Last Updated on November 26, 2025 by Bilal Hasdemir
Cancer diagnosis and treatment have made big strides. Yet, the first step often relies on a key tool: ultrasound technology. Oncologist ultrasound examinations play a crucial role in this process. It’s interesting to know that almost half of cancer patients undergo some form of ultrasound testing during their treatment.
Getting a cancer diagnosis can be tough. But, early detection and monitoring are key for good treatment. Ultrasound is a big help here, giving a non-invasive way to find and watch different cancers.
Using ultrasound for cancer detection, doctors can keep a close eye on the disease and how well treatments work. This helps make better choices and gives patients a better idea of what’s going on with their health.
Key Takeaways
- Ultrasound is a critical diagnostic tool in oncology.
- It aids in the detection and monitoring of various cancers.
- Non-invasive and effective, ultrasound supports informed treatment decisions.
- Regular use can help track the progression of cancer and treatment efficacy.
- Patients benefit from a clearer understanding of their condition through ultrasound monitoring.
The Role of Imaging in Cancer Care
Imaging technologies have changed cancer care a lot. They give oncologists key info for managing patients. Imaging is key for diagnosing, staging, and tracking cancer treatment.
Importance of Accurate Diagnosis
Getting a cancer diagnosis right is very important. Tools like ultrasound, CT scans, and MRI help oncologists see tumors. This info is key for knowing the cancer type and stage, which helps decide treatment.
How well a cancer treatment works depends on a good diagnosis. With clear images, doctors can find tumors’ exact location and size. This helps in planning treatment and checking how well it’s working.
The Oncologist’s Imaging Toolkit
Oncologists use many imaging tools, each with its own benefits. Ultrasound is good for looking at surface structures and guiding biopsies. CT scans and MRI give detailed views of the body, helping to see how far tumors have spread.
We use these tools to make treatment plans that fit each patient. By mixing different imaging methods, we get a full picture of the tumor. This helps us stage cancer right and plan effective treatments.
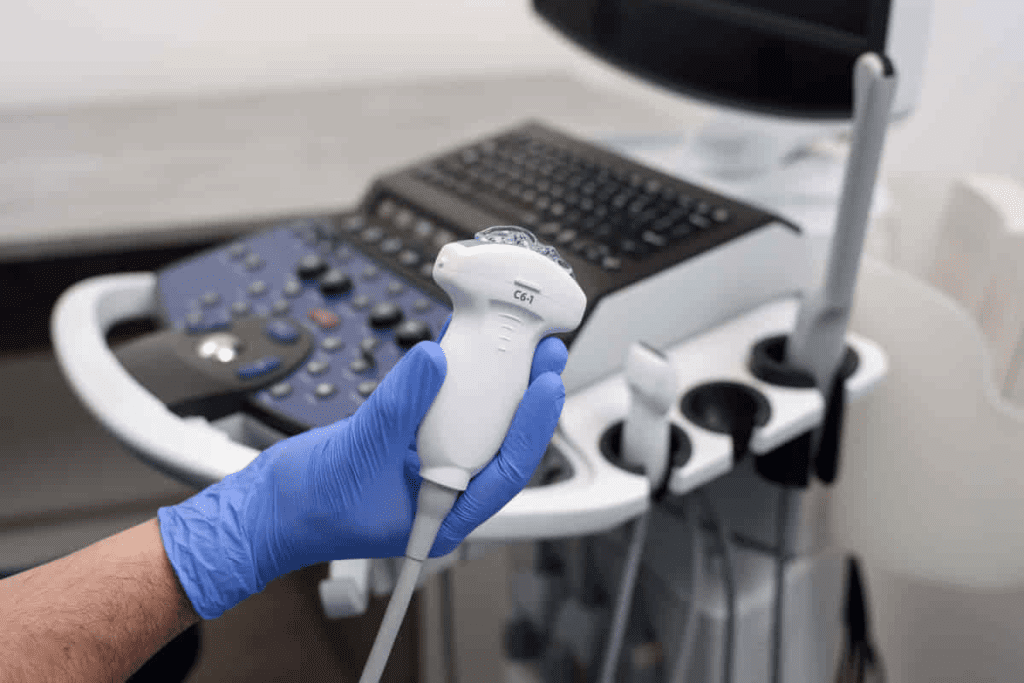
Understanding Ultrasound Technology in Oncology
Ultrasound technology is key in oncology, helping us diagnose and track cancer without surgery. It uses sound waves to show us what’s inside the body. This is great for guiding biopsies and checking how tumors are doing.
How Ultrasound Works
Ultrasound sends high-frequency sound waves into the body with a probe called a transducer. These sound waves bounce back and are caught by the transducer. This creates images on a screen in real-time.
Key components of ultrasound technology include:
- The transducer, which converts electrical energy into sound waves and vice versa.
- Advanced signal processing algorithms that enhance image quality.
- Real-time imaging capabilities that allow for dynamic assessment of tissues and organs.
Advantages and Limitations
Ultrasound has big pluses in oncology, like being non-invasive and not using harmful radiation. It also lets us see things in real-time. But, it has downsides like needing skilled operators and not seeing as deep as other methods.
| Advantages | Limitations |
| Non-invasive and safe | Operator-dependent |
| Real-time imaging | Limited depth penetration |
| No ionizing radiation | May not be suitable for all tissue types |
Even with its downsides, ultrasound is a big help in fighting cancer. It gives us important info for planning treatments and checking on tumors. Knowing its strengths and weaknesses helps us use it better in cancer care.
Primary Reasons Oncologist Ultrasound Procedures Are Ordered
Oncologists use ultrasound for key reasons in cancer treatment. It’s a non-invasive way to diagnose, stage, and monitor cancer. This technology is vital in oncology.
Initial Cancer Detection
Ultrasound is a key tool for early cancer detection, especially for organs like the breast, ovaries, and liver.Finding tumors early is key for good treatment plans.
In breast cancer, ultrasound helps with mammograms, mainly for women with dense breasts. It tells the difference between solid masses and cysts. This info is important for more tests.
Staging and Treatment Planning
After finding cancer, ultrasound helps with staging and planning treatment. It shows how far the tumor has spread. Knowing this helps pick the best treatment.
| Cancer Type | Ultrasound Role in Staging | Impact on Treatment Planning |
| Breast Cancer | Assesses tumor size and lymph node involvement | Guides surgical and radiation therapy decisions |
| Ovarian Cancer | Evaluates tumor extent and metastasis | Influences surgical planning and chemotherapy |
| Liver Cancer | Determines tumor size and location | Affects surgical resection and ablation planning |
Monitoring Treatment Response
Ultrasound also checks how well treatment is working. It looks at tumor size and changes. This is important for improving patient results.
For example, during chemo, ultrasound checks if tumors are getting smaller. It shows if the treatment is working well.
Ultrasound vs. Other Imaging Modalities in Cancer Care
Imaging is key in fighting cancer. Knowing the differences between imaging types helps doctors. We use these methods to find, check, and track cancer. Here, we look at how ultrasound compares with other imaging in cancer care.
Ultrasound vs. CT Scan for Cancer
CT scans and ultrasound help find cancer. CT scans give detailed views of cancer spread. But, they use radiation and might not be safe for everyone.
Ultrasound is safe and doesn’t use radiation. It’s better for some patients, like pregnant women.
- Advantages of Ultrasound over CT Scan:No radiation exposure
- Real-time imaging capability
- Cost-effective
- Limitations of Ultrasound compared to CT Scan:Less detailed images for certain areas
- Operator-dependent
Ultrasound vs. MRI in Oncology

MRI gives detailed images without radiation. Ultrasound is portable and cheaper than MRI. It’s good for quick checks and procedures.
But, MRI shows more about soft tissues.
- When to Choose Ultrasound over MRI:For initial screening or bedside assessment
- For guiding biopsies or other interventions
- In situations where MRI is contraindicated
When Ultrasound Is Preferred
Ultrasound is best in some cases. It’s great for checking superficial areas like thyroid nodules or breast lesions. It’s also good for guiding procedures like biopsies or drain placements.
- Key scenarios where ultrasound is preferred:
- Superficial lesion assessment
- Guiding interventional procedures
- Patients with contraindications to other imaging modalities
Ultrasound for Breast Cancer Detection and Monitoring
Ultrasound is key in finding and tracking breast cancer early. It’s a non-invasive method that gives insights into breast issues. It works well with other tools like mammograms.
Supplementing Mammography
Mammograms are the main tool for breast cancer screening. But, they can miss cancers in dense breasts. Ultrasound for breast cancer detection helps find these hidden cancers.
Research shows ultrasound can find more cancers in dense breasts. It’s safe and helps see breast health clearly when mammograms are unsure.
Monitoring Breast Tumors
After finding breast cancer, ultrasound-guided biopsies are key. They help see how big and what kind of tumors are. This info is vital for planning treatment.
Ultrasound also checks if tumors are shrinking during treatment. This helps doctors adjust treatment plans for better results.
Ultrasound-Guided Breast Biopsies
Ultrasound-guided breast biopsies are a major tool in fighting breast cancer. They use ultrasound to guide the needle to the right spot. This way, they get precise tissue samples.
| Procedure | Description | Benefits |
| Ultrasound-Guided Biopsy | Uses ultrasound imaging to guide the biopsy needle | High precision, minimally invasive |
| Mammography-Guided Biopsy | Uses mammography imaging to guide the biopsy needle | Effective for calcified lesions |
| Surgical Biopsy | Surgical removal of tissue for examination | More invasive, used when other methods are inconclusive |
The use of breast cancer screening with ultrasound and biopsies has greatly helped in fighting breast cancer. Ultrasound gives detailed images and guides procedures. It’s a vital tool in the fight against breast cancer.
Ultrasound Applications in Gynecologic Oncology
Ultrasound has greatly improved in gynecologic oncology. It helps us find and treat female reproductive cancers early. This technology boosts our ability to diagnose and treat patients better.
Ultrasound for Ovarian Cancer
Ultrasound is key in finding and managing ovarian cancer. It lets us see the ovaries and spot problems like cysts or tumors early. Using ultrasound for ovarian cancer helps us diagnose more accurately and act quickly.
We use different ultrasound methods, like transvaginal ultrasound, to get clear images of the ovaries. This helps us understand the size, shape, and details of ovarian masses. Knowing this is important for deciding how to treat the cancer.
Ultrasound for Pelvic Cancer Assessment
Ultrasound for pelvic cancer is also important for checking other gynecologic cancers, like cervical and endometrial cancers. It helps us see how far the cancer has spread and if it’s touching nearby tissues.
Ultrasound gives us live images. This helps us guide biopsies and other procedures. It makes our diagnoses and treatment plans more accurate.
Monitoring Gynecologic Cancer Treatment
Gynecologic cancer treatment monitoring is another big use of ultrasound in gynecologic oncology. We use it to see how tumors react to treatments like surgery, chemotherapy, or radiation.
By doing regular ultrasound checks, we can watch how tumors change. This lets us adjust treatment plans as needed. It helps us get the best results for our patients.
Abdominal Ultrasound in Oncology Practice
Abdominal ultrasound is key in oncology for spotting and tracking tumors in the belly. It helps us see different cancers in the belly area. This gives us important info for making a diagnosis, figuring out how far the cancer has spread, and planning treatment.
Liver and Pancreatic Cancer Assessment
Ultrasound is great for checking liver and pancreatic cancers. It lets us see tumors, measure their size, and check if they’ve spread. For liver cancer, it helps find tumors and guide biopsies. In pancreatic cancer, it helps see if the tumor can be removed and if there are any distant cancers.
Liver and Pancreatic Cancer Assessment Using Ultrasound
| Cancer Type | Ultrasound Role | Benefits |
| Liver Cancer | Detecting lesions, guiding biopsies | Non-invasive, real-time imaging |
| Pancreatic Cancer | Assessing tumor resectability, detecting metastases | Aids in staging and treatment planning |
Kidney and Adrenal Tumor Evaluation
Ultrasound is also vital for checking kidney and adrenal tumors. It helps tell if a tumor is bad or not, measures its size, and checks if it’s spread. For kidney tumors, it helps watch how big they get and if surgery is needed.
Gastrointestinal Cancer Imaging
In gastrointestinal cancer, ultrasound helps check how thick a tumor is, if lymph nodes have cancer, and if nearby areas are affected. It’s not as good as CT or MRI, but it’s a good first look. It also helps guide treatments.
We keep improving ultrasound tech to better diagnose cancer. By using ultrasound with other scans, we give patients the best care for belly cancers.
Ultrasound for Soft Tissue Cancer Evaluation
Ultrasound is key in oncology for checking soft tissue cancers. It helps us find and understand these cancers. This makes it easier to plan treatments.
Identifying Soft Tissue Masses
Ultrasound helps spot soft tissue masses. It shows us where they are and what they look like. This info is key for making treatment plans.
Soft tissue sarcomas are hard to spot because they are rare and can look different. Ultrasound helps us find them.
Differentiating Benign vs. Malignant Lesions
Telling if a soft tissue lesion is benign or malignant is important. Ultrasound looks at the lesion’s texture, edges, and blood flow. Malignant ones often have irregular edges and more blood flow.
By looking at these signs, we can guess if a lesion is cancerous. This helps us decide what tests to do next.
Monitoring Soft Tissue Sarcomas
Ultrasound is also great for watching how soft tissue sarcomas respond to treatment. We check how the tumor changes over time. This helps us change treatment plans if needed.
Ultrasound is a big help in caring for soft tissue cancer patients. It’s used from the start of diagnosis to after treatment.
Ultrasound-Guided Biopsies in Cancer Diagnosis
We use ultrasound-guided biopsies to get accurate tissue samples for cancer diagnosis. This method is key in oncology, helping to diagnose different cancers precisely.
Benefits of Real-Time Guidance
Ultrasound-guided biopsies offer real-time guidance. This means we can precisely target the tumor, lowering the chance of errors and improving accuracy. It also helps us avoid important structures, making the procedure safer for patients.
Types of Ultrasound-Guided Biopsies
There are several biopsies done under ultrasound, like fine-needle aspiration and core needle biopsies. The choice depends on the tumor’s location, size, and characteristics, and the patient’s health.
| Biopsy Type | Description | Advantages |
| Fine-needle Aspiration Biopsy | Uses a thin needle to collect cell samples. | Minimally invasive, quick recovery. |
| Core Needle Biopsy | Uses a larger needle to collect tissue samples. | Provides more tissue for analysis, helpful for diagnosing specific cancer types. |
What to Expect During the Procedure
During an ultrasound-guided biopsy, patients lie comfortably on a table. The area is cleaned and prepped, and a local anesthetic may be used to reduce pain. The ultrasound probe guides the biopsy needle to the target, and tissue samples are taken.
After the procedure, patients are watched for any immediate issues. The tissue samples are analyzed in a lab, and results come back in a few days to a week.
Using Ultrasound to Monitor Cancer Treatment Response
Ultrasound has changed how we watch cancer treatment work. It gives doctors real-time views of tumors. This helps them see if the treatment is working and make changes if needed.
Measuring Tumor Size Changes
Ultrasound is key in tracking tumor size changes. Regular ultrasound scans show if tumors are getting smaller, staying the same, or growing. This info helps doctors know if the treatment is working and if they should keep going or change it.
A study on breast cancer patients showed ultrasound can show early if treatment is working. This is important for making treatment plans better.
| Tumor Response | Ultrasound Findings | Clinical Implication |
| Complete Response | No detectable tumor | Continue monitoring, consider stopping treatment |
| Partial Response | Significant reduction in tumor size | Continue current treatment, monitor closely |
| Stable Disease | No significant change in tumor size | Re-evaluate treatment plan, consider alternative therapies |
| Progressive Disease | Tumor growth or new lesions | Modify treatment plan, consider more aggressive therapy |
Assessing Tumor Vascularity
Ultrasound also checks tumor vascularity through Doppler imaging. Tumor vascularity shows how aggressive the tumor is and how it’s responding to treatment. Changes in vascularity can tell us if treatments are working, even before we see size changes.
For example, if Doppler ultrasound shows less vascularity, it might mean the treatment is working well, even if the tumor size hasn’t changed yet.
Frequency of Monitoring Scans
How often ultrasound scans are done depends on the cancer type, stage, and treatment. Ultrasound scans are done at regular times during treatment to check how it’s going and adjust plans as needed.
For some cancers, like breast cancer, scans might be done more often at the start of treatment. For checking for recurrence, scans might be less frequent, like every 6-12 months.
Ultrasound in Cancer Follow-Up Care
Ultrasound technology is key in cancer follow-up care. It’s a non-invasive way to check how treatment is working. We use it to give patients a full care plan without invasive tests.
Surveillance for Recurrence
Ultrasound is vital for watching for cancer return. It lets doctors check the cancer area often. This helps spot any signs of cancer coming back early.
Benefits of Ultrasound Surveillance:
- Early detection of recurrence
- Non-invasive and painless
- No radiation exposure
- Cost-effective compared to other imaging modalities
Monitoring for Treatment Complications
Ultrasound helps watch for treatment side effects. It checks the liver, kidneys, and other organs. This is important because treatment can harm these organs.
| Organ | Potential Complications | Ultrasound Monitoring |
| Liver | Chemotherapy-induced damage | Assessing liver texture and detecting lesions |
| Kidneys | Radiation-induced nephropathy | Evaluating kidney size and detecting hydronephrosis |
| Gallbladder | Treatment-related dysfunction | Checking for gallstones and inflammation |
Long-Term Follow-Up Protocols
Follow-up plans change based on cancer type, stage, and treatment. Ultrasound is often part of these plans. It helps keep an eye on patients over time.
We make sure each patient gets the right care. This includes ongoing support and monitoring during their cancer journey.
Advanced Ultrasound Technologies in Oncology
Advanced ultrasound technologies are changing how we care for cancer patients. They help doctors make more accurate diagnoses and plan better treatments. They also let us watch how cancer treatments are working in real time.
Contrast-Enhanced Ultrasound
Contrast-Enhanced Ultrasound (CEUS) is a big step forward in ultrasound. It uses tiny bubbles to show blood flow and tissue details better. CEUS is great for:
- Spotting tumors and understanding their blood supply
- Helping with procedures and checking how treatments work
CEUS is safe, shows images in real time, and doesn’t use harmful radiation. It’s perfect for patients who need many scans or can’t handle other contrast agents.
Elastography for Cancer Assessment
Elastography checks how stiff tissues are. It finds that cancerous tissues are usually stiffer. It helps by:
- Telling the difference between good and bad growths
- Looking at liver fibrosis
- Helping find the right spot for biopsies
Elastography is non-invasive and gives extra info. This leads to more accurate diagnoses and better treatment plans.
3D and 4D Ultrasound Applications
Three-dimensional (3D) and four-dimensional (4D) ultrasound are making a big difference in oncology. 3D ultrasound creates detailed 3D images. 4D ultrasound adds time to these images, showing how things move.
- 3D Ultrasound helps with complex anatomy and surgery planning.
- 4D Ultrasound is good for watching fetal growth in pregnant cancer patients and seeing how tumors move.
These new ultrasound tools are changing cancer care. They offer new ways to diagnose, treat, and monitor patients. As these technologies get better, we’ll see even more exciting uses in oncology.
Oncologist Ultrasound Training and Expertise
Oncologists need a lot of training to use ultrasound well. This technology helps in diagnosing and treating cancer. It’s important to focus on the training needed for its effective use.
Specialized Training Requirements
Oncologists must get special training to use ultrasound right. This training covers how to use the equipment and read ultrasound images for cancer care.
Good training programs should include:
- Hands-on experience with ultrasound equipment
- Study of ultrasound imaging techniques specific to oncology
- Interpretation of ultrasound images in cancer diagnosis and treatment
- Understanding the limitations and possible mistakes of ultrasound in oncology
Point-of-Care Ultrasound in Oncology
Point-of-care ultrasound is used at the bedside or clinic to make quick decisions. In oncology, it’s great for checking tumor status, guiding biopsies, and watching how treatments work.
Oncologists need training that focuses on:
| Skill | Description |
| Image Acquisition | Ability to get high-quality ultrasound images for the clinical question |
| Image Interpretation | Skill in reading ultrasound images to make clinical decisions |
| Clinical Integration | Putting ultrasound findings into the bigger clinical picture |
Multidisciplinary Approach to Interpretation
Using a team approach to read ultrasound images makes diagnosis better. This means working together with oncologists, radiologists, and others to share knowledge.
We suggest regular team meetings to talk about tough cases. This way, we can use ultrasound better and help patients more.
Patient Experience During Oncologic Ultrasound
The experience of having an oncologic ultrasound involves getting ready, the test itself, and learning about the results. We know that getting tested can make people anxious. So, we aim to help you through each step, making sure you feel well-informed and at ease.
Preparing for an Oncology Ultrasound
Getting ready is important for a good oncologic ultrasound. We suggest wearing comfy clothes and no jewelry or tight clothes that might get in the way. You might need to not eat or drink for a while or have a full bladder. Our team will give you specific directions based on your situation.
- Wear comfortable, loose-fitting clothing
- Avoid jewelry that may interfere with the ultrasound
- Follow specific dietary instructions provided by our team
What to Expect During the Procedure
A skilled technician or doctor will put gel on the area and use a probe to take pictures. It’s usually painless and takes 15 to 60 minutes, depending on the test. Feel free to ask questions and let us know if you’re feeling any discomfort.
Understanding Your Results
After the test, our radiologists will look at the pictures and write a report for your oncologist. Waiting for results can be tough. Our team will share your results with you as soon as we can and talk about what’s next. If you have questions or concerns, please don’t hesitate to contact us.
Being prepared and knowing what to expect makes the oncologic ultrasound easier. We’re here to support you from start to finish, helping you understand your results.
Conclusion: The Future of Ultrasound in Cancer Care
Ultrasound is key in cancer care, from finding tumors to tracking treatments. The future looks bright, with new ultrasound tech set to improve patient care.
New ultrasound tech is making images clearer, helping doctors make better diagnoses and plans. We’ll see more use of contrast-enhanced ultrasound and elastography. These tools give deep insights into tumors.
These new tools will help doctors give more tailored care. As ultrasound tech keeps getting better, it will stay a big part of fighting cancer. This means better care and results for patients.
With the latest ultrasound tech, cancer care will get even better. It will be more precise, effective, and caring.
FAQ
Why do oncologists order ultrasounds for cancer detection?
Oncologists use ultrasounds because they are non-invasive. They help detect and monitor cancerous tumors. They also check the size of tumors and how well they respond to treatment.
What is the role of ultrasound in cancer staging?
Ultrasound is key in cancer staging. It helps oncologists see how far tumors have spread. This information helps plan treatment and predict outcomes.
How does ultrasound compare to CT scans in cancer imaging?
Ultrasound is often better than CT scans for some cancers, like breast and ovarian. It’s non-invasive, doesn’t use radiation, and shows images in real-time.
Can ultrasound be used to guide cancer biopsies?
Yes, ultrasound-guided biopsies are common in oncology. They allow for precise sampling of tumor tissue for diagnosis and analysis.
How is ultrasound used in breast cancer detection and monitoring?
Ultrasound helps with mammograms, monitors breast tumors, and guides biopsies. It gives important information for diagnosis and treatment.
What are the applications of ultrasound in gynecologic oncology?
Ultrasound is used in gynecologic oncology to check ovarian and pelvic cancers. It monitors treatment response and detects recurrence.
How does ultrasound contribute to abdominal cancer assessment?
Abdominal ultrasound evaluates liver, pancreatic, and gastrointestinal cancers. It helps oncologists see how far tumors have spread and how well they respond to treatment.
Can ultrasound be used to evaluate soft tissue cancers?
Yes, ultrasound identifies and differentiates soft tissue masses. It monitors soft tissue sarcomas and guides biopsies. It helps in diagnosing and managing soft tissue cancers.
What are the benefits of ultrasound-guided biopsies in cancer diagnosis?
Ultrasound-guided biopsies offer real-time guidance, precision, and are minimally invasive. They reduce complications and improve accuracy.
How is ultrasound used to monitor cancer treatment response?
Ultrasound measures tumor size changes and assesses tumor vascularity. It monitors treatment response, providing valuable information for treatment planning.
What is the role of contrast-enhanced ultrasound in oncology?
Contrast-enhanced ultrasound improves tumor visualization and characterization. It enhances diagnostic accuracy and treatment monitoring.
How do oncologists prepare for and interpret ultrasound results?
Oncologists are trained to perform and interpret ultrasounds. They use a multidisciplinary approach to integrate imaging findings with clinical information.
What can patients expect during an oncologic ultrasound?
Patients can expect a non-invasive, quick procedure. Minimal preparation is required. They will receive guidance on understanding their results and next steps.
References
- Chiu, S., Staley, H., Jeevananthan, P., et al. (2025). Ovarian Cancer Screening: Recommendations and Future Prospects. Rofo. https://doi.org/10.1055/a-2589-5696
- National Comprehensive Cancer Network. (2025). NCCN Clinical Practice Guidelines in Oncology: Ovarian Cancer. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1459
- British Gynaecological Cancer Society. (2017). BGCS Ovarian Cancer Guidelines. https://www.bgcs.org.uk/wp-content/uploads/2019/05/BGCS-Guidelines-Ovarian-Guidelines-2017.pdf
- National Institute for Health and Care Excellence. (2023). Ovarian cancer: recognition and initial management (NG122). https://www.nice.org.uk/guidance/cg122