Plastic surgery restores form and function through reconstructive procedures, cosmetic enhancements, and body contouring.
Send us all your questions or requests, and our expert team will assist you.
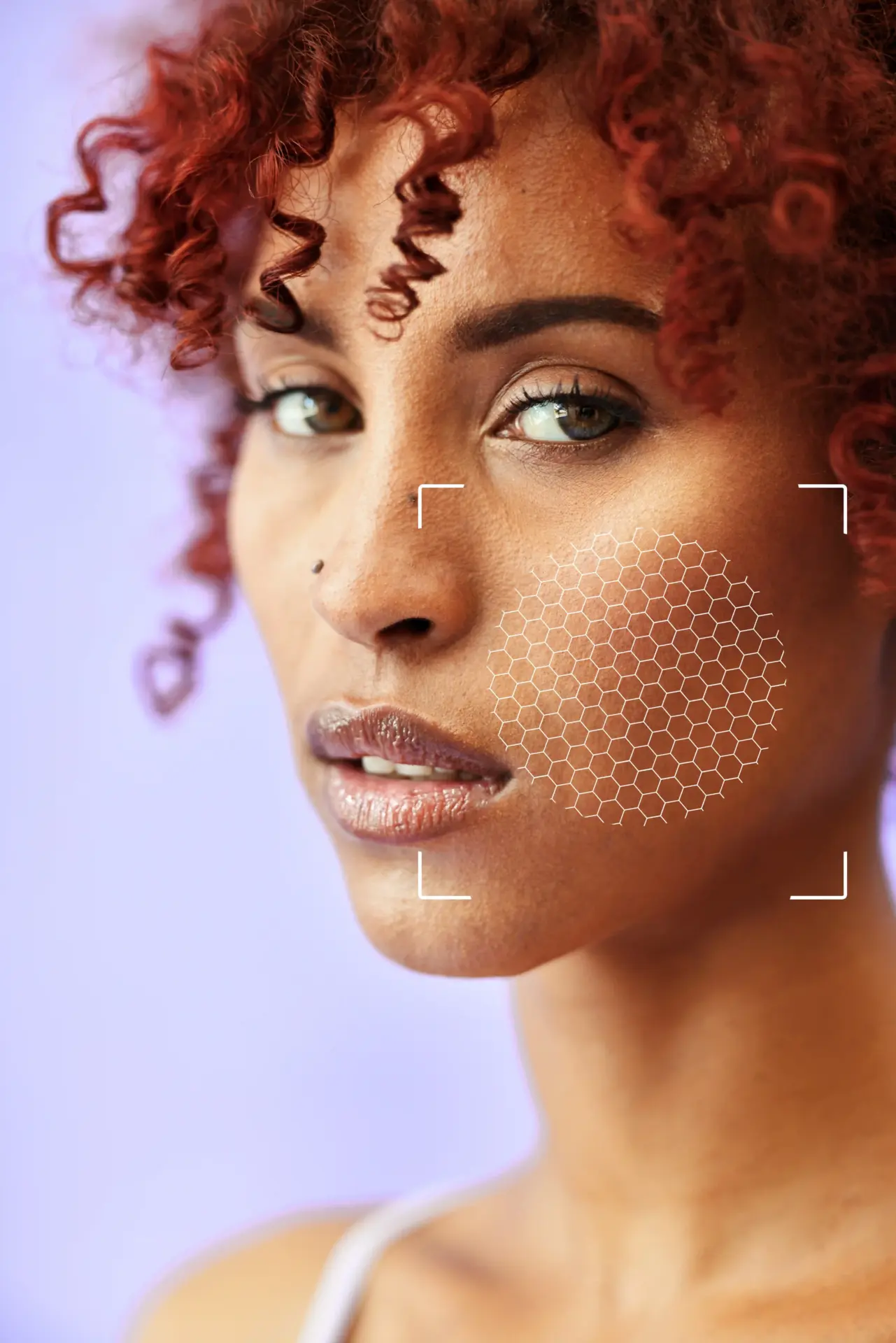
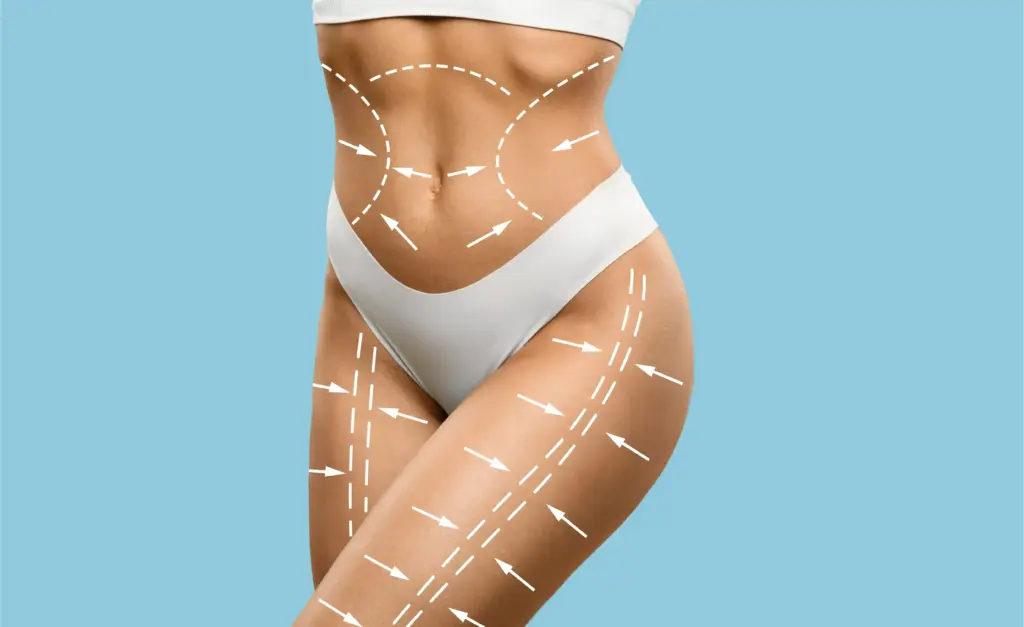
The consultation process begins with a comprehensive physical assessment. The surgeon evaluates the quality of the abdominal skin, checking for elasticity and the presence of stretch marks. This determines how well the skin will drape after fat removal.
The surgeon palpates the abdomen to assess the rectus diastasis (muscle separation). The patient may be asked to crunch or flex their abs to reveal the extent of the bulge. This physical exam dictates whether muscle repair is needed and to what extent.

A critical part of the examination is distinguishing between subcutaneous and visceral fat. Surgeons cannot suction visceral fat (fat around the organs). If a patient has a protruding, hard, firm belly, it is likely visceral fat.
In such cases, the surgeon will advise weight loss before surgery. Performing a tummy tuck on a patient with high visceral fat can lead to poor aesthetic results and respiratory compromise, as the tightened muscles press against the internal bulk.

A thorough review of the patient’s medical history is mandatory. The surgeon looks for conditions that impair healing, such as diabetes, connective tissue disorders, or autoimmune diseases. History of blood clots (DVT/PE) is a significant safety concern.
The surgeon also reviews all medications and supplements. Blood thinners, anti-inflammatories, and certain herbal supplements must be stopped weeks before surgery to prevent hematoma. Previous abdominal surgeries are noted to map out scar tissue and vascular supply.
Nicotine is a potent vasoconstrictor that reduces blood flow to healing tissues. In a tummy tuck, the skin flap relies on microscopic vessels for survival. Smoking can cause skin necrosis (death of the skin), leading to massive open wounds.
Surgeons enforce a strict zero-tolerance policy for nicotine. Patients must stop smoking, vaping, or using patches for at least 4 to 6 weeks before and after surgery. Urine tests for nicotine metabolites are often administered to verify compliance.

Patients are advised to be at a stable, maintainable weight for at least 6 months before surgery. Fluctuating weight can compromise the results. If a patient loses significant weight after surgery, loose skin may return. If they gain weight, the repair can be stretched.
The surgeon calculates the Body Mass Index (BMI). While there is no universal cutoff, many surgeons prefer a BMI under 30 or 32 for optimal safety and results. Higher BMIs are associated with increased risks of infection and wound healing issues.
Good nutrition is essential for wound healing. Patients are encouraged to adopt a high-protein diet in the weeks leading up to surgery. Protein provides the building blocks for tissue repair and collagen formation.
Hydration is also emphasized. Patients should drink plenty of water and avoid alcohol, which dehydrates the body and can interfere with anesthesia. Some surgeons prescribe specific vitamin regimens (such as Zinc and Vitamin C) to boost the immune system.
Send us all your questions or requests, and our expert team will assist you.

Elective surgery requires a stable mental state. The surgeon assesses the patient’s motivations and expectations. Patients should desire the surgery for themselves, not to please others.
The recovery from a tummy tuck is physically demanding. Patients must be mentally prepared for downtime, discomfort, and a temporary loss of independence. A strong support system at home is verified during the consultation.
For female patients, future pregnancy plans are a vital topic. While a tummy tuck does not prevent pregnancy, a future pregnancy will stretch the repaired muscles and skin, effectively undoing the results of the surgery.
Surgeons strongly advise waiting until the patient is sure they are done having children. This ensures the longevity of the investment and avoids the need for revision surgeries later.
Standard pre-operative tests are ordered to ensure the patient is fit for anesthesia. This includes blood work (CBC, metabolic panel, coagulation profile) and sometimes an EKG for heart health.
For patients with a history of hernias, an abdominal ultrasound or CT scan may be ordered to map the defect. This allows the surgeon to plan a concurrent hernia repair if necessary.
Patients receive detailed instructions on preparing their home for recovery. This includes setting up a sleeping area where they can maintain a flexed position (like a recliner) to take tension off the incision.
Arrangements for childcare, pet care, and household chores must be made. Patients will not be able to lift heavy objects or drive for several weeks. Prescriptions for pain management and antibiotics are filled in advance.
The consultation includes a transparent breakdown of costs, including surgeon fees, anesthesia, facility fees, and garment costs. Since this is cosmetic surgery, insurance generally does not cover it unless a documented hernia repair is performed.
Financing options and deposit schedules are reviewed. The administrative team ensures the patient understands the financial commitment and the cancellation policies.
Patients are encouraged to bring photos of their desired results (“wish pics”) to help the surgeon understand their aesthetic goals. However, the surgeon manages expectations by explaining what is achievable based on the patient’s specific anatomy.
The goal is to align the patient’s vision with surgical reality. The surgeon explains trade-offs, such as scar length versus contour improvement, ensuring informed consent.
Ideally, yes. You should be within 10 to 15 pounds of your goal weight. Losing weight after surgery can cause the skin to loosen again, compromising the result. Surgery is for contouring, not weight loss.
Yes, it is medically safe to get pregnant. However, the baby’s growth will stretch the skin and muscles again, likely reversing the flat stomach you achieved. It is best to wait until you are done having children.
You cannot have this surgery if you smoke. Smoking constricts blood vessels and will cause the skin of your tummy to turn black and die (necrosis). You must quit all nicotine 6 weeks before and after.
Generally, no. A tummy tuck is considered cosmetic. However, if you have a hernia that needs repair, insurance might cover the hernia portion of the surgery, but not the skin removal or liposuction.
Most patients need 2 to 3 weeks off work. If you have a desk job, you might return sooner, but you will be tired and sore. If you have a physical job, you may need 4 to 6 weeks.


Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)