate health. Talk to a healthcare expert to create a workout plan that fits your lifestyle and abilities.
Supplements and Natural Approaches
While a balanced diet is essential, some supplements can support prostate health. Saw palmetto, zinc, and omega-3 fatty acids have been studied for their benefits. Always consult a healthcare professional before adding supplements to your routine.
Natural methods like stress management and enough sleep are also important. They help keep your overall health in check and reduce prostate risks.
Regular Screening and Early Detection Benefits
Regular screenings are key to preventive prostate care. Early detection through tests like the PSA test can greatly improve treatment success. Discuss screening options and schedules with your healthcare provider based on your risk and health.
By following these preventive steps, men can actively work towards a healthy prostate and lower the risk of prostate issues.
Conclusion
It’s important to know about prostate problems and what affects prostate health. This article has covered many points, like age, hormones, genes, lifestyle, and the environment. These all play a part in prostate issues.
Knowing the main causes of prostate problems helps us take action. We can lower our risk by eating right, exercising, and avoiding bad substances. Regular check-ups and early detection are also key to managing prostate health.
Prostate health is influenced by many things, and we need a wide approach to tackle them. By understanding these factors and making healthy choices, men can lower their risk of prostate problems. We suggest talking to doctors to create a plan for good prostate health.
FAQ
What are the primary risk factors for developing prostate problems?
Main risk factors include age, family history, and genetics. Lifestyle choices like diet and exercise also matter. Certain health conditions, like obesity and diabetes, can increase risk too.
How does age affect prostate health?
Age is a big risk factor for prostate issues. The risk grows after 40 due to cell changes and hormone shifts.
Can lifestyle changes help prevent prostate issues?
Yes, a healthy diet, regular exercise, and managing weight help. Avoiding smoking and too much alcohol is also key.
What is the role of genetics in prostate health?
Genetics and family history are very important. Certain genes can raise the risk of prostate cancer and other issues.
How do hormonal imbalances affect the prostate?
Hormonal imbalances, like testosterone to DHT conversion, can cause prostate growth. This increases the risk of BPH.
What is the connection between obesity and prostate health?
Obesity is linked to higher risks of BPH and prostate cancer. This is due to chronic inflammation and metabolic issues.
Can infections and inflammatory conditions affect the prostate?
Yes, bacterial infections can cause acute prostatitis. Chronic inflammation can lead to prostatitis and even prostate cancer.
How do environmental factors impact prostate health?
Exposure to harmful chemicals, occupational hazards, pesticides, and heavy metals can harm the prostate.
What are the benefits of regular screening for prostate health?
Regular screening can catch problems early. This leads to better treatment outcomes for conditions like prostate cancer.
Are there any supplements or natural approaches that can support prostate health?
Some supplements and dietary changes might help. But, always talk to a healthcare professional before trying new supplements.
How do medical conditions like diabetes and cardiovascular disease affect prostate health?
Diabetes and heart disease can raise the risk of prostate problems. This is due to chronic inflammation and metabolic issues.
What are the differences in prostate cancer risk among different racial and ethnic groups?
African American men face a higher risk of prostate cancer. This is due to both genetic and socioeconomic factors.
Reference
- Cornford, P., van den Bergh, R. C. N., Briers, E., et al. (2021). EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer. European Urology, 79(2), 243-262. https://pubmed.ncbi.nlm.nih.gov/33696335/