Cardiology is the medical specialty focused on the heart and the cardiovascular system. It involves the diagnosis, treatment, and prevention of conditions affecting the heart and blood vessels. These conditions include coronary artery disease, heart failure, arrhythmias (irregular heartbeats), and valve disorders. The field covers a broad spectrum, from congenital heart defects present at birth to acquired conditions like heart attacks.
Send us all your questions or requests, and our expert team will assist you.
When you visit a doctor with concerns about your heart rhythm, the process of finding the answer is logical and thorough. The goal of diagnosis is not just to confirm that an arrhythmia exists but to pinpoint exactly where the electrical signal is going wrong and why. Fortunately, modern medicine provides a toolkit of tests that are painless, noninvasive, and highly effective at recording the heart’s activity. The diagnostic journey usually moves from simple conversations and basic checks to more advanced monitoring if needed. Doctors act like detectives, gathering clues from your story and your body to solve the puzzle. This section outlines the common cardiac arrhythmia diagnosis tests you might encounter, explaining what they are, why they are done, and what you can expect during each one. Understanding these tests can remove the anxiety of the unknown and help you prepare for your appointments.

The most important tool a doctor has is often a conversation. Before any wires are attached or machines are turned on, your doctor will want to hear your story. They will ask specific questions about what your symptoms feel like, when they happen, and what makes them better or worse. They will also ask about your family history—whether parents or siblings have had heart trouble—and about your lifestyle habits like smoking, caffeine intake, and exercise. This “history taking” provides the context for everything else.
After talking, the doctor will perform a physical exam. This involves listening to your heart with a stethoscope. They can hear the heart valves’ “lub-dub” and detect irregular rhythms, extra beats, or murmurs. They’ll check your pulse at your wrist or neck to feel the beat’s rate and strength. They might check your blood pressure and look for signs of swelling in your legs, which can be related to heart function. This basic exam gives the doctor a baseline and helps decide which specific tests are needed next.
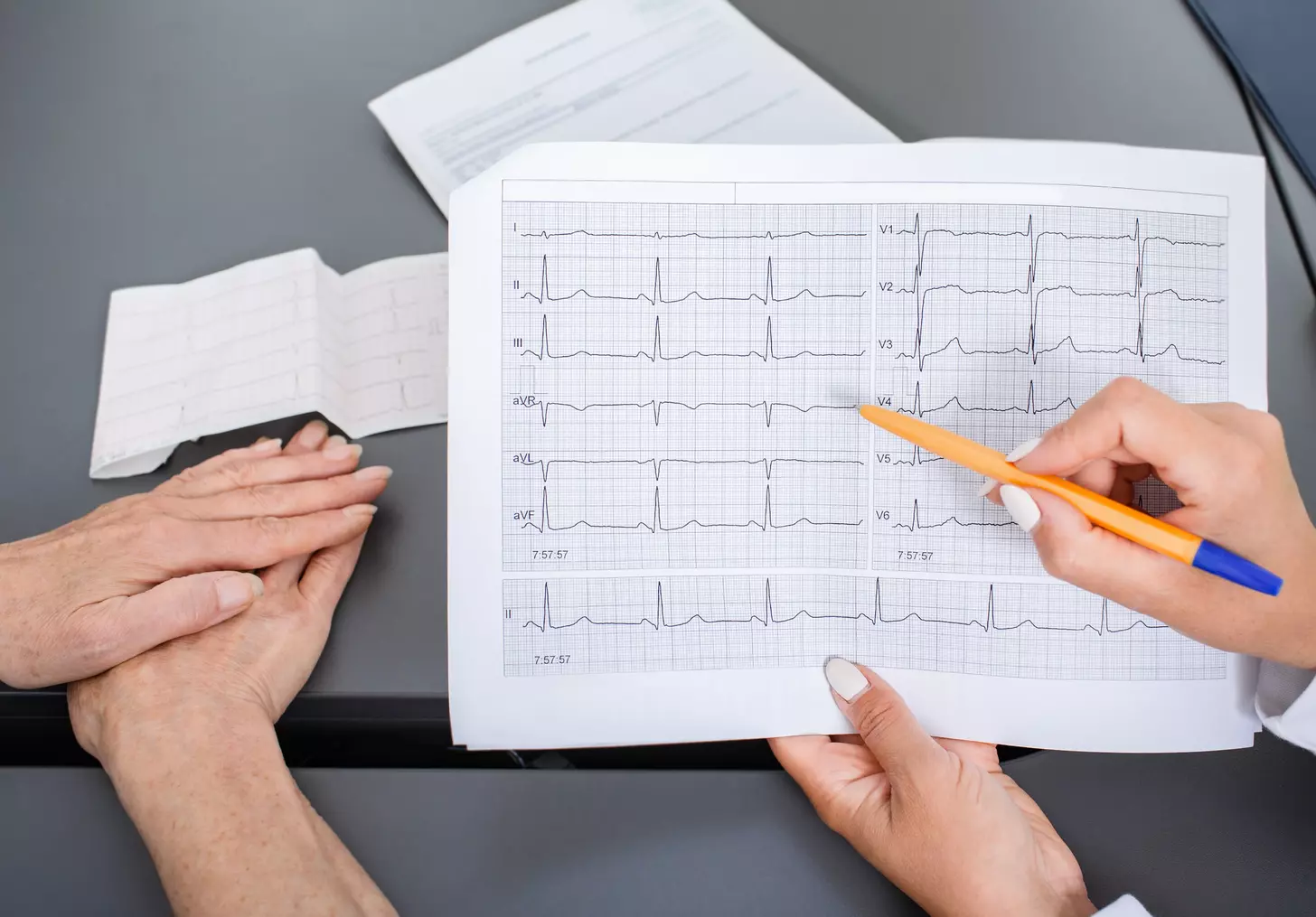
The electrocardiogram, commonly called an ECG or EKG, is the gold standard for diagnosing heart rhythm problems. It is a quick, painless, and safe test that records the electrical activity of your heart. You will be asked to lie down, and small sticky patches called electrodes will be placed on your chest, arms, and legs. These patches are connected by wires to a machine.
The machine does not send any electricity into your body; it simply listens to and records the electricity your heart is naturally making. The result is a graph drawn on paper or a screen, showing waves and spikes that represent each heartbeat. The doctor looks at the shape, timing, and spacing of these waves. They can instantly see if the heart is beating too fast or too slow or if the electrical signal is getting blocked. An ECG only records the heart for a few seconds, so it is perfect for detecting problems that are happening right now, but it might miss arrhythmias that come and go.

Since an ECG only captures a snapshot, doctors often need a “movie” of your heart rhythm over a longer period to catch arrhythmias that happen intermittently. This is where wearable monitors come in. These devices allow you to go about your daily life while the doctor gathers data.
A Holter monitor is a small, portable device about the size of a deck of cards or a small camera. You wear it for 24 to 48 hours while you go about your normal daily life. It has wires attached to patches on your chest. You can tuck the device into a pocket or clip it to your belt. It records every single heartbeat—over 100,000 of them—day and night. You will usually be asked to keep a diary of your activities and symptoms so the doctor can match what you felt with what the recording shows. It is a great way to see how your heart reacts to sleep, stress, and movement.
If your symptoms happen very rarely, like once a week or once a month, a 24-hour monitor might miss them. In these cases, an event recorder is used. This is a device you can wear for weeks at a time. Some types record constantly but only save the data when you push a button (when you feel a symptom). Others trigger automatically when they detect an abnormal rhythm. There are even tiny monitors that can be injected under the skin (loop recorders) to monitor the heart for years. These devices ensure that no matter when the arrhythmia strikes, the data is captured for the doctor to see.
While an ECG looks at the electricity, an echocardiogram looks at the structure. An echocardiogram is essentially an ultrasound of the heart. It uses sound waves to create a A A moving picture of your heart on a screen. A technician will put some cold gel on your chest and move a wand-like device (transducer) over your skin.
This test allows the doctor to see the heartbeat in real-time. They can measure the size of the heart chambers, see how well the heart muscle is pumping, and check if the valves are opening and closing correctly. This step is crucial because sometimes an arrhythmia is caused by a structural problem, like a weak heart muscle or a damaged valve. Knowing the physical condition of the heart helps guide the treatment plan. It is completely painless and uses no radiation. Other imaging tests like MRI or CT scans might be used in rare cases for more detailed views, but the echocardiogram is the standard “look inside.”
Some arrhythmias only happen when the heart is working hard. To catch these, doctors use a stress test. The goal is to make the heart beat faster and see how the electrical system handles the increased demand. The most common way to do these tasks is on a treadmill.
You will be hooked up to an ECG machine and asked to walk on a treadmill. The speed and incline will gradually increase, making you work harder. The doctor watches the ECG screen closely to see if an irregular rhythm starts as your heart rate goes up. They also monitor your blood pressure and ask how you are feeling. If you cannot walk on a treadmill due to joint problems, they can give you a medication that simulates the effect of exercise on the heart. This test aids in establishing the safety of your exercise routine and detects exercise-induced arrhythmias that may go undetected during rest.
If the non-invasive tests do not provide enough information, or if the doctor needs to pinpoint the exact location of the problem to fix it, they may perform an electrophysiology study (EPS). This is a minimally invasive procedure done in a special hospital lab. You are usually sedated but awake enough to follow instructions.
In this procedure, thin, flexible tubes called catheters are inserted into a vein, usually in the groin, and guided gently up to the heart. These catheters have electrodes on the tips. Once inside the heart, they act like microscopic microphones, recording the electrical activity from the inside. This allows the doctor to create a detailed “map” of the electrical pathways.
The doctor can also use the catheters to send small, safe electrical signals to the heart to try and trigger the arrhythmia. This is done in a controlled environment. By inducing the arrhythmia, they can see exactly where it starts. The result confirms the diagnosis and often allows the doctor to treat the problem immediately during the same procedure, such as by cauterizing the tiny area of tissue causing the short circuit.
Send us all your questions or requests, and our expert team will assist you.
No, an ECG is completely painless. It involves sticking small patches on your skin. There are no needles, and you do not feel any electricity.
It depends on the type of monitor. Most traditional Holter monitors cannot get wet, so you cannot shower with them. Newer patch monitors are often water-resistant, but you should always ask your nurse first.
Stress tests are very safe. They are performed by trained professionals who monitor your heart continuously. If there is any sign of danger or if you feel too unwell, the test is stopped immediately.
A urethral diverticulum is a pocket or pouch that forms in the wall of the urethra. It acts like a trap for urine. Because the urine in the pouch doesn’t empty properly, it can become infected or form stones. It is most common in women and can cause pain during intercourse or dribbling of urine after voiding.
An EPS is used when doctors need a very precise look at the heart’s electrical wires, usually to plan a procedure or when other tests haven’t found the cause. It provides the most detailed information possible.


Atrial fibrillation, or AFib, is a heart condition that makes your heartbeat irregular. It affects millions of people worldwide. This condition is a big risk


Atrial fibrillation (AFib) is a common heart condition in the U.S. It can lead to serious problems if not treated quickly. 1 in 4 adults

Did you know that atrial fibrillation, a type of irregular heartbeat, can strike anyone? Even a WWE Hall of Famer like Diamond Dallas Page can

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)