Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
The primary physical indication for surgical intervention is the presence of visible xanthelasma plaques that cause aesthetic dissatisfaction. These lesions present as soft, yellowish papules or plaques that are usually symmetrical and may involve all four eyelids in severe cases. They typically start small but can coalesce into large, band-like structures.
The texture of the plaque is distinct from the surrounding skin. It often appears slightly raised and velvety. In advanced stages, the plaques can become tuberous or nodular. The morphology dictates the surgical approach: flat lesions are amenable to simple excision, whereas nodular lesions may require deeper dissection.

The location of the xanthelasma is a critical physical indication. Most commonly, they originate at the medial canthus (inner corner) of the upper eyelid. Over time, they may spread laterally across the lid and involve the lower eyelid. The depth of the lesion determines whether surface treatments will suffice or if full-thickness excision is required.
Deeply infiltrating lesions that extend into the orbicularis oculi muscle are strong candidates for surgery. Surface lasers may not reach these deep foam cells without causing excessive scarring. Surgery allows for the precise removal of the deep component while preserving the overlying muscle function.

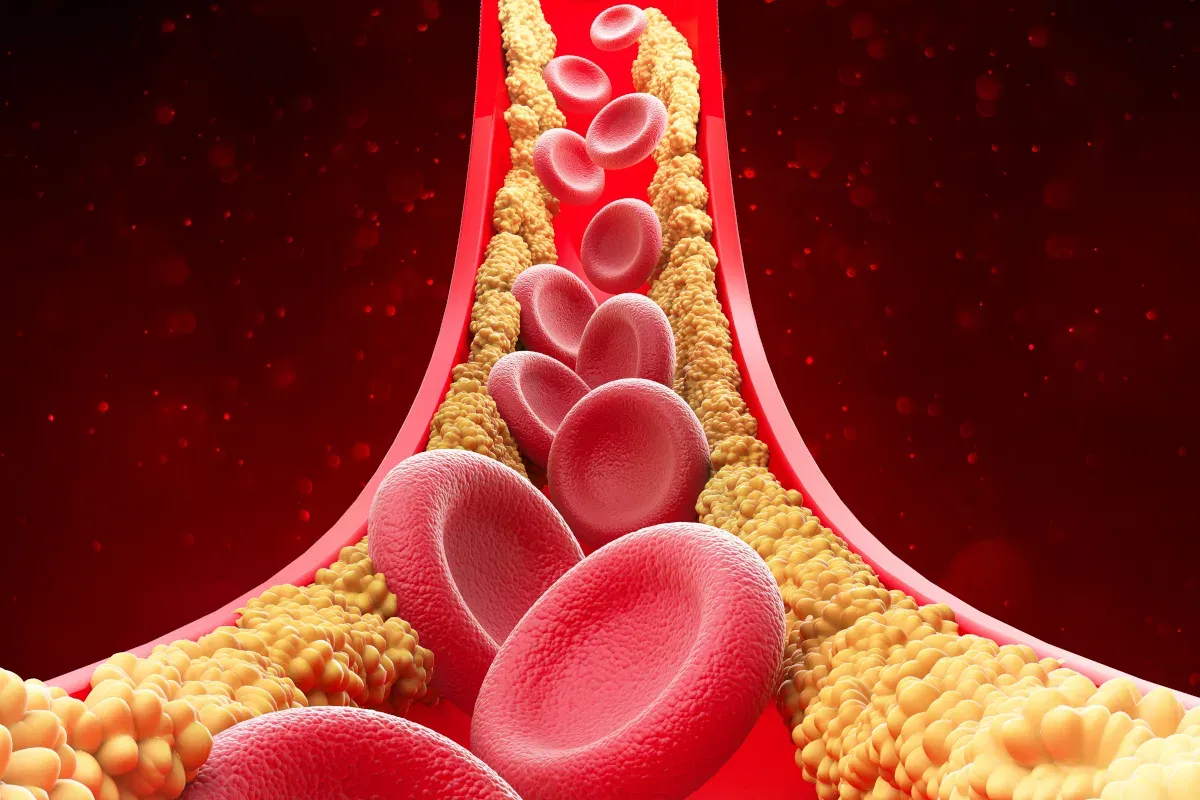
A leading biological cause of xanthelasma is hyperlipidemia, a condition characterized by elevated blood lipid levels. Specifically, high levels of low-density lipoprotein (LDL) and triglycerides are often associated with the formation of these plaques. The excess lipids in the bloodstream permeate the capillary walls in the eyelid skin and are engulfed by macrophages.
These lipid-laden macrophages, or foam cells, become trapped in the tissue, creating the visible plaque. Patients with xanthelasma have a higher statistical probability of atherosclerosis and cardiovascular disease. This biological link makes lipid profiling an essential part of the clinical picture.
Genetics plays a significant role in the development of xanthelasma. Familial Hypercholesterolemia is a genetic disorder that leads to dangerously high cholesterol levels from birth. Individuals with this condition frequently develop xanthelasma in childhood or early adulthood.
Even without a specific named syndrome, a family history of xanthelasma or early heart disease is a strong biological predictor. Genetic polymorphisms that affect lipid metabolism and macrophage function contribute to the eyelid skin’s susceptibility to lipid deposition, regardless of diet.

Interestingly, a significant portion of patients with xanthelasma have normal lipid levels (normolipidemic). In these cases, the cause is thought to be a local tissue abnormality or an inflammatory response. The eyelid skin may have an inherent defect that allows localized lipid leakage or retention.
Factors such as chronic low-grade inflammation, altered capillary permeability, and local macrophage dysfunction are implicated. This indicates that xanthelasma is not solely a systemic disease but also a localized cutaneous disorder, justifying local surgical treatment even in healthy individuals.
Xanthelasma can be a secondary symptom of other metabolic disorders. Diabetes mellitus is a common comorbid condition, as insulin resistance affects lipid metabolism. Hypothyroidism (underactive thyroid) can also lead to elevated lipid levels and the subsequent formation of xanthelasma.
Liver diseases, such as primary biliary cirrhosis, can cause obstructive jaundice and hyperlipidemia, resulting in extensive xanthomas and xanthelasma. Identifying these underlying biological causes is crucial for preventing recurrence and managing the patient’s overall health.


Send us all your questions or requests, and our expert team will assist you.

While primarily cosmetic, large or thick xanthelasma plaques can cause functional issues. The added weight of lipid deposits on the upper eyelid can contribute to mechanical ptosis, a condition in which the eyelid droops. This can make the eyes feel heavy and tired, especially toward the end of the day.
In severe cases, the drooping eyelid can encroach upon the superior visual field. The patient may have to strain their forehead muscles to keep their eyes open, which can lead to tension headaches. Removing the heavy plaques relieves this weight and restores a more comfortable eyelid position.
The raised and irregular texture of xanthelasma can interfere with eyelid hygiene. The crevices around nodular plaques can trap debris, oils, and makeup, leading to local irritation or blepharitis (eyelid inflammation). Patients often report difficulty thoroughly cleaning the area.
For those who wear glasses, large lesions on the medial side can interfere with the fit of the nose pads. The friction from the glasses can cause the plaques to become inflamed or tender. Surgical removal restores a smooth surface that is easy to clean and does not obstruct eyewear.
Large lesions located near the tear ducts (lacrimal puncta) can interfere with the drainage of tears. If the plaque distorts the position of the eyelid margin, it can lead to epiphora, or watering eyes. The mechanical displacement of the punctum prevents tears from draining properly.
Surgery in this delicate area requires extreme precision to avoid damaging the lacrimal system. However, correcting the distortion caused by the plaque can often improve tear mechanics and resolve tearing or dry eye symptoms associated with lid malposition.
The psychological impact of xanthelasma is a significant indication for surgery. The yellow plaques are evident and challenging to conceal with makeup. Patients often report feeling self-conscious, embarrassed, and perceived as “unhealthy” or “aged” by others.
The eyes are the focal point of facial communication. The presence of disfiguring plaques can affect social confidence and professional interactions. The desire to restore a normal appearance and eliminate the stigma associated with the lesions is a valid and significant reason for seeking surgical correction.


Yes, there is a strong hereditary component to xanthelasma. If your parents or siblings have the condition, you are genetically more predisposed to developing it. This is often linked to inherited lipid disorders like Familial Hypercholesterolemia.
Diabetes is a risk factor. Uncontrolled diabetes often leads to high levels of triglycerides and other lipids in the blood. This systemic lipid imbalance can contribute to the formation of xanthelasma plaques on the eyelids.
Indirectly, yes. Chronic stress can negatively impact your metabolism, lead to poor dietary choices, and increase inflammation. While stress doesn’t cause xanthelasma directly, it can exacerbate the underlying conditions, like high cholesterol, that lead to it.
Recurrence is common because the underlying cause—whether systemic high cholesterol or a local skin predisposition—may persist. If lipid levels remain high or the genetic tendency persists, new deposits can form in the same area or nearby areas.
Typically, xanthelasma plaques are painless and do not cause itching. They are soft to the touch. If an eyelid lesion is painful, bleeding, or rapidly changing in shape, it may be a different condition and should be evaluated by a doctor immediately.







Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)