Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.

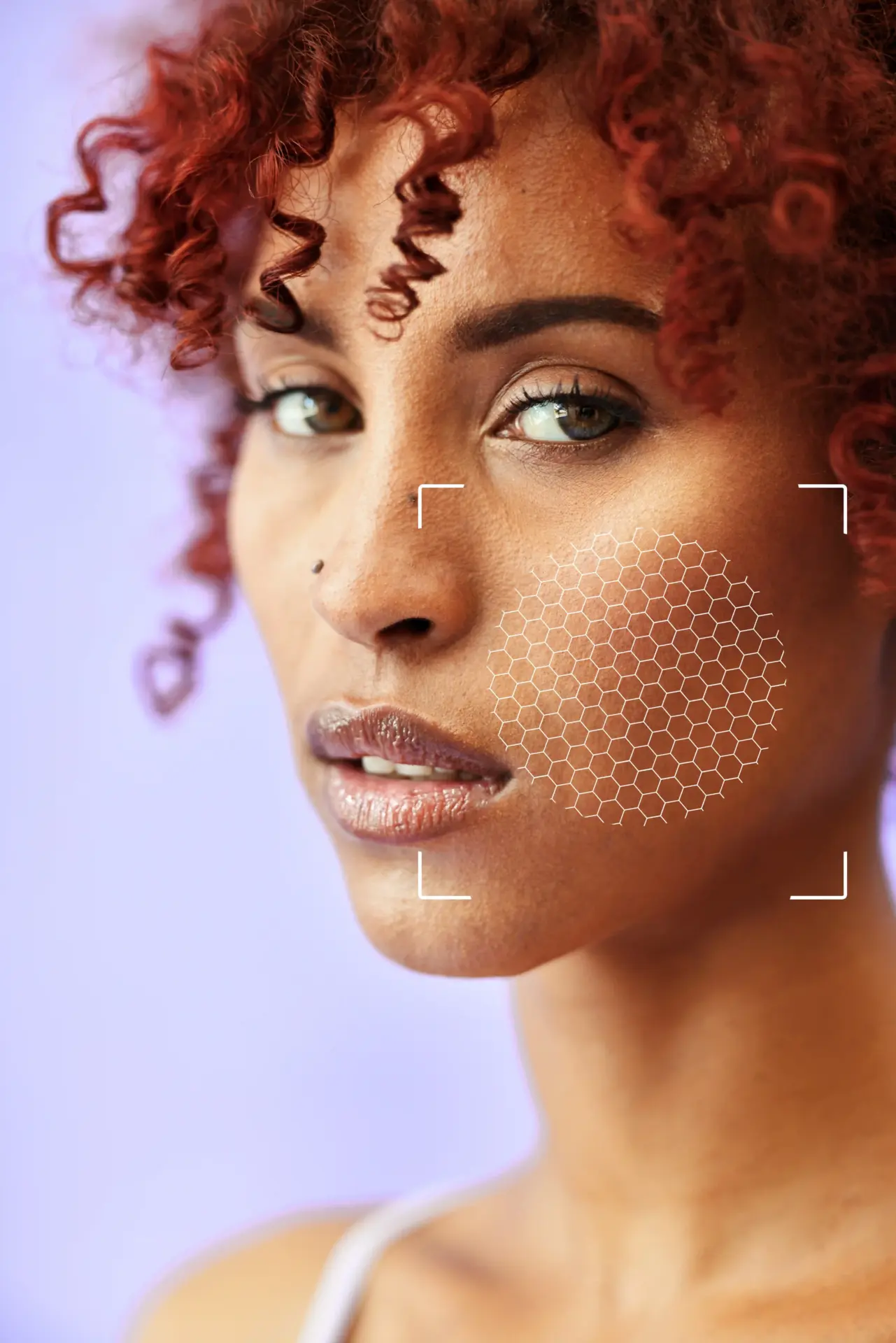
Modern consultations utilize digital mapping technology to visualize the extent of the disease. High-resolution photography is used to document the lesions. The surgeon may use digital tools to outline the boundaries of the plaques, which often extend beyond what is visible to the naked eye under standard lighting.
Simulation software can be used to demonstrate the potential results of the surgery. By digitally removing the lesions from the patient’s image, the surgeon can show the expected improvement in the eyelid contour. This helps in managing expectations regarding scarring and the final aesthetic outcome.
High-resolution medical photography
Digital delineation of plaque boundaries
Visualization of subsurface extension
Simulation of post-surgical results
Objective baseline for monitoring

A critical component of the physical exam is assessing skin elasticity, also known as the “pinch test.” The surgeon gently pinches the eyelid skin to determine the degree of laxity. This assessment dictates whether a simple excision is possible or if a more complex flap or graft is needed.
If the patient has abundant loose skin (dermatochalasis), the surgeon can remove the xanthelasma and close the wound primarily without tension. If the skin is tight, removing a large lesion could pull the eyelid down (ectropion). This measurement is the key determinant of surgical feasibility.
The surgeon also evaluates the integrity of the orbicularis oculi muscle, which lies directly beneath the skin. Xanthelasma can sometimes infiltrate this muscle layer. Understanding the depth of involvement is essential for surgical planning to ensure muscle function is preserved.
The snap-back test is performed to assess the tone of the lower eyelid. The surgeon pulls the lower lid away from the eye and releases it to see how quickly it snaps back. Poor tone indicates a higher risk of malposition after surgery, requiring additional supportive measures like a canthopexy.

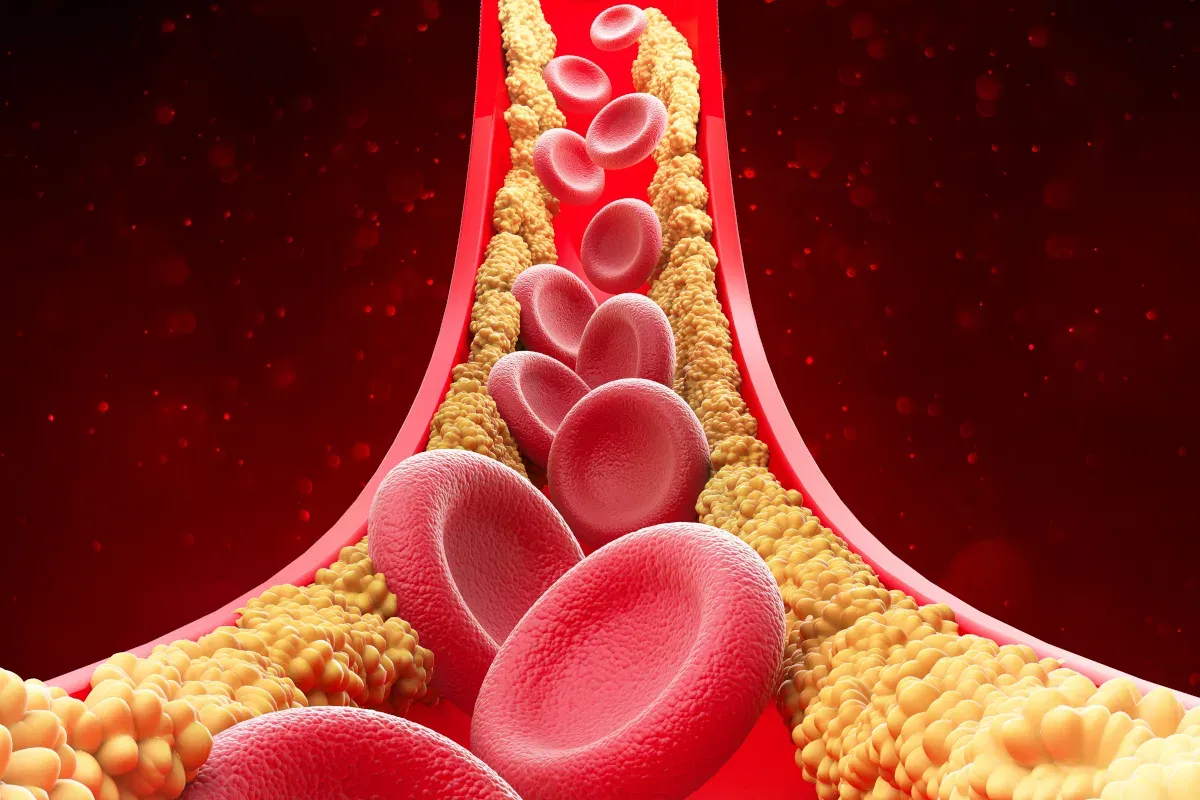
Surgical readiness involves reviewing the patient’s metabolic health. Patients are typically required to undergo a lipid panel to check their cholesterol and triglyceride levels. If levels are uncontrolled, the surgeon may recommend medical management alongside or before surgery to reduce the risk of recurrence.
Cardiovascular risk assessment is also routine. Since xanthelasma is a marker for heart disease, the surgeon may coordinate with the patient’s primary care physician or cardiologist. Optimizing systemic health is a prerequisite for long-term surgical success.
A thorough review of current medications is conducted to identify any agents that could increase bleeding risk. Blood thinners, antiplatelet drugs, and certain supplements (like fish oil and Vitamin E) can cause excessive bruising and hematoma formation in the delicate eyelid tissue.
Patients are generally advised to pause these medications under their prescribing doctor’s guidance for a specific period before surgery. This preparation minimizes complications and ensures a clean surgical field for microsurgical precision.


Send us all your questions or requests, and our expert team will assist you.

Nicotine is a potent vasoconstrictor that impairs microcirculation and wound healing. In eyelid surgery, where skin flaps are often used, blood flow is critical. Smoking significantly increases the risk of skin necrosis, poor scarring, and wound infection.
A strict smoking cessation protocol is often enforced. Patients are required to stop smoking and the use of nicotine products for several weeks before and after the procedure. This requirement ensures that the delicate eyelid tissues have the optimal oxygen supply needed for healing.
For large lesions, the surgeon maps the facial tension vectors. Understanding how the skin pulls and stretches is vital for incision placement. The goal is to orient the scar so that it is hidden in natural creases and does not fight against gravity or facial expression.
Digital tools or manual marking can be used to visualize these vectors. This planning prevents distortion of the eye shape, such as the “pulling” of the inner corner (medial canthal web), which is a difficult-to-correct complication of poor planning.
A basic eye examination is performed to document visual acuity and ocular surface health. Conditions such as dry eye syndrome must be identified preoperatively, as eyelid surgery can temporarily exacerbate dryness.
The position of the lacrimal punctum (tear drain) is carefully noted. Xanthelasma is often located dangerously close to this structure. Pre-operative identification ensures the surgeon plans the excision to protect the tear drainage system from injury or distortion.
The consultation concludes with logistical planning. Patients are informed about the recovery timeline, usually requiring a few days of social downtime due to swelling and stitches. Transportation arrangements are made if sedation is to be used.
Post-operative care supplies are discussed, including ice packs, antibiotic ointment, and artificial tears. Ensuring the patient has these items ready at home (“nesting”) reduces stress immediately after the procedure.


If your surgery is performed under local anesthesia only, you typically do not need to fast. However, if you are having sedation (twilight anesthesia), you will be required to fast (no food or drink) for a specific number of hours, usually 8 to 12, before the procedure.
If you receive sedation, you absolutely need a responsible adult to drive you home. Even with only local anesthesia, your vision might be blurry from ointment or swelling immediately after surgery, so having a driver is strongly recommended for safety.
No, generally you should continue taking your cholesterol medication (statins) as prescribed. Controlling your lipid levels helps prevent xanthelasma from recurring. Always confirm medication instructions with your surgeon.
No, you should not wear contact lenses on the day of surgery. You will likely need to wear glasses for the first week or two during recovery to avoid pulling on your eyelids while inserting or removing lenses.
If you have chronic dry eyes, inform your surgeon. Eyelid surgery can temporarily worsen dryness. Your surgeon may prescribe aggressive lubrication drops or ointment to use before and after surgery to protect your cornea.







Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)