Last Updated on November 26, 2025 by Bilal Hasdemir
Men with localized prostate cancer face a tough choice when reviewing prostate cancer treatment options: surgery or radiation therapy. A study found that about 70% of men choose surgery, while the rest might pick radiation or other treatment options. Deciding on the best treatment can feel overwhelming, so at this important time, it’s key to look at the good and bad of each treatment approach. We aim to clear up the best localized prostate cancer treatment options, guiding you to make a well-informed choice.
Key Takeaways
- It’s vital to understand prostate cancer and its treatment options.
- Surgery and radiation are the main treatment approaches for localized cases.
- The choice between surgery and radiation depends on many factors, like the cancer’s stage and the patient’s health.
- Talking to a healthcare professional about the best treatment options is essential.
- Choosing wisely can greatly affect the treatment outcome.
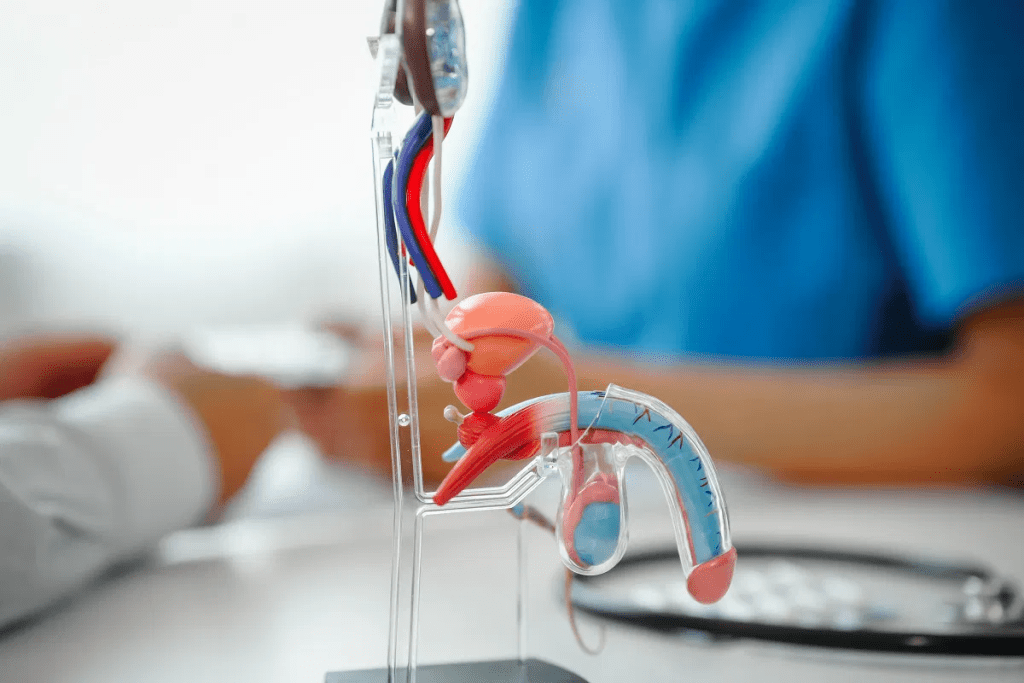
The Prostate Cancer Treatment Landscape
The world of prostate cancer treatment is complex. It’s shaped by many things, like how common the disease is and what each patient needs. Prostate cancer is a big deal for men in the U.S., affecting their health and life quality.
The Prevalence and Impact of Prostate Cancer in the United States
Many men in the U.S. get prostate cancer. The American Cancer Society says over 288,000 new cases will be diagnosed in 2023. This disease has a big impact on healthcare and the lives of those affected. Knowing about prostate cancer survival rates by treatment is key for making smart choices.
Because prostate cancer is so common, we need good ways to manage it. These include watching the disease closely, surgery, and radiation therapy. Each option is chosen based on the patient’s risk and health.
The Critical Importance of Treatment Selection
Choosing the right treatment for prostate cancer is very important. It can greatly affect how well a patient does. Prostate cancer treatment decision factors include the cancer’s stage and grade, the patient’s age and health, and what they prefer. Doctors from different fields often work together to decide the best course of action.
We stress the need to think about all the prostate cancer treatment decision factors when picking a treatment. By learning about the different prostate cancer management strategies, patients can make choices that fit their needs and wishes.
Current Statistics: Surgery vs. Radiation Treatment Choices

Choosing between surgery and radiation therapy for prostate cancer is complex. It depends on many factors. Looking at current statistics, we see that different things affect these choices.
National Trends in Prostate Cancer Treatment Selection
Over time, how we treat prostate cancer has changed. Both surgery and radiation therapy are common. Studies show that the choice depends on the cancer’s stage and the patient’s health.
Surgery, like radical prostatectomy, has been a key treatment for early prostate cancer. New surgical methods, like robotic-assisted surgery, have made it safer and faster. This makes it appealing to many.
Demographic Factors Influencing Treatment Choices
Demographic factors greatly affect the choice between surgery and radiation. Age, ethnicity, and income level are important.
- Younger patients often choose surgery to get rid of the cancer.
- Older patients or those with health problems might prefer radiation because it’s less invasive.
- Money and access to care also play a role in what treatment patients choose.
Regional Variations in Treatment Preferences
There are big differences in how prostate cancer is treated across different areas. Access to treatments varies, affecting patient choices.
Research shows that results can differ a lot in different places. This highlights the need for standard care guidelines. Knowing these differences helps doctors tailor care to their patients’ needs.
By looking at these trends and factors, we can understand the current state of prostate cancer treatment. This helps both patients and doctors make better choices.
Prostate Cancer Treatment Options: A CompleteOverview

It’s important to know all about prostate cancer treatment options. This knowledge helps in making the right choices for care. Today, treatments are more personalized, fitting each patient’s needs and wishes.
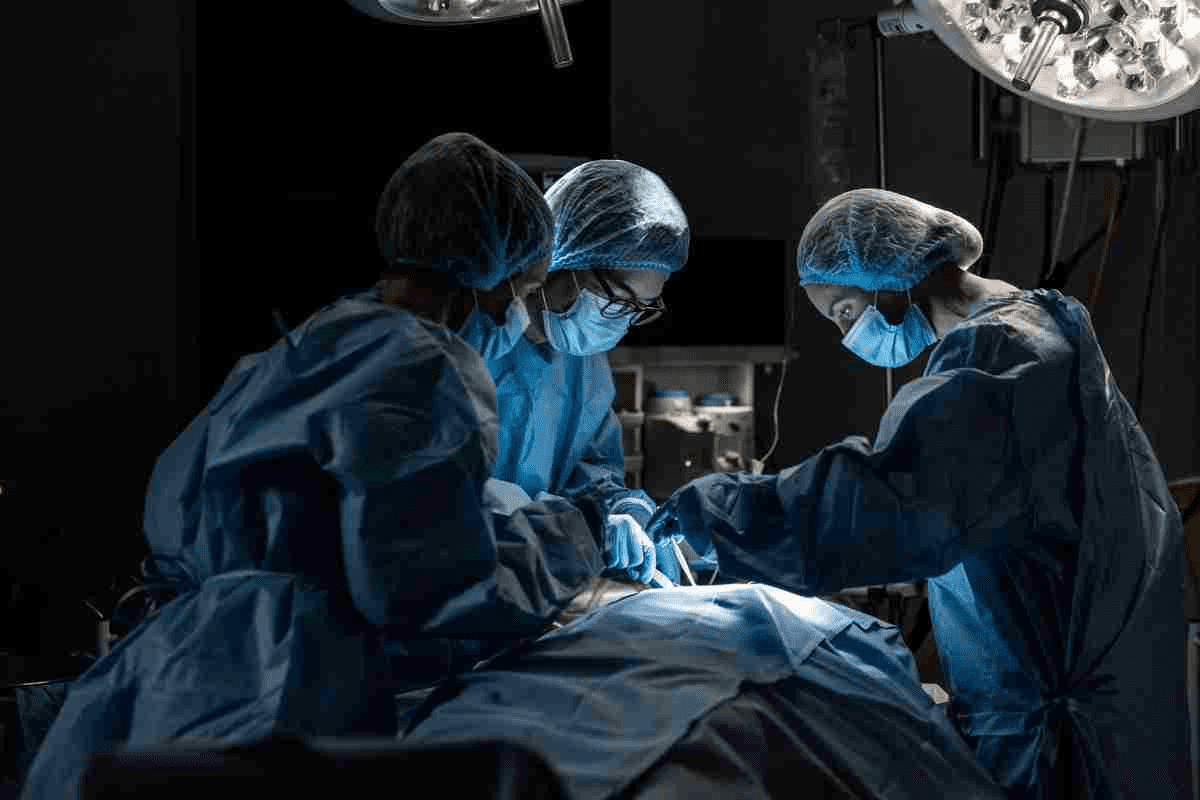
Surgical Approaches: Radical Prostatectomy
Removing the prostate through surgery is a common treatment. This surgery can be done in different ways:
- Open surgery
- Laparoscopic surgery
- Robotic-assisted laparoscopic surgery
The choice of method depends on the patient’s health, cancer stage, and the surgeon’s skill. Robotic prostatectomy is popular for its accuracy and fewer complications.
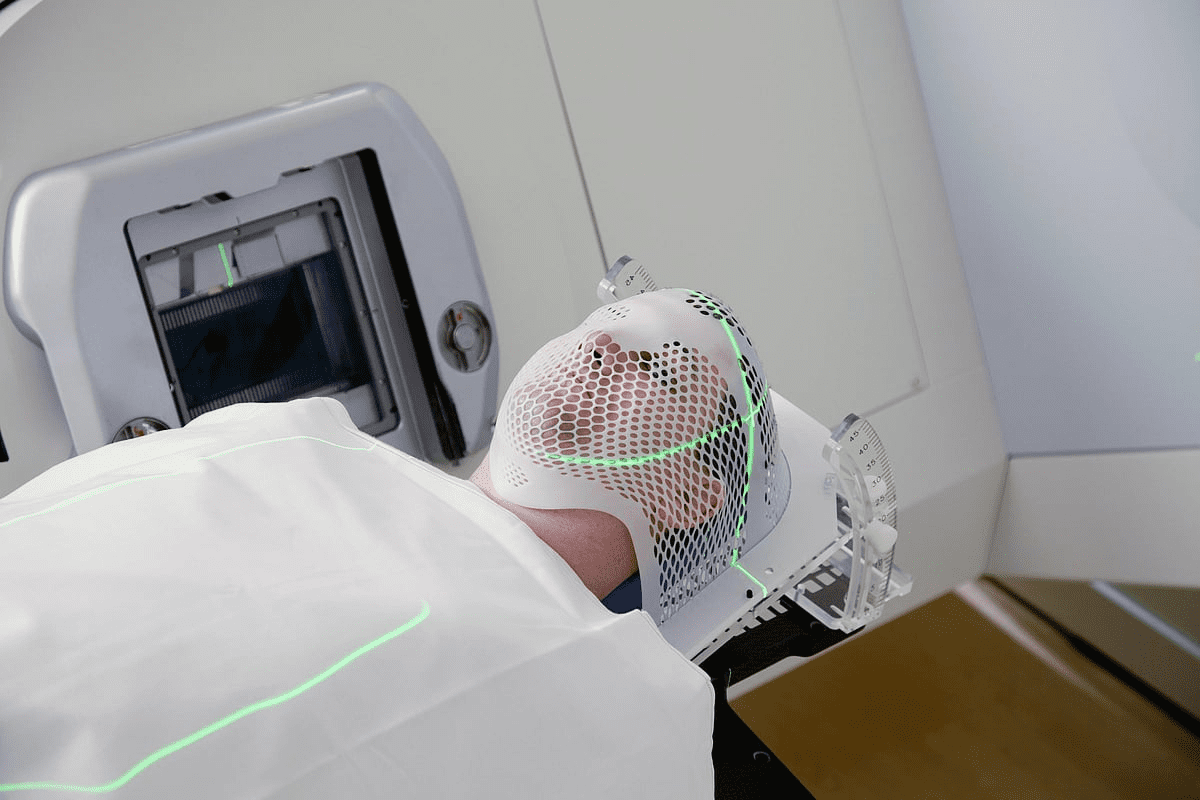
Radiation Therapy Approaches
Radiation therapy is also a key treatment for prostate cancer. It uses high-energy rays to kill cancer cells. There are two main types:
- External Beam Radiation Therapy (EBRT)
- Brachytherapy
EBRT sends radiation from outside the body. Brachytherapy places radioactive seeds in the prostate. Advances in radiation technology have made these treatments more precise, reducing side effects.
Active Surveillance as a Management Strategy
For those with low-risk prostate cancer, active surveillance might be suggested. This means watching the cancer closely with tests and biopsies, but not treating right away. The aim is to delay treatment and its side effects until the cancer grows more aggressive.
Other Treatment Modalities
There are more treatment options beyond surgery and radiation. These include:
| Treatment Modality | Description |
| Cryotherapy | Freezing prostate tissue to destroy cancer cells |
| Hormone Therapy | Reducing testosterone levels to slow cancer growth |
| Immunotherapy and Targeted Therapy | Stimulating the immune system or targeting specific cancer cell characteristics |
These treatments can be used alone or together, based on the cancer and the patient’s health.
Comparing Effectiveness: Surgery vs. Radiation for Prostate Cancer
It’s important for patients and doctors to know how surgery and radiation compare for prostate cancer. When picking a treatment, looking at how well it controls cancer, survival rates, and if more treatments are needed is key.
Cancer Control and Survival Rates
How well a treatment controls cancer and survival rates are key to judging its success. Both surgery and radiation can be very effective, but results depend on the cancer’s stage and how aggressive it is.
A study in the Journal of Clinical Oncology found that for early-stage prostate cancer, surgery and radiation have similar survival rates at 10 years. But, surgery tends to have lower rates of cancer coming back.
“The choice between surgery and radiation therapy for prostate cancer should be based on individual patient characteristics, including cancer stage, overall health, and personal preferences.”
Biochemical Recurrence Rates
Biochemical recurrence, shown by rising PSA levels after treatment, is also important. Studies show that recurrence rates can vary a lot between surgery and radiation.
| Treatment | 5-Year Biochemical Recurrence-Free Survival | 10-Year Biochemical Recurrence-Free Survival |
| Surgery | 80-90% | 70-80% |
| Radiation Therapy | 70-85% | 60-75% |
Need for Secondary Treatments
How often you need more treatments after the first one is another thing to consider. Patients who have surgery might need radiation if cancer comes back. Those who get radiation might need surgery or other treatments.
A study found that more patients who got radiation needed extra treatments than those who had surgery.
Recent Comparative Studies and Their Findings
New studies keep giving us insights into surgery and radiation for prostate cancer. A recent study found that while survival rates were similar, there were differences in complications and side effects.
As we keep improving prostate cancer treatments, knowing these details is vital. By looking at the latest research and each patient’s situation, doctors can give the best advice for treatment.
Side Effects and Quality of Life: Surgery
Thinking about surgery for prostate cancer? It’s key to know the possible side effects. Surgery can be a good choice, but knowing the risks is important. This helps you understand how it might affect your life.
Short-term Complications
Right after surgery, you might face issues like infection, bleeding, or reactions to anesthesia. These problems are not common but can be serious. We watch our patients closely after surgery to lower these risks.
Urinary Incontinence Rates and Management
Many men deal with urinary incontinence after prostate surgery. How bad it is can depend on the surgery and the person. But, most men get better over time. There are ways to manage incontinence while you recover.
| Time Post-Surgery | Continence Recovery Rate |
| 3 months | 40-60% |
| 6 months | 70-80% |
| 1 year | 80-90% |
Erectile Dysfunction After Prostatectomy
Erectile dysfunction (ED) is another possible side effect. The chance of getting ED depends on your age, how well you were doing before surgery, and the surgery type. Using nerve-sparing techniques can help lower the risk. We talk to our patients about ED and how to manage it.
Other Possible Surgical Complications
There are other, less common risks like hurting nearby structures or getting lymphoceles. These are rare but important to know about. Knowing these risks is part of making an informed choice.
It’s vital to understand these possible side effects and complications. This helps set clear expectations and make the best treatment choice. We work with our patients to reduce risks and help with any recovery issues.
Side Effects and Quality of Life: Radiation Therapy
Radiation therapy is a common treatment for prostate cancer. It comes with challenges and side effects that can affect a patient’s quality of life. We need to look at both the immediate and long-term effects on patients.
Acute Radiation Side Effects
Patients may feel tired, have to go to the bathroom often, and experience bowel irritation during and after radiation therapy. Fatigue is a common complaint, making patients feel more tired than usual. It’s important to manage these side effects to keep patients’ quality of life during treatment.
Long-term Bowel and Bladder Issues
Radiation therapy can cause long-term bowel and bladder problems. Chronic bowel problems include diarrhea or rectal bleeding. Bladder issues can be urinary incontinence or frequency. The severity of these issues varies among patients, and some may need ongoing management.
Sexual Function After Radiation
Radiation therapy can affect sexual function in prostate cancer patients. Erectile dysfunction is a possible long-term side effect. The extent of this effect depends on several factors, including the type and dose of radiation. Patients should talk to their healthcare provider about treatments for erectile dysfunction.
Secondary Cancer Risks
There’s a risk of developing secondary cancers from radiation therapy. While the risk is low, it’s something patients and healthcare providers should consider. The risk depends on the dose of radiation and the patient’s age at treatment.
It’s important for prostate cancer patients to understand the side effects and long-term implications of radiation therapy. Being informed helps patients make better choices and work with their healthcare team to manage side effects.
Recovery Timeline Comparison
The recovery time after prostate cancer treatment depends on the treatment type. Surgery and radiation have different recovery paths. Knowing these differences helps set realistic goals and make informed choices.
Hospital Stay and Initial Recovery: Surgery
Surgery for prostate cancer, like radical prostatectomy, means a hospital stay of one to three days. At home, recovery takes several weeks. During this time, patients might feel pain, tired, and unable to do much.
Doctors advise avoiding heavy lifting and strenuous activities for six weeks after surgery. Recovery is checked at follow-up visits. Most men can get back to normal in 3 to 6 months.
Treatment Duration and Recovery: Radiation
Radiation therapy for prostate cancer can be external or internal. External beam radiation therapy lasts several weeks, with daily sessions. Brachytherapy might take just one session or a few days.
Recovery from radiation therapy takes longer than surgery. Some men feel tired and have urinary or bowel changes for weeks to months. Recovery can take up to a year or more.
Return to Normal Activities
The time to get back to normal varies between surgery and radiation. Surgery recovery takes 3 to 6 months. Radiation recovery is slower, with side effects lasting several months.
“The journey through treatment is unique to each individual, and understanding the recovery process can significantly impact a patient’s ability to cope and recover.” – A healthcare professional’s insight into prostate cancer treatment recovery.
Long-term Recovery Considerations
Long-term recovery includes managing side effects like urinary incontinence and erectile dysfunction. These can affect quality of life. Ongoing support and management are key for a good recovery.
| Recovery Aspect | Surgery | Radiation Therapy |
| Hospital Stay | 1-3 days | Not applicable |
| Initial Recovery | Several weeks | Several weeks to months |
| Return to Normal Activities | 3-6 months | Variable, up to several months |
| Long-term Side Effects | Urinary incontinence, erectile dysfunction | Bowel changes, urinary issues, erectile dysfunction |
Age as a Factor in Treatment Selection
Age is key when picking a prostate cancer treatment. Patients look at their age, health, and cancer details to decide. These factors help choose the right treatment.
Treatment Recommendations by Age Group
Younger patients might get more aggressive treatments. This is because they have more years to live and fewer health issues. Older patients might get less invasive treatments or watchful waiting. This depends on their health and cancer type.
- Younger patients (less than 60 years): Often considered for radical treatments like surgery or radiation therapy due to their longer life expectancy.
- Older patients (60-75 years): Treatment choices depend on overall health and cancer aggressiveness. Some may undergo surgery or radiation, while others might be recommended for active surveillance.
- Elderly patients (over 75 years): Typically considered for less aggressive treatments, focusing on managing symptoms and improving quality of life, unless they have a high-risk cancer.
Life Expectancy Considerations
Life expectancy is key in choosing treatments. Patients with more years to live often get more aggressive treatments. Those with less time might get less intense treatments to avoid side effects.
We look at life expectancy when picking treatments. We make sure the treatment fits the patient’s health and cancer.
Age-Related Complication Risks
Age affects the risk of treatment complications. Older patients face higher risks due to health issues and less body strength. For example, they might face more urinary problems or erectile dysfunction after surgery.
- Surgical complications can include urinary incontinence and erectile dysfunction.
- Radiation therapy side effects might involve bowel and bladder issues.
- Active surveillance carries the risk of cancer progression if not monitored closely.
We consider age, life expectancy, and health to tailor treatments. This helps manage prostate cancer and reduce risks.
The Role of Cancer Staging and Risk Classification
Knowing the stage and risk of prostate cancer is key to picking the right treatment. Staging and risk classification help both patients and doctors make smart choices. This is important for the best treatment plan.
Low-Risk Prostate Cancer Treatment Preferences
For those with low-risk prostate cancer, watching and waiting is often the first step. This means regular checks with PSA tests, digital exams, and biopsies. It aims to avoid the side effects of aggressive treatments while keeping an eye on the cancer.
A study in the Journal of Clinical Oncology found watching and waiting is safe and works well. It shows men with low-risk cancer have a low chance of dying from it.
Intermediate-Risk Disease Approaches
Those with intermediate-risk cancer might need more action. Options include surgery, radiation, or both. The choice depends on health, life expectancy, and what the patient wants.
- Surgery: Radical prostatectomy is a common choice for intermediate-risk cancer, aiming for a cure.
- Radiation Therapy: External beam or brachytherapy can be effective, sometimes with hormone therapy too.
High-Risk Disease Management
High-risk prostate cancer needs strong treatment. Plans are made just for the person, looking at the cancer’s stage and the patient’s health.
A study in the Journal of Urology showed combining treatments like radiation and hormone therapy helps. It improves outcomes for men with high-risk cancer.
Personalized Risk Assessment Tools
New tools in personalized medicine help better understand risk and guide treatment. For example, the Signatera test can spot cancer cells in the blood. It’s more accurate than old methods.
As a Natera news release points out, these tools are changing prostate cancer treatment. They give doctors more precise info, helping them make better choices.
Active Surveillance vs. Immediate Treatment
Prostate cancer treatment now includes active surveillance, which watches the disease instead of treating it right away. This method is getting more attention because it might lower the risks of surgery or radiation.
Candidates for Active Surveillance
Active surveillance is best for men with low-risk prostate cancer. Low-risk prostate cancer means a low Gleason score, a low PSA level, and small cancer in biopsies. We look at many things to see if active surveillance is right, like the patient’s health, how long they might live, and what they want.
Monitoring Protocols and Triggers for Intervention
Men on active surveillance get checked often. This includes PSA tests, digital rectal exams, and biopsies. Monitoring protocols help find any changes in the cancer. If big changes happen, like a Gleason score increase or PSA level rise, treatment might be considered again.
Psychological Aspects of Watchful Waiting
The mental side of active surveillance is important. Men on surveillance might worry about the cancer getting worse.
“The uncertainty of not knowing whether the cancer will progress can be a significant source of stress.”
We stress the need for mental support and counseling. This helps men deal with the emotional side of waiting and watching.
In summary, active surveillance is a good choice for men with low-risk prostate cancer. Knowing who it’s for, how it’s monitored, and its mental impact helps men make better choices about their health.
Physician Influence on Treatment Decisions
Choosing a specialist for prostate cancer treatment can greatly affect your care path. Prostate cancer is complex, and doctors’ opinions are key in making decisions.
Specialist Bias: Urologists vs. Radiation Oncologists
Urologists and radiation oncologists may have different views on treating prostate cancer. Urologists might suggest surgery, while radiation oncologists might recommend radiation therapy. This difference comes from their expertise and familiarity with treatments.
A study in the Journal of Clinical Oncology showed that urologists often recommend surgery. Radiation oncologists, on the other hand, suggest radiation therapy more often. This shows how important it is to know about specialist biases.
Multidisciplinary Approach Benefits
A multidisciplinary approach brings together specialists from different fields. This team includes urology, radiation oncology, and more. It offers a complete view of treatment options.
The benefits of this approach are:
- A more holistic understanding of the patient’s condition
- Access to a broader range of treatment options
- Better coordination of care
- Improved patient outcomes
| Benefits | Description |
| Comprehensive Understanding | A team approach provides a more complete view of the patient’s condition. |
| Broad Treatment Options | Patients have access to various treatments, including surgery, radiation, and other therapies. |
| Better Care Coordination | A multidisciplinary team ensures that all aspects of care are well-coordinated. |
Second Opinion Importance
Getting a second opinion is key to informed decisions. It offers new insights into diagnosis and treatment, boosting confidence in choices.
Patients who get second opinions often feel more in control and satisfied with their care. It’s important to see getting a second opinion as a normal part of treatment, impacting outcomes greatly.
Financial Considerations: Cost Comparison
It’s important for prostate cancer patients to know the cost differences between surgery and radiation therapy. The cost of cancer treatment can be high. Understanding these costs is key to making informed decisions.
Insurance Coverage Differences
Insurance coverage for prostate cancer treatment varies a lot. Many plans cover both surgery and radiation. But, the amount covered can be different.
A study in the Journal of Clinical Oncology showed that insurance coverage for surgery varied. This affected how much patients had to pay out-of-pocket. Radiation therapy patients also faced different coverage levels based on their insurance.
| Treatment Type | Average Cost | Average Insurance Coverage | Average Out-of-Pocket Expenses |
| Surgery (Radical Prostatectomy) | $40,000 – $60,000 | 80% – 90% | $4,000 – $12,000 |
| Radiation Therapy | $30,000 – $50,000 | 80% – 90% | $3,000 – $10,000 |
Out-of-Pocket Expenses
Even with insurance, out-of-pocket expenses for prostate cancer treatment can be high. These costs include deductibles, copays, and extra treatments or complications.
A study by the American Cancer Society found that prostate cancer patients often face big out-of-pocket expenses. This can affect their financial stability and quality of life.
Long-term Financial Impact
The financial impact of prostate cancer treatment goes beyond the initial costs. Patients may lose income due to recovery time, have ongoing medical expenses, and deal with treatment side effects.
Research shows that prostate cancer can lead to financial hardship for some patients. It’s important to plan financially and get support.
Innovations in Prostate Cancer Treatment Options
Prostate cancer treatment has made big strides in recent years. These changes are making care better and outcomes more positive. Now, there are more effective and tailored treatments for men with prostate cancer.
Advances in Surgical Techniques
Surgery for prostate cancer has improved a lot. Robotic prostatectomy is a big step forward. It lets doctors remove the prostate gland more precisely, cutting down on risks and speeding up recovery.
Robotic surgery has many benefits:
- It’s more precise and accurate
- It lowers the chance of urinary problems and erectile issues
- It uses smaller cuts, leaving less scar
- Patients often stay in the hospital less and recover faster
Next-Generation Radiation Technologies
Radiation therapy for prostate cancer has also improved. New technologies like Intensity-Modulated Radiation Therapy (IMRT) and Stereotactic Body Radiation Therapy (SBRT) are more precise. They target the tumor better, protecting healthy tissues.
These new radiation technologies offer:
- Better tumor control and fewer side effects
- Shorter treatment times, making it easier for patients
- They help keep more of the surrounding tissues safe
Focal Therapy Approaches
Focal therapy is a new way to treat prostate cancer. It focuses on the exact area with cancer, not the whole gland. This method aims to lessen side effects while controlling the cancer well.
Focal therapy includes:
- High-Intensity Focused Ultrasound (HIFU)
- Cryotherapy
- Laser-induced Thermotherapy
Immunotherapy and Targeted Treatments
Immunotherapy and targeted treatments are becoming key for prostate cancer. Immunotherapy for prostate cancer uses the body’s immune system to fight cancer. Treatments like checkpoint inhibitors are showing promise in trials.
Targeted therapies aim at specific cancer molecules. They could lead to more effective and less harmful treatments.
As research keeps moving forward, we’ll see even more new treatments for prostate cancer. These advancements will improve patient outcomes and quality of life.
Working with Your Healthcare Team
Dealing with prostate cancer treatment means working together with your healthcare team. This teamwork is key to making choices that fit your values, health, and goals.
Assembling a Multidisciplinary Care Team
A team of experts is vital for prostate cancer care. This team usually includes:
- Urologists: They handle surgical treatments for prostate cancer.
- Radiation Oncologists: They specialize in radiation therapy.
- Medical Oncologists: They focus on systemic treatments like hormone therapy and chemotherapy.
- Nurses and Nurse Navigators: They offer support and guidance during treatment.
- Support Staff: They include social workers, counselors, and others who help with emotional and practical care.
Having a team with different skills ensures your care is well-rounded. This leads to more personalized and effective treatment plans.
Key Questions to Ask Your Doctors
Being active in your care means asking the right questions. Discuss these with your doctors:
- What are the specific characteristics of my prostate cancer, and how do these influence treatment choices?
- What are the benefits and risks of each treatment option?
- How will the recommended treatment affect my quality of life, both short-term and long-term?
- Are there any clinical trials or emerging treatments that might be right for me?
- What support resources are available to help manage the emotional and practical aspects of my care?
Asking these questions helps you understand your diagnosis and the treatment choices.
Shared Decision-Making Approaches
Shared decision-making is a team effort. You and your healthcare team make decisions together. This ensures your treatment fits your needs and values.
“The goal of shared decision-making is to ensure that patients receive care that is not only effective but also aligned with their personal values and preferences.”
Support Resources for Treatment Decisions
Prostate cancer treatment can be complex and emotionally tough. Luckily, there are many support resources to help:
- Patient Support Groups: Connecting with others who have gone through similar challenges can offer emotional support and advice.
- Educational Materials: Many organizations provide educational resources to help patients understand their diagnosis and treatment options.
- Counseling Services: Professional counseling can help deal with the emotional impact of a prostate cancer diagnosis.
- Navigational Services: Some healthcare systems offer navigational services to help patients coordinate their care and access support resources.
By using these resources and working closely with your healthcare team, you can make informed decisions. You’ll also get the support you need throughout your treatment journey.
Conclusion: Making an Informed Treatment Decision
When you face prostate cancer, choosing the right treatment is key. We’ve looked at surgery, radiation, and active surveillance. It’s important to know the options, how well they work, and any side effects.
Choosing a treatment depends on the cancer’s stage, your age, and health. Working with your healthcare team is vital. They help pick the best treatment for you.
Being informed means looking at the latest research and thinking about your values. This helps you make a choice that fits your life.
Having a team of doctors and asking the right questions helps you make a good choice. We urge you to be involved in your care. Get help from your doctors and family to go through treatment.
FAQ
What are the main treatment options for prostate cancer?
Treatments for prostate cancer include surgery, radiation therapy, and active surveillance. Other options are focal therapy and immunotherapy.
How do surgery and radiation therapy compare in terms of effectiveness for prostate cancer?
Surgery and radiation therapy both work well against prostate cancer. They have similar results in controlling cancer and survival rates. The choice depends on the patient’s health and cancer stage.
What are the side effects of prostate cancer surgery?
Surgery can lead to urinary incontinence and erectile dysfunction. Patients may also face short-term issues like infection and bleeding.
What are the side effects of radiation therapy for prostate cancer?
Radiation can cause urinary frequency and fatigue. It may also lead to long-term problems like bowel and bladder issues and a higher risk of secondary cancers.
How does age influence the choice of treatment for prostate cancer?
Age is key in choosing treatment. Older patients might face more risks with surgery. Treatment plans vary by age, considering life expectancy.
What is active surveillance, and who is a candidate for it?
Active surveillance is for patients with low-risk prostate cancer. It involves regular monitoring. Candidates have low-risk disease and are closely watched with tests and imaging.
How do physicians influence treatment decisions for prostate cancer?
Doctors are vital in making treatment choices. Their opinions can influence decisions. A team approach and seeking a second opinion are helpful.
What are the financial implications of choosing surgery versus radiation therapy for prostate cancer?
The cost of treatment varies. Insurance, out-of-pocket costs, and long-term expenses differ. Patients should think about these when deciding.
What are the latest innovations in prostate cancer treatment?
New treatments include better surgery methods, advanced radiation, focal therapy, and immunotherapy. These are improving outcomes.
How can patients make informed treatment decisions for prostate cancer?
Patients should work with a team of doctors. Asking questions and considering personal factors are key. Staying updated with medical evidence is also important.
What is the role of cancer staging and risk classification in determining treatment for prostate cancer?
Staging and risk classification guide treatment choices. Plans vary based on disease risk level.
How do treatment outcomes compare for prostatectomy versus radiation therapy?
Outcomes for surgery and radiation are similar. But, the risk of cancer coming back and needing more treatment can differ.
What are the benefits of a multidisciplinary care team in prostate cancer treatment?
A team approach offers a complete treatment plan. It combines specialists’ expertise for better decision-making and support.
References
- Men’s Perspectives on Selecting Their Prostate Cancer Treatment. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC4283563/