Cardiology is the medical specialty focused on the heart and the cardiovascular system. It involves the diagnosis, treatment, and prevention of conditions affecting the heart and blood vessels. These conditions include coronary artery disease, heart failure, arrhythmias (irregular heartbeats), and valve disorders. The field covers a broad spectrum, from congenital heart defects present at birth to acquired conditions like heart attacks.
Send us all your questions or requests, and our expert team will assist you.
Surgery provides a new beginning, not a panacea. While cardiothoracic surgery can address the immediate mechanical problem, it does not remove the underlying tendency for disease. If the habits that caused the problem in the first place do not change, they can return. Therefore, the post-surgery phase is about embracing a new lifestyle. This stage is often the hardest part for patients, but also the most rewarding.
Prevention is also key for those who have not had surgery but are at risk. The same rules apply: protect your heart and lungs. Living a heart-healthy life does not mean giving up everything you love. It means making smarter choices, finding balance, and prioritizing your well-being. This section outlines the practical steps patients can take to protect their surgical investment and enjoy their renewed health.

Food is fuel, and the quality of that fuel matters. After surgery, patients are often advised to follow a diet similar to the Mediterranean diet, which is rich in fruits, vegetables, whole grains, and lean proteins. The goal is to reduce the buildup of plaque in the arteries and keep blood pressure stable.
Salt holds onto water in the body. For someone with a heart condition, excess water increases blood pressure and strains the heart. Patients are taught to read labels and avoid processed foods like canned soups, cold cuts, and frozen dinners, which are often hidden salt bombs. Cooking at home using herbs and spices instead of salt is a major positive change.

Not all fats are bad. “Good” fats found in olive oil, avocados, and nuts are beneficial. However, saturated fats (found in red meat, butter, and cheese) and trans fats (found in fried foods) should be limited. These unhealthy fats raise cholesterol levels, which can clog the new bypass grafts or native arteries. Switching to skim milk and choosing chicken or fish over steak are simple, effective swaps.
Movement is medicine. After the initial recovery period, regular exercise is essential for strengthening the heart muscle and improving lung capacity. The heart is a muscle, and like any muscle, it gets stronger with use. Exercise also helps lower blood pressure, control weight, and improve mood.
Patients should aim for at least 150 minutes of moderate activity per week. This sounds like a lot, but it breaks down to just 30 minutes a day, five days a week. Walking is the best and safest exercise for most cardiac patients. It requires no equipment and can be done anywhere. Once the surgeon approves, gardening, swimming, and cycling are also excellent options. The key is consistency rather than intensity. Slow and steady wins the race.
It is very common to feel emotional after chest surgery. Many patients experience “cardiac blues” or even depression. The physical trauma of surgery, combined with the realization of one’s mortality, can be a heavy burden. Stress also releases hormones that increase heart rate and blood pressure, which is not good for a healing heart.
Managing mental health is as important as caring for the physical incision. Techniques like deep breathing, meditation, and gentle yoga can lower stress levels. Staying connected with friends and family prevents isolation. If feelings of sadness persist, talking to a therapist or joining a support group for heart patients can be incredibly helpful. A positive mindset has been proven to aid in physical recovery.
After surgery, patients are usually sent home with several new prescriptions. These might include blood thinners to prevent clots, statins to lower cholesterol, beta-blockers to slow the heart rate, and medications to control blood pressure. It can be overwhelming to manage this new routine.
However, taking these medications exactly as prescribed is non-negotiable. They are the chemical bodyguards protecting the surgical repair. Stopping a blood thinner suddenly, for example, could lead to a stroke. Using a pill organizer box, setting alarms on a phone, or using a smartphone app can help track doses. Patients should never stop or change a dose without talking to their doctor first.
If you smoke, the single most important thing you can do for your survival is to stop. Continuing to smoke after heart or lung surgery drastically increases the risk of complications, infection, and death. Smoking causes blood vessels to constrict and promotes clotting. For lung patients, it directly damages the remaining lung tissue.
Quitting is hard, but help is available. Nicotine patches, gums, and prescription medications can reduce cravings. Avoidance is also important staying away from secondhand smoke and environmental toxins like heavy pollution or harsh chemical fumes protects the lungs. Your surgeon and primary care doctor can provide resources and support to help you quit for good.
Surgery is not a “fix it and forget it” event. It is the beginning of a lifelong relationship with your medical team. Regular checkups are essential to monitor the success of the surgery and catch any new issues early. You will likely see your cardiologist once or twice a year for the rest of your life.
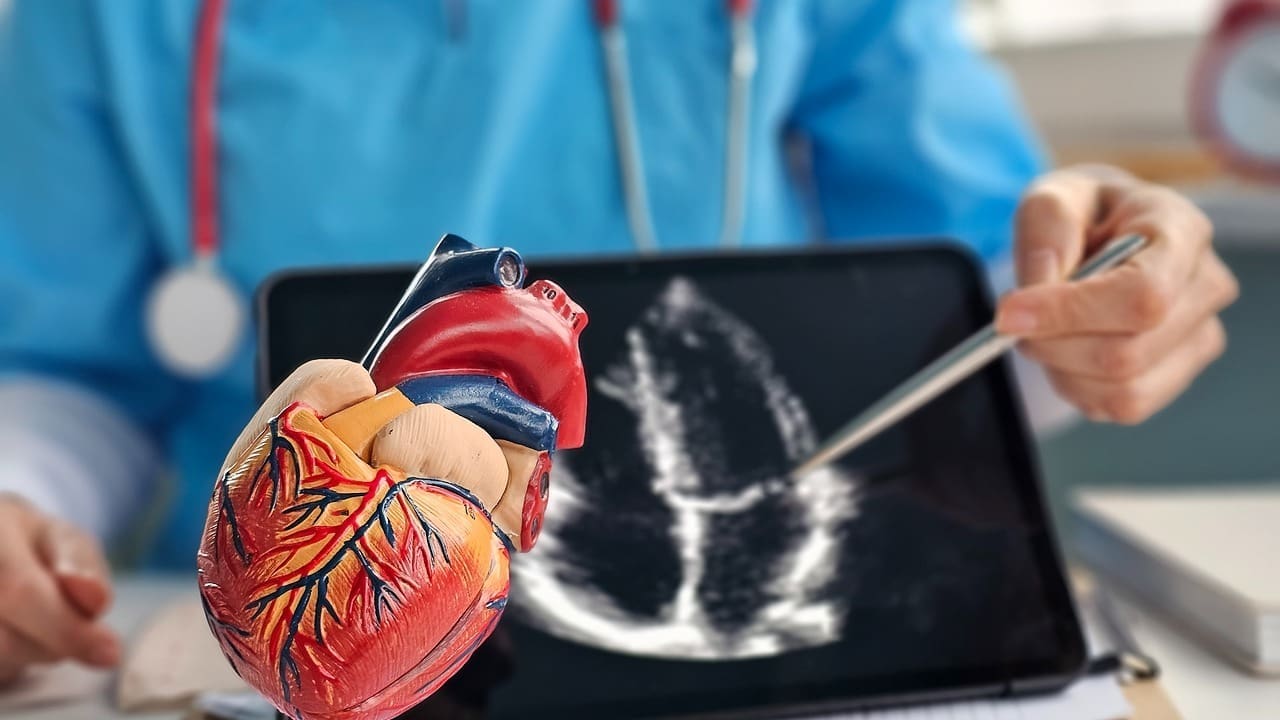
During these visits, you might have repeat EKGs or echocardiograms to ensure the valves are working and the heart function is stable. Blood tests will check your cholesterol and kidney function. These visits are opportunities to adjust medications and discuss any new symptoms. Staying engaged in your care and keeping these appointments is the best insurance policy for your health.

Send us all your questions or requests, and our expert team will assist you.
Yes. A heart-healthy diet is about balance, not total deprivation. You can enjoy a treat occasionally, perhaps for a special occasion, as long as your daily habits are healthy. Moderation is the key.
Likely, yes. You might reduce some medications over time, but drugs like aspirin or statins are typically lifelong therapies to prevent future disease.
Generally, yes, once you have recovered. A common rule of thumb is that if you can walk up two flights of stairs without gasping for breath or having chest pain, you are physically ready for sexual activity. Always check with your doctor first.
You should be able to talk while you exercise. If you are too breathless to speak a sentence, you are pushing too hard. Pain, dizziness, or extreme fatigue are signs to stop immediately.
If you miss a dose, take it as soon as you remember, unless it is almost time for the next one. Never double up on doses to “catch up.” If you are unsure, call your pharmacist for advice.


At Liv Hospital, we know how vital anticoagulant therapy is. It stops blood clots that could cause serious issues. These include deep vein thrombosis (DVT),
At Liv Hospital, we know how vital anticoagulant medications are. They help prevent strokes, heart attacks, and pulmonary embolisms. For people with certain health issues,

A blood clot in the arm is a serious issue called upper extremity deep vein thrombosis (UEDVT). It’s important to spot the signs early because

At Liv Hospital, we know how vital it is to stop dangerous blood clots. These clots can cause heart attacks, strokes, and other heart problems.
At Liv Hospital, we know how vital it is to know about medications that prevent and treat dangerous blood clots. We focus on our patients,

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)