Cardiology is the medical specialty focused on the heart and the cardiovascular system. It involves the diagnosis, treatment, and prevention of conditions affecting the heart and blood vessels. These conditions include coronary artery disease, heart failure, arrhythmias (irregular heartbeats), and valve disorders. The field covers a broad spectrum, from congenital heart defects present at birth to acquired conditions like heart attacks.
Send us all your questions or requests, and our expert team will assist you.
Before a doctor decides to place a stent, they must be absolutely certain about the location and severity of the blockage. You cannot fix a problem you cannot see. Therefore, the path to a stent procedure involves a series of investigative steps. It is a process of gathering evidence, starting with simple non-invasive checks and moving toward advanced imaging that lets the doctor look inside your body.
This section explains the diagnostic journey. We will walk through the tests you might undergo, from the initial stethoscope exam to the high-tech scans. The goal of these tests is to answer three questions: Is there a blockage? Where exactly is it? And is it severe enough to require a stent? Understanding these tests helps you prepare for them and understand what the results mean for your treatment plan.
If the physical exam raises suspicions, the next step is usually a stress test. A resting heart often looks normal even when it has blocked arteries because the blood flow is sufficient for sitting still. To find the problem, doctors have to make the heart work hard.
A stress test forces the heart to pump faster and harder, which increases its demand for oxygen. If an artery is blocked, it won’t be able to deliver that extra oxygen, and signs of distress will appear on the monitors. There are two main ways to do this: physical exercise or medication.
The first step is always a conversation and a basic exam. Your doctor will ask about your symptoms in detail. They want to know exactly what the pain feels like, when it happens, and what makes it better or worse. They will also review your risk factors, such as smoking history or diabetes.
During the physical exam, the doctor will use a stethoscope to listen to your heart and lungs. They are listening for irregular rhythms or fluid in the lungs. They will also check the pulses in your wrists, neck, and feet. A weak pulse in the feet, for example, is a strong clue that there are blockages in the leg arteries. They may also listen to the arteries in your neck with the stethoscope to hear if the blood is making a “whooshing” sound, which indicates turbulence caused by narrowing.
This is the standard treadmill test. You will be hooked up to a heart monitor (ECG) and asked to walk on a treadmill. The speed and incline will gradually increase.
The doctor watches your heart rate and the electrical waves on the monitor. They are looking for specific changes in the wave patterns that indicate a lack of oxygen. They also ask you if you feel any chest pain or shortness of breath. If you can’t walk on a treadmill due to joint problems, they can do a chemical stress test instead.

This is a more advanced version of the stress test. A small amount of safe radioactive tracer is injected into your bloodstream. A special camera takes pictures of your heart while you are resting and again after you have exercised (or received medication to simulate exercise).
The tracer lights up the blood flow in the heart muscle. On the images, healthy muscle looks bright because it is getting plenty of blood. Blocked areas look like dark spots or “cold spots” because the tracer can’t get there. This information tells the doctor exactly which part of the heart is at risk.

An electrocardiogram, often called an ECG or EKG, is a simple, painless test that records the heart’s electrical signals. Sticky patches with sensors are attached to your chest, arms, and legs. It takes just a few minutes.
While a stress test looks for blockages under load, a resting ECG can show if you have had a heart attack in the past (which you might not have noticed) or if your heart is currently under strain. It can also detect irregular heartbeats, called arrhythmias, which can be a complication of heart disease. It serves as a baseline for all other heart tests.
Before moving to invasive procedures, doctors might use a CT angiogram (CTA). This is a powerful X-ray scan that produces detailed 3D images of your heart and arteries. It is done in a radiology department, not an operating room.
You lie on a table that slides into a doughnut-shaped machine. Contrast dye is injected into a vein in your arm. The machine spins around you, capturing slices of images. Computers stitch these together to create a roadmap of your arteries. It is excellent for ruling out disease. If the CT scan shows clear arteries, you usually don’t need a stent. If it shows heavy calcium or narrowing, it confirms the need for a closer look.
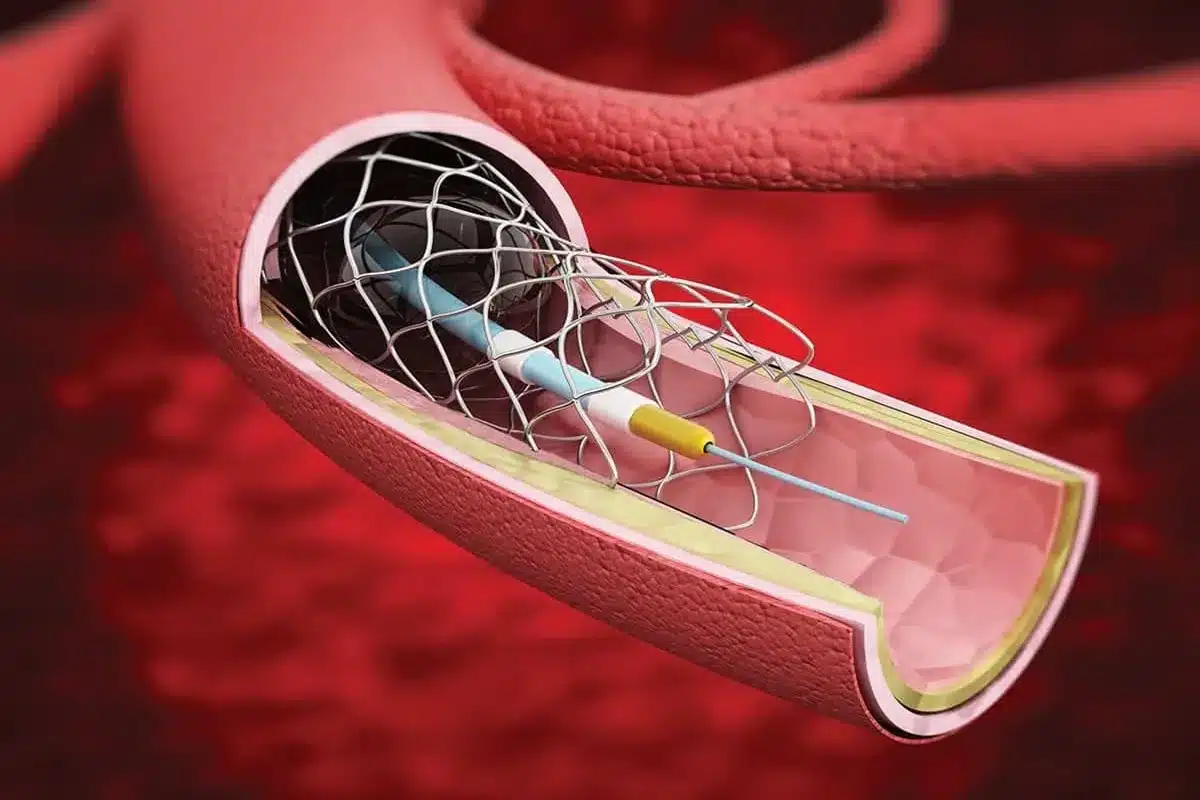
If the stress tests or CT scans suggest a serious blockage, the definitive test is the coronary angiogram. This is also known as cardiac catheterization. This kind of test is the only test that gives a perfect, real-time view of the blood flow and allows the doctor to fix the problem immediately if needed.
This test is invasive, meaning instruments enter your body, but it is not open surgery. It is performed in a special room called a catheterization lab (cath lab). This stage is the pivotal moment where the diagnosis turns into treatment.
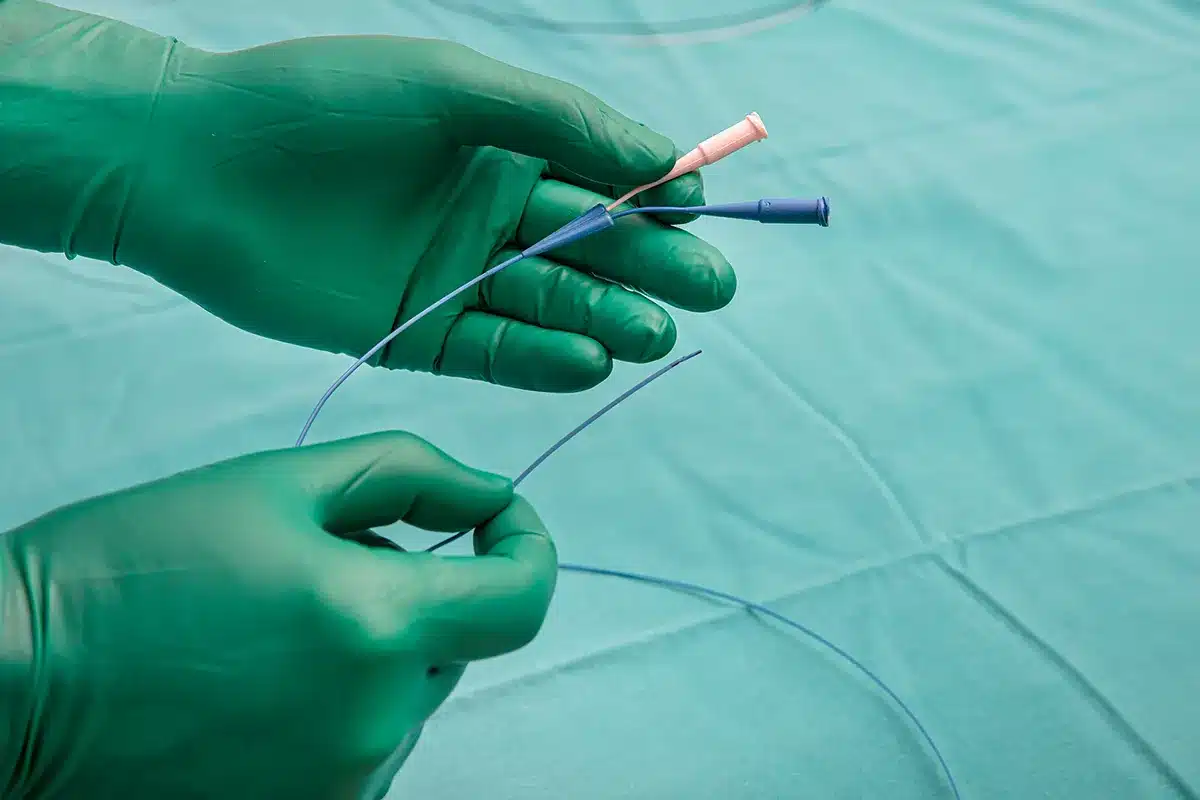
You will be awake but sedated (relaxed) for this procedure. The doctor numbs an area on your wrist or groin. They insert a thin, flexible tube called a catheter into the blood vessel.
Carefully, they guide this tube through your body’s main arteries until the tip sits right at the opening of the heart arteries. You cannot feel the tube moving inside you because blood vessels have no internal nerve endings.
Once the catheter is in place, the doctor injects a special contrast dye through it. This dye flows into your coronary arteries. At the same time, an X-ray machine creates a movie of the dye flowing.
On the screen, the arteries appear as dark, branching rivers. If there is a blockage, the river will look pinched, or the dye might stop completely. This visual proof is what the doctor uses to decide right then and there: “Yes, we need to place a stent.”
Preparing for an angiogram (and potential stent) requires a few safety steps. You will usually be told not to eat or drink anything for 6 to 8 hours before the procedure to prevent nausea from the sedation. You will need to tell your doctor about all medications you take, especially blood thinners or diabetes medicines, as doses might need to be adjusted.
You should also plan for your recovery. You will not be allowed to drive yourself home because of the sedatives. You will need a friend or family member to drive you. Packing a small bag with comfortable clothes and your ID helps make the check-in process smoother.

Send us all your questions or requests, and our expert team will assist you.
Most patients feel a sting when the local anesthetic is injected to numb the skin and some pressure when the catheter is inserted. However, the procedure itself is generally not painful. You might feel a brief warm flush when the dye is injected.
A diagnostic angiogram takes about 30 to 60 minutes. If the doctor proceeds to place a stent immediately, it can take an additional 30 to 60 minutes
The contrast dye is generally safe, but it can stress the kidneys, especially in people who already have kidney problems. Doctors will hydrate you before and after to help flush the dye out.
Using the wrist (radial access) is becoming more common because it has a lower risk of bleeding complications and allows patients to sit up and walk sooner after the procedure. However, the groin is still used if the wrist arteries are too small or twisty
No, you are usually awake. This is called “conscious sedation.” You are given medicine to make you very relaxed and sleepy, but you can still follow instructions, like “take a deep breath,” which helps the doctor get clear images.

Every year, 1 million heart stent procedures are done worldwide. This helps many people with heart disease live better lives. After getting a heart stent,

For millions of people worldwide, coronary stents are a lifeline. They keep arteries open and lower the risk of heart attack. At Liv Hospital, we
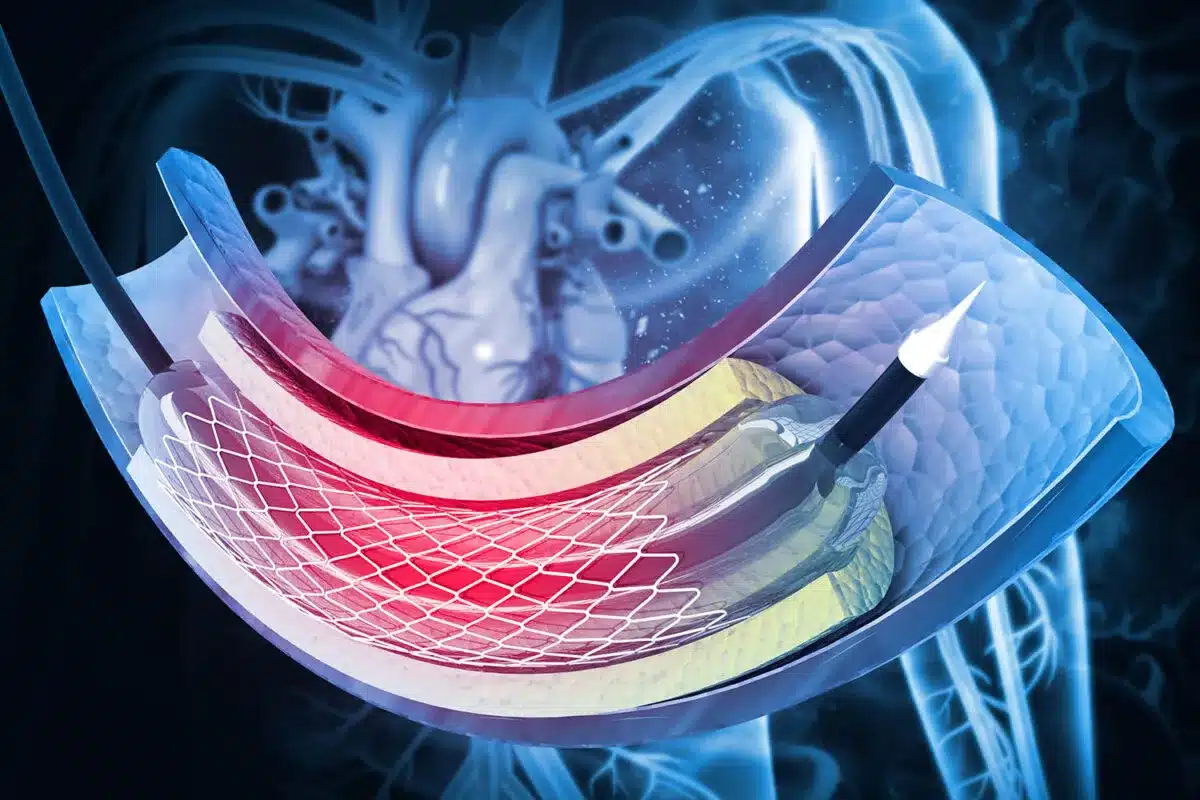
Heart stents are tiny mesh tubes that help keep arteries open. They are made from strong materials like stainless steel or cobalt chromium alloy. These

Blocked artery surgery for the heart is a lifesaving procedure. It’s often done through angioplasty and stent placement. This helps restore blood flow to the

Coronary artery disease affects millions worldwide. The use of coronary stents is a common treatment. But is it considered a major surgery? We look into

Coronary artery disease affects millions worldwide. Many patients get stent placement procedures every year. The number of coronary stents needed depends on the patient’s condition

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)