Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.

To ensure a precise diagnosis, surgeons often utilize ultrasound imaging during the consultation. High-frequency ultrasound allows the surgeon to visualize the depth and density of the glandular tissue versus the subcutaneous fat. This “look beneath the skin” confirms the diagnosis without invasive measures.
In cases where the mass is unilateral, rigid, or fixed, a mammogram may be ordered to rule out male breast cancer. This safety protocol ensures that any suspicious pathology is identified and managed appropriately before cosmetic intervention.

The physical examination involves specific tactile maneuvers, most notably the “pinch test.” The surgeon pinches the tissue beneath the areola to assess its thickness and consistency. A firm, rubbery resistance indicates glandular tissue, while soft, pliable tissue indicates fat.
The surgeon also assesses skin elasticity by pulling the skin and watching its recoil. This determines whether the skin will snap back after tissue removal or if skin excision will be necessary. This assessment prevents post-operative skin laxity and ensures a tight contour.
Gynecomastia is often a symptom of an underlying hormonal imbalance. Therefore, a comprehensive endocrine workup is standard preparation. Blood tests are ordered to measure levels of Testosterone (total and free), Estrogen (Estradiol), Prolactin, LH, and FSH.
This profile helps rule out systemic causes such as hypogonadism, pituitary tumors, or thyroid dysfunction. Treating the underlying hormonal issue is essential before surgery to ensure the safety of the patient and to prevent the regrowth of tissue post-operatively.

Modern consultations leverage 3D imaging technology (such as Vectra) to create a digital avatar of the patient. This allows the surgeon to simulate the surgical outcome, showing the patient what their chest will look like after being flattened.
This tool is invaluable for managing expectations. It helps the patient visualize the reduction in projection and the definition of the pectoral muscles. It also allows for the discussion of potential asymmetry and scar placement on a 3D model of the patient’s own body.
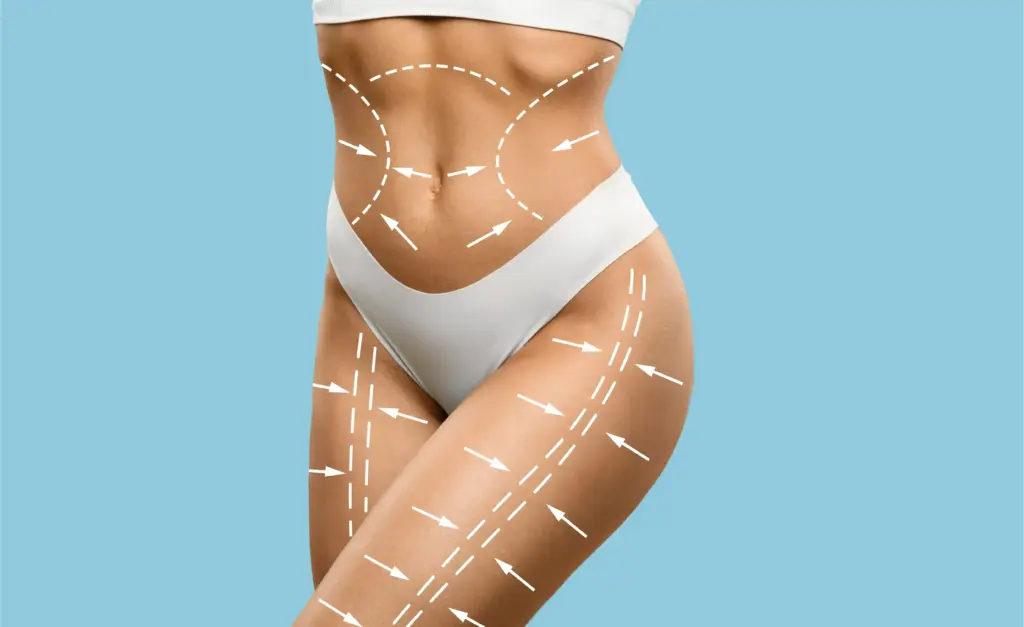
Weight stability is a prerequisite for surgery. Patients are advised to be at or near their ideal body weight for at least six months before the procedure. Significant weight fluctuations after surgery can alter the results, leading to loose skin or recurrent fatty deposits.
Surgeons typically require a BMI under 30 or 32 to minimize surgical risks and optimize aesthetic outcomes. If a patient is actively losing weight, surgery is postponed until the weight has stabilized to allow for an accurate assessment of the skin envelope.
Send us all your questions or requests, and our expert team will assist you.

Nicotine is a potent vasoconstrictor that impairs blood flow to the skin, specifically the nipple-areola complex. In gynecomastia surgery, where the skin is undermined and thinned, adequate blood supply is critical for healing. Smoking increases the risk of nipple necrosis (tissue death) and wound dehiscence.
A strict zero-tolerance policy is enforced. Patients must cease all nicotine products vapes, patches, gum, and cigarettes for at least 4 weeks before and after surgery. Urine cotinine tests may be used to verify compliance to ensure patient safety.
A thorough review of all medications is conducted. Blood-thinning medications, including aspirin, ibuprofen, and certain herbal supplements (Fish Oil, Vitamin E, Garlic), must be paused 2 weeks before surgery to prevent hematoma (blood collection).
Patients using anabolic steroids must stop their cycle significantly in advance of the surgery. Continued steroid use increases the risk of bleeding and complications during anesthesia. The surgeon provides a specific protocol for tapering or stopping these substances.
The consultation includes a screening for Body Dysmorphic Disorder (BDD). Patients with BDD may have distorted perceptions of their bodies that surgery cannot fix. The surgeon assesses the patient’s motivations and ensures they have realistic expectations of the outcome.
The surgeon also evaluates the patient’s emotional readiness for the recovery period. Understanding the temporary swelling, the need for a compression vest, and the gradual reveal of results is crucial for a positive psychological experience.
To minimize infection risk, patients are instructed to use an antibacterial soap (like Hibiclens) for several days before surgery. The chest area should be kept clean and free of rashes or active acne.
If there is excessive chest hair, the patient may be asked to trim it with clippers (not a razor) a few days before surgery to improve visualization and dressing adhesion. Shaving with a razor is avoided immediately before surgery to prevent micro-cuts that could harbor bacteria.
The patient is measured for a medical-grade compression vest during the pre-op visit. This vest is a critical component of the surgery, acting as an external mold to press the skin against the chest wall and prevent fluid buildup.
Logistics for the day of surgery are finalized, including arranging for a responsible adult to drive the patient home and stay with them for the first 24 hours. Instructions on fasting (NPO) and clothing choices for surgery day are provided.
If your blood work shows abnormal hormone levels (like very high prolactin or very low testosterone), your surgeon will refer you to an endocrinologist. This is to treat the root cause of the imbalance before we perform the cosmetic correction.
If you have true gynecomastia (glandular tissue), liposuction alone will not work. The gland is too dense to be sucked out. Leaving the gland behind results in a “donut” effect where the fat is gone but the nipple still protrudes.
Marijuana can affect how much anesthesia you need and can irritate your lungs. It is best to stop smoking at least 2 weeks before surgery. Edibles should also be avoided close to the surgery date to prevent interactions with anesthesia drugs.
Absolutely not. Gynecomastia surgeons see this condition every single day. The environment is professional, private, and non-judgmental. The goal is to help you feel comfortable in your body, starting from the very first meeting.
You should trim your chest hair with electric clippers about 2-3 days before surgery. Please do not use a razor blade right before surgery, as it can cause tiny cuts that may become infected. We need the area to be hair-free enough for bandages to stick.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)