Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
Grade 1 gynecomastia represents the mildest form of the condition, characterized by a small, localized button of glandular tissue concentrated beneath the areola. There is no excess skin involved, and the chest contour remains relatively flat outside the immediate nipple area. This is often referred to as “puffy nipple” syndrome.
The physical indication for surgery here is the protrusion of the nipple-areola complex, which can be visible through thin clothing. Patients often complain of sensitivity or tenderness in this localized area. The surgical approach is typically a minimal incision periareolar excision to remove the disc of tissue.

Grade 2 gynecomastia involves a more diffuse enlargement of the breast that extends beyond the areolar borders. The chest appears fuller, resembling a small female breast. Importantly, in Grade 2, there is still no significant excess skin; the skin elasticity is sufficient to retract after tissue removal.
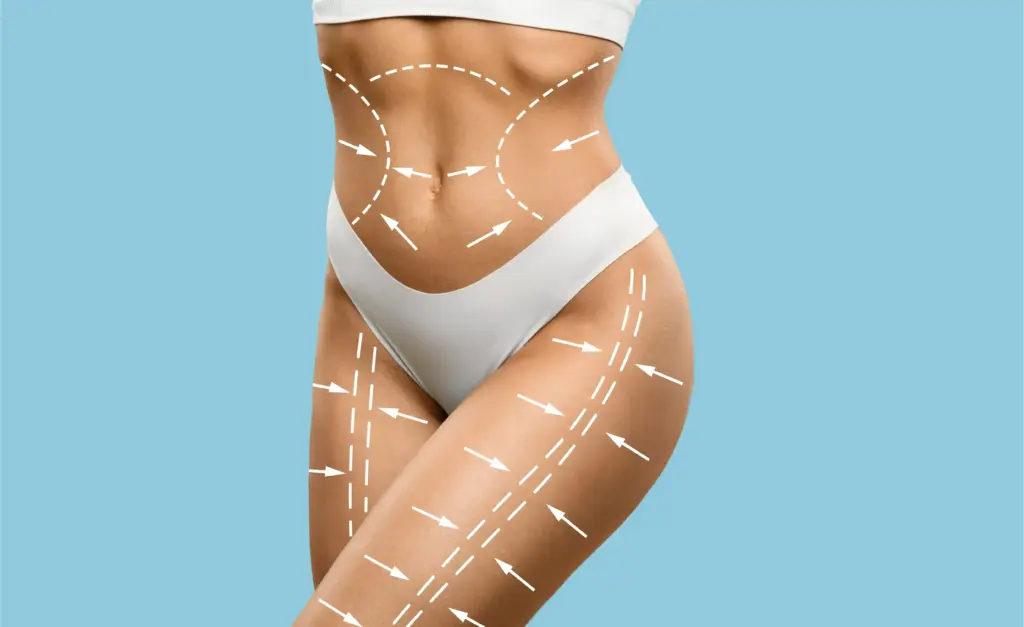
This grade typically involves a mix of both glandular tissue and fatty deposits. The physical indication is a softening of the pectoral definition and a rounded lower chest contour. Treatment requires a combination of aggressive liposuction to feather the edges and direct excision to remove the central gland.

Grade 3 marks the transition where skin management becomes a critical factor. The breast enlargement is moderate to severe, similar to Grade 2, but the stretched, sagging skin (ptosis) has been pulled down by the increased tissue weight. The nipple may sit lower on the chest wall.
The physical indication here is a visible fold or droop in the breast tissue. Simply removing the fat and gland would leave an empty, hanging skin sac. Therefore, the procedure must include techniques to tighten the skin or excise a small amount of skin to ensure a flat contour.
Grade 4 gynecomastia is the most severe presentation, often resembling a mature female breast. There is significant glandular and fatty volume, combined with a large amount of excess, hanging skin. The nipple-areola complex is often enlarged and displaced downwards.
This condition is physically debilitating and requires a reconstructive approach similar to a mastectomy or breast reduction. The physical indication is a massive tissue volume that obscures the entire male chest anatomy. Surgical correction involves extensive skin resection, free nipple grafting, or complex flap techniques.

Gynecomastia does not always present symmetrically. Many patients experience unilateral gynecomastia, where only one breast is enlarged, or asymmetric gynecomastia, where one side is significantly larger than the other. This creates a noticeable imbalance in the chest wall.
The physical indication is a visual discrepancy in chest volume. This can cause severe distress and difficulty fitting clothing. The surgical challenge lies in achieving symmetry, often requiring different amounts of tissue removal and other techniques for the left and right sides to match the underlying muscle.
A significant portion of gynecomastia cases begin during puberty due to hormonal fluctuations. While many resolve spontaneously, some persist into adulthood. This type of gynecomastia is often characterized by dense, fibrous glandular tissue that has been present for years.
The biological cause is an imbalance in the estrogen-testosterone ratio during development. The persistent glandular tissue becomes fibrotic over time, making it unresponsive to medical therapy. Physical indications include a rubbery firmness under the nipple that has been stable since the teenage years.
Send us all your questions or requests, and our expert team will assist you.

Anabolic steroid use is a prevalent cause of gynecomastia in the bodybuilding community. Exogenous testosterone is converted to estrogen by the body (aromatization), leading to rapid, aggressive glandular growth. These glands are often densely vascular and fibrous.
The physical indication is a hard, painful lump under the nipple in an otherwise muscular individual. The gland sits atop a well-developed pectoral muscle, making it very prominent. Treatment involves excision, but recurrence is a risk if steroid use continues without estrogen blockers.
Numerous medications can trigger gynecomastia as a side effect. These include anti-androgens, certain heart medications, antidepressants, and ulcer drugs. The biological mechanism involves disrupting the hormonal balance or increasing prolactin levels.
The physical indication is the onset of breast tenderness and enlargement shortly after starting a new medication. While stopping the medication may halt growth, the established fibrous tissue often requires surgical removal to restore the chest contour.
After massive weight loss, patients are often left with a combination of residual resistant fat and loose skin in the chest area. This presents a unique functional and aesthetic challenge. The breast tissue may appear deflated or ptotic.
The physical indication is a “deflated” look with skin folds that may cause chafing or irritation. The surgical focus is heavily weighted towards skin tightening and excision to redrape the chest skin over the more petite body frame.
A specific physical indication found in many patients is the “rubber disc.” This is a concentrated, circular mass of glandular tissue located strictly behind the areola. It feels distinct from the surrounding soft fat, often described as a golf ball or hockey puck.
This distinct demarcation makes liposuction alone ineffective, as the cannula cannot penetrate or break down the disc. The physical presence of this disc is the primary indication for the open excision component of the surgery.
In many cases of gynecomastia, the constant pressure of the underlying gland stretches the areolar skin, making the areola appear larger than usual. This expansion can also lead to herniation, where the areola bulges outward.
The physical indication is an areola diameter exceeding the standard male norm (typically 28-30mm) and a lack of a flat contour. Surgery aims to reduce the diameter of the areola by either relieving underlying pressure or performing a direct donut-lift excision.
While gynecomastia is often asymptomatic, a subset of patients experiences physical pain (mastodynia) or hypersensitivity. This is particularly common in rapid-onset cases or steroid-induced gynecomastia. The nipples may be painful to the touch or chafe against clothing.
This functional issue can limit physical activity and cause daily discomfort. Surgical removal of the glandular tissue eliminates the source of the pain and resolves the hypersensitivity, providing functional relief alongside aesthetic improvement.
The Grade (1-4) is a medical classification system used to describe the severity of the condition. It helps surgeons decide which technique to use. Grade 1 is small and localized, while Grade 4 is large and may require excess skin to be removed, requiring more complex surgery.
Anabolic steroids increase testosterone levels. The body tries to balance this by converting excess testosterone into estrogen via the enzyme aromatase. This high level of estrogen stimulates breast tissue growth, just like in female puberty.
Gynecomastia on only one side is usually benign, but it warrants a more thorough workup. In rare cases, a unilateral lump can be a sign of male breast cancer. Your surgeon will likely recommend an ultrasound or mammogram to rule this out before surgery.
The surgery removes the tissue pushing the nipple out, which usually shrinks the areola significantly as the skin retracts. If the areola is still too large, the surgeon can perform a physical reduction to reduce its diameter.
You can, but the results are best if you are near your ideal weight. Visceral fat (fat inside the belly) and generalized obesity can mask the results of chest surgery. Surgeons typically recommend a BMI under 30-32 for safety and optimal aesthetics.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)