Last Updated on November 26, 2025 by Bilal Hasdemir
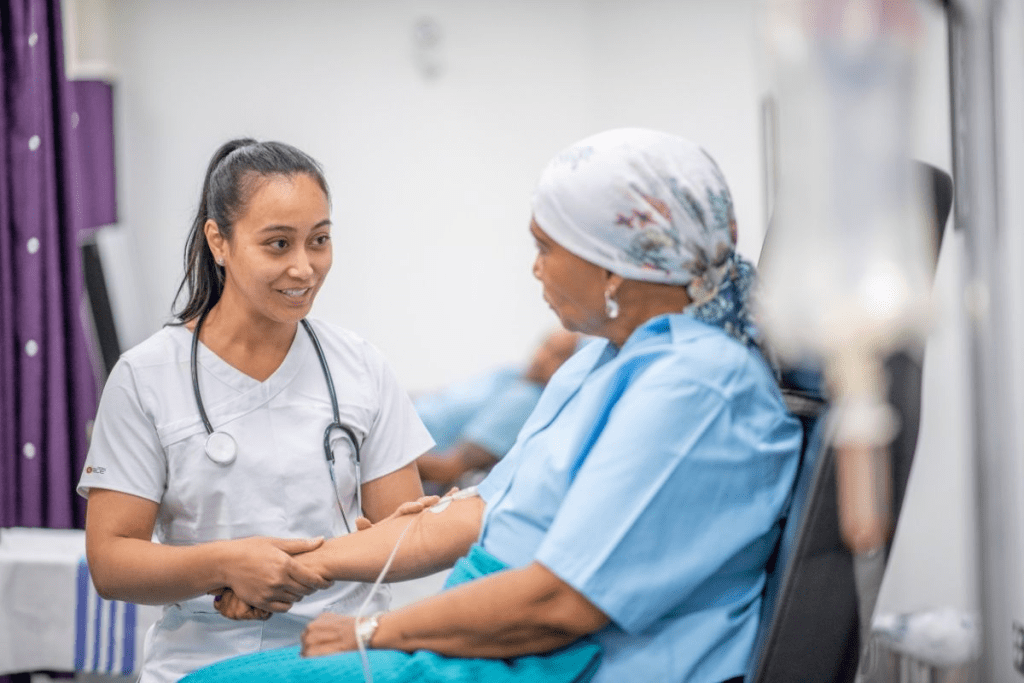
Chemotherapy is a key part of cancer treatment. It uses drugs to kill cancer cells. But, chemotherapy can also cause pain as a side effect. It’s important for patients to understand this to manage their treatment better.
Pain from chemotherapy can be different for everyone. The type of cancer, the chemotherapy plan, and how well someone can handle pain all matter. These factors help decide how much pain someone might feel.
Key Takeaways
- Chemotherapy can cause a range of side effects, including pain.
- The experience of pain varies among individuals undergoing chemotherapy.
- Understanding chemotherapy pain is crucial for effective treatment navigation.
- Factors such as cancer type and chemotherapy regimen influence pain levels.
- Individual tolerance to pain also plays a significant role.
Understanding Chemotherapy and Pain
Chemotherapy and pain have a complex relationship. It’s shaped by how the treatment works and the patient’s health. Chemotherapy is a key part of cancer treatment. It uses strong drugs to kill cancer cells.
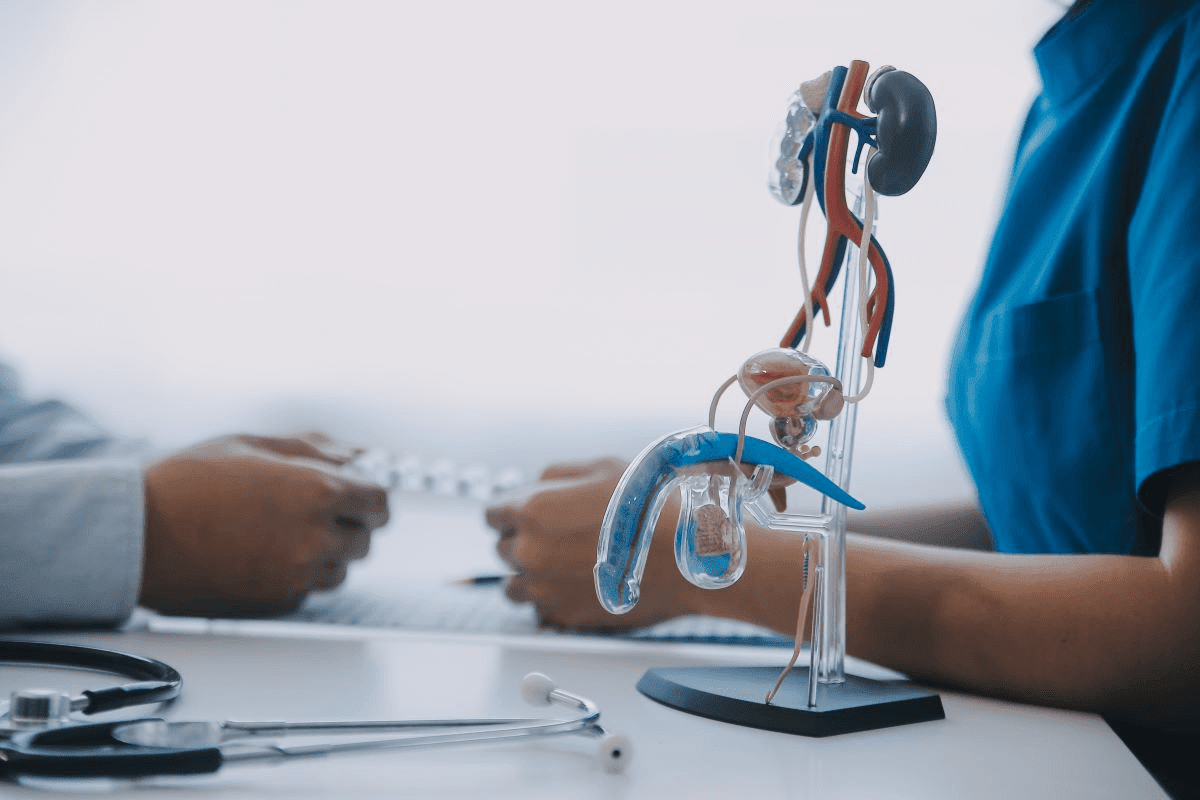
What is Chemotherapy?
Chemotherapy uses drugs that target fast-growing cells, like cancer cells. But these drugs can also harm healthy cells that grow quickly. This can cause side effects, including chemotherapy pain.
How Chemotherapy Affects the Body
Chemotherapy can affect the body in many ways. It can damage healthy cells, leading to side effects. Pain from chemotherapy side effects is common. It can feel like pain from chemotherapy injections, nerve pain, or body aches.
Variability in Patient Experiences
How patients feel about chemotherapy and pain can differ a lot. It depends on the drugs used, how often they’re given, and the patient’s health. Knowing these factors helps manage chemotherapy body pain better.
By understanding pain and its causes, patients and doctors can reduce discomfort. This makes the treatment process better for everyone.
Does Chemo Hurt? The Truth About Chemotherapy Pain

It’s important for patients to know the truth about chemotherapy pain before starting treatment. Chemotherapy saves many lives, but worries about pain can cause a lot of stress.
Immediate Pain During Administration
Many worry if chemotherapy hurts when it’s given. The good news is that chemotherapy itself doesn’t hurt. But, how it’s given can sometimes be uncomfortable.
For example, getting chemotherapy through an IV might feel like a pinch or sting when the needle goes in.
Even though the drugs themselves don’t hurt, some people might feel a cold sensation or pressure during the infusion. This feeling usually goes away once the treatment is over.
Delayed Pain Reactions
While chemotherapy might not hurt when given, some people feel pain later. This can happen for many reasons, like how the body reacts to the drugs or side effects like neuropathy.
How and when pain happens can be different for everyone, so it’s key to talk about it with your doctor. Knowing about possible pain after treatment can help you prepare.
Misconceptions About Chemotherapy Pain
There are many wrong ideas about chemotherapy pain that can make people more anxious. One big myth is that chemotherapy is very painful. While some people do feel pain or discomfort, it’s not true for everyone.
“Chemotherapy is not inherently painful, but the treatment and its side effects can sometimes cause discomfort or pain.” “ An oncologist
Learning the real facts about chemotherapy pain can help patients deal with their treatment better. It’s also good to know that there are ways to manage any pain or discomfort from chemotherapy.
Types of Pain Associated with Chemotherapy
Chemotherapy can cause pain in different ways. This includes pain at the injection site, in nerves, muscles, joints, and bones. Each type shows how chemotherapy can affect the body in complex ways.
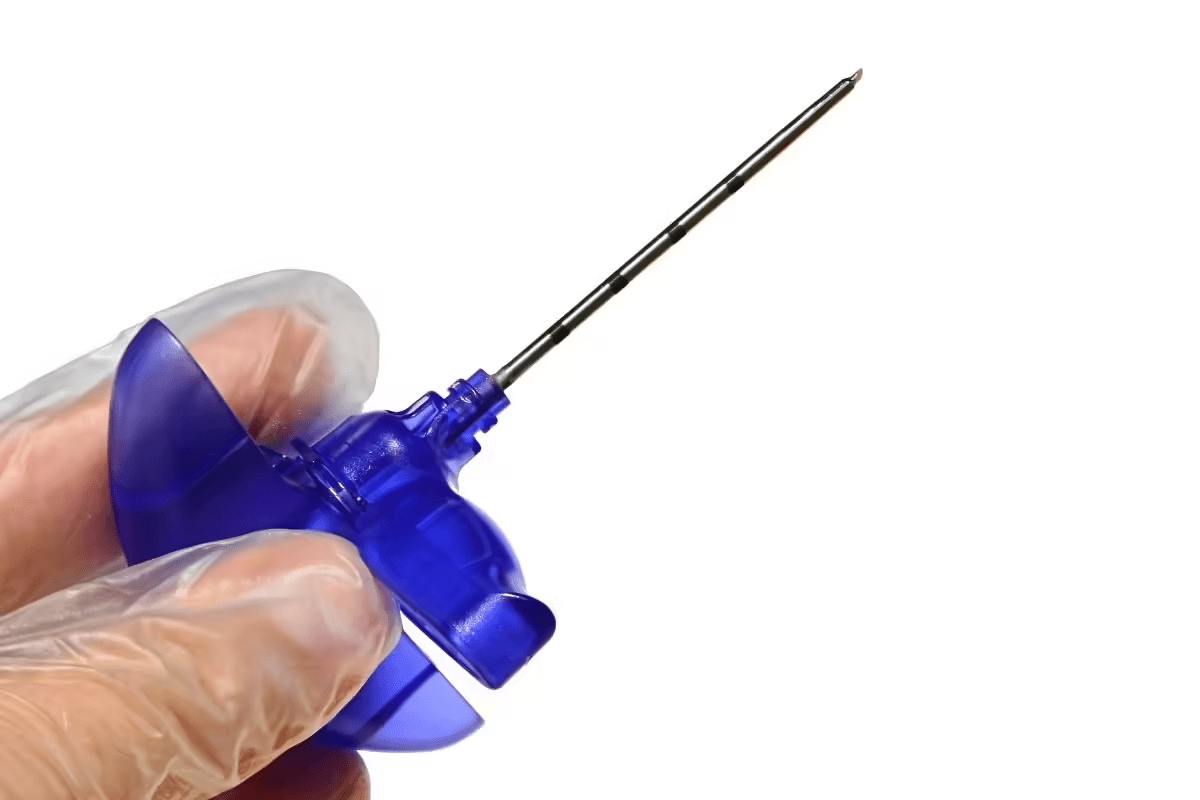
Injection Site Pain
Pain at the injection site is common during chemotherapy. This pain can be mild or severe. It depends on the drugs used and how sensitive a person is.
Some people feel pain or discomfort from the IV insertion. Others react to the chemotherapy drugs. To manage this pain, doctors might change the IV site or use topical anesthetics. Applying warm or cold compresses can also help.
Nerve Pain (Neuropathy)
Nerve pain, or neuropathy, is another common issue. It happens when chemotherapy drugs damage nerves. Symptoms include numbness, tingling, and burning sensations, usually in the hands and feet.
The severity of neuropathy varies. Some people have mild symptoms, while others face severe pain. Knowing the risk of neuropathy with certain treatments can help manage it.
Muscle and Joint Pain
Many patients experience muscle and joint pain during chemotherapy. This pain can come from the drugs or the body’s reaction to treatment.
Muscle and joint pain can be mild or severe. It can affect different parts of the body. Managing this pain often involves medication, physical therapy, and lifestyle changes.
Bone Pain from Certain Medications
Some chemotherapy drugs can cause bone pain. This pain can be due to the drugs’ effects on bone marrow or the bone itself. It can be widespread or focused in certain areas.
Managing bone pain may involve changing the chemotherapy regimen. Doctors might also use pain medications or other treatments to reduce discomfort and improve quality of life.
Different Chemotherapy Administration Methods and Pain Levels
Chemotherapy is given in various ways, and knowing these differences is key to managing pain. The way the treatment is given can greatly affect how much discomfort or pain you feel during and after it.
Intravenous (IV) Chemotherapy
IV chemotherapy is a common method, where the drug goes straight into a vein. It’s usually well-tolerated, but some might feel pain or discomfort at the injection site.
- Common issues include vein irritation and potential for extravasation.
- Some patients may experience a cold sensation or metallic taste during infusion.
Oral Chemotherapy
Oral chemotherapy means taking medication in pill or liquid form. It’s often easier to do but can still cause side effects.
“Oral chemotherapy can be just as effective as IV chemotherapy for certain types of cancer, but it requires strict adherence to the prescribed regimen.” -Cancer Treatment Expert
- Gastrointestinal side effects are common.
- Some patients may experience mouth sores or other oral complications.
Intrathecal and Intraperitoneal Chemotherapy
These are more specialized ways of giving chemotherapy. Intrathecal chemotherapy injects drugs into the spinal fluid. Intraperitoneal chemotherapy puts drugs directly into the abdominal cavity.
Intrathecal chemotherapy is often used for cancers that have spread to the central nervous system.
Intraperitoneal chemotherapy is typically used for ovarian cancer and some other abdominal cancers.
Port vs. Direct IV Access
Using a port versus direct IV access can also affect your experience. A port is a small device implanted under the skin, making it easier to access a vein.
- Ports reduce the need for repeated needle sticks.
- They can make the administration of chemotherapy more comfortable and less painful.
Understanding the different ways chemotherapy is given and their potential for pain or discomfort is important. By talking to their healthcare provider, patients can make informed decisions about their care.
Common Painful Side Effects of Chemotherapy
People getting chemotherapy often face many painful side effects. These can change a lot from person to person. They depend on the type of chemotherapy, how much is used, and the patient’s health.
Mouth Sores and Oral Pain
Mouth sores, or mucositis, are a common and painful side effect of chemotherapy. These sores can pop up in the mouth, throat, or digestive tract. They make eating, drinking, and even swallowing saliva painful. Managing oral pain is key to keep up nutrition and avoid infections. We suggest using mouthwashes with saline or medicated solutions as your doctor prescribes.
Headaches and Migraines
Some chemotherapy drugs can cause headaches or migraines. This is because they affect blood vessels and nerve endings. These headaches can be mild or very severe. Staying hydrated and getting enough rest can help ease these symptoms.
Abdominal Pain and Digestive Issues
Chemotherapy can lead to stomach pain, nausea, vomiting, and changes in bowel habits. These can include diarrhea or constipation. These digestive problems can be painful and make it hard to eat well. We suggest eating foods that are easy on the stomach. Also, tell your healthcare team if your symptoms get worse.
Skin Sensitivity and Rashes
Some chemotherapy agents can make your skin sensitive, cause rashes, or dryness. This can be painful and uncomfortable. To help, protect your skin from extreme temperatures, use gentle skin care products, and avoid direct sunlight. Sometimes, special treatments are needed to make your skin feel better.
Managing these painful side effects is key to chemotherapy care. Knowing what to expect and how to manage these side effects can make treatment more comfortable. We work with patients to create a care plan that covers both the cancer and chemotherapy side effects.
Factors That Influence Pain During Chemotherapy
Many factors can affect how much pain someone feels during chemotherapy. Knowing these factors helps doctors find better ways to manage pain.
Type of Cancer Being Treated
The type of cancer matters a lot when it comes to pain during chemotherapy. Each cancer reacts differently to treatment, which changes how much pain someone feels.
Cancers that grow fast or spread a lot might need stronger chemotherapy. This can lead to more pain.
Chemotherapy Drugs and Protocols
The chemotherapy drugs and how they are used also play a big role. Some drugs cause more pain than others. This can be because they are stronger or have more side effects.
For example, some drugs can damage nerves, causing pain. Others might make muscles or joints hurt.
| Chemotherapy Drug | Common Side Effects | Potential for Pain |
| Paclitaxel | Nerve damage, muscle pain | High |
| Cisplatin | Nausea, nerve damage | Moderate to High |
| Doxorubicin | Fatigue, hair loss | Low to Moderate |
Individual Health Factors
Health factors like overall health, age, and past medical conditions also matter. These can change how much pain someone feels during chemotherapy.
People with health problems like diabetes or heart disease might feel more pain. This is because these conditions can make side effects worse.
Previous Pain Conditions
Having pain before chemotherapy can also affect how someone feels pain during treatment. People with chronic pain might need special pain plans.
By understanding these factors, doctors can make pain plans that work better for each patient. This makes chemotherapy easier for everyone.
Preparing for Chemotherapy to Minimize Pain
Getting ready for chemotherapy is more than just physical prep. It also means getting your mind and heart ready. Knowing what to do before treatment can help lower pain and discomfort risks.
Pre-Treatment Consultations
Before starting chemotherapy, it’s key to talk with your healthcare team. These talks help you understand your treatment plan, possible side effects, and pain management strategies. Make sure to ask about the chemotherapy drugs, their side effects, and pain management.
Preventative Medications
Some patients may get medicines to prevent side effects like nausea or pain. It’s important to take these medicines as directed to avoid discomfort.
| Medication Type | Purpose | Administration Timing |
| Anti-nausea medication | Prevent nausea | Before chemotherapy |
| Pain relief medication | Manage pain | As directed by healthcare provider |
Physical Preparation
Getting your body ready for chemotherapy can help you handle it better. Eating well, staying hydrated, and doing light exercise can boost your health and lower side effect risks.
“Preparing your body for chemotherapy can make a significant difference in how you feel during and after treatment. A healthy lifestyle, including a balanced diet and regular exercise, can enhance your resilience.” ” Oncology Specialist
Mental and Emotional Readiness
It’s just as important to prepare mentally and emotionally as it is physically. Mindfulness, meditation, and counseling can help with chemotherapy’s emotional side. Having a support network of family, friends, and groups can offer comfort and help.
- Mindfulness and meditation
- Counseling services
- Support groups
- Family and friend networks
By preparing fully, patients can reduce pain and make chemotherapy better. It’s about setting up a supportive space for your physical, emotional, and mental health.
The Experience of Chemotherapy Infusions
Patients going through chemotherapy infusions face many feelings and sensations. Knowing what happens during these sessions can ease some of the worry about treatment.
What Happens During a Chemo Session
In a chemotherapy infusion, drugs to fight cancer are given through an IV. The time it takes can vary, from a few minutes to hours, based on the treatment plan.
Preparation is key. Before starting, doctors get everything ready. They make sure the patient is comfortable and safe.
Common Sensations During Infusion
During the infusion, patients might feel different things. Some might feel a bit uncomfortable or taste something metallic. This is because of the drugs in their system.
Post-Infusion Discomfort
After the infusion, some people might feel tired, nauseous, or have pain where the IV was. It’s important to manage these feelings to make the treatment better.
- Resting well after treatment
- Drinking lots of water to get rid of the drugs
- Taking pain meds as told by doctors
Managing Anxiety During Treatment
Managing anxiety is key when getting chemotherapy. Deep breathing, meditation, and thinking positive can help. These methods can make patients feel better.
Having support from loved ones and doctors is also crucial. It helps patients deal with the emotional side of chemotherapy.
Chemotherapy-Induced Peripheral Neuropathy (CIPN)
CIPN is a nerve damage condition caused by chemotherapy. It affects a patient’s quality of life by causing various symptoms.
Symptoms and Progression
CIPN symptoms include numbness, tingling, and pain in hands and feet. These feelings can be mild or severe and may get worse if not treated.
- Numbness or tingling in extremities
- Pain or burning sensations
- Sensitivity to cold or heat
- Loss of coordination or balance
In severe cases, CIPN can make walking or doing fine motor tasks hard.
Long-Term Management
Managing CIPN needs a detailed plan. Some symptoms may go away after treatment, but others can last, needing ongoing care.
- Medications to alleviate pain and other symptoms
- Physical therapy to improve mobility and strength
- Lifestyle adjustments, such as avoiding extreme temperatures
We help patients create a care plan that meets their needs and improves their life quality.
When to Seek Medical Attention
Patients should tell their doctor about any CIPN symptoms right away. Early treatment can lessen symptoms and improve results.
“Early detection and management of CIPN can significantly impact a patient’s ability to continue with their chemotherapy treatment as planned.” -A cancer research study
Latest Research on CIPN
Research on CIPN is ongoing to understand its causes and find better treatments. Studies are looking at how different chemotherapy agents cause CIPN.
We keep up with new research to offer our patients the best care for CIPN.
Medical Approaches to Managing Chemotherapy Pain
Effective pain control is key in chemotherapy care. It improves patient outcomes. Managing chemotherapy pain requires a detailed approach with various medical strategies.
Prescription Pain Medications
Prescription pain medications are vital for managing chemotherapy pain. They range from mild to strong opioids, based on pain severity. Accurate diagnosis and pain assessment are crucial for the right medication and dosage.
Healthcare providers consider the patient’s condition and medical history. They also look at potential interactions with other treatments. For example, acetaminophen or NSAIDs might be used for mild pain. Opioids are for more severe pain.
Preventative Treatments
Preventative treatments help avoid pain during chemotherapy. These include medications that protect against nerve damage, a common pain cause in chemotherapy patients.
Anticonvulsants or antidepressants can prevent chemotherapy-induced peripheral neuropathy (CIPN). This condition causes significant pain. By adding these treatments to the chemotherapy regimen, healthcare providers can lessen pain risk and severity.
When to Adjust Your Chemo Protocol
Adjusting the chemotherapy protocol might be needed for effective pain management. This could mean changing the dosage, switching drugs, or altering the schedule.
It’s crucial for the patient and healthcare team to work together. Monitoring the patient’s response to chemotherapy and reporting pain helps make informed care decisions.
Balancing Pain Control and Side Effects
Managing chemotherapy pain involves balancing pain control with medication side effects. Healthcare providers aim to minimize side effects while managing pain well.
This balance requires careful consideration of the patient’s health and chemotherapy type. Tailoring pain management strategies to the individual helps achieve optimal pain relief with fewer side effects.
Non-Pharmacological Pain Management Strategies
Managing pain during chemotherapy needs a mix of methods. Non-pharmacological strategies help a lot. They can make patients feel better and live better lives.
Physical Therapy and Exercise
Physical therapy and exercise are key for pain management. Gentle activities like yoga or swimming keep muscles flexible and reduce pain. Physical therapists create special plans for each patient’s needs.
For example, yoga can help with balance for those with neuropathy. Exercise also boosts well-being and fights off fatigue, a common side effect of chemotherapy.
Heat and Cold Therapy
Heat or cold can help manage pain. Heat, like a warm bath, relaxes muscles and boosts blood flow. Cold, like an ice pack, reduces swelling and numbs pain.
But, be careful with heat or cold, especially if you have neuropathy or sensitive skin. Always test the temperature and watch your skin to avoid problems.
Massage and Acupuncture
Massage therapy relaxes muscles and reduces tension. Gentle massage or lymphatic drainage is especially helpful. Acupuncture, with fine needles in specific spots, also relieves pain for some.
Make sure to see licensed professionals for massage and acupuncture. They can customize treatments for your pain and comfort.
Mindfulness and Meditation
Mindfulness and meditation help manage pain by calming the mind and reducing stress. You can try deep breathing, guided imagery, or meditation alone or with a therapist.
These practices do more than just help with pain. They also boost mental and emotional health. Regular mindfulness can lead to better coping and a better life.
Patient Stories: Real Experiences with Chemotherapy Pain
Patient stories give us a deep look into chemotherapy pain. They share how pain can show up differently and how to handle it.
Diverse Perspectives on Pain Management
Chemotherapy pain varies from person to person. It depends on the cancer type and treatment. Some feel nerve damage, while others get pain at the injection site.
A breast cancer patient talked about nerve damage pain. She felt numbness and tingling in her hands and feet. This is called chemotherapy-induced peripheral neuropathy (CIPN).
On the other hand, a lung cancer patient felt pain during the infusion. He got a burning feeling at the IV site. He used medication and cold compresses to manage it.
Coping Strategies That Worked
Many patients found ways to cope with pain. Some use medicine and alternative therapies. For example, one patient used mindfulness and meditation to reduce anxiety and pain.
Another patient found physical therapy helpful for muscle and joint pain. He stressed the need to stay mobile and strong during treatment.
- Mindfulness and meditation
- Physical therapy and exercise
- Medication management
- Alternative therapies like acupuncture and massage
Unexpected Challenges and Solutions
Patients face surprises during chemotherapy. One patient got severe mouth sores, making eating hard. She used a special mouthwash and ate softer foods to help.
Another patient worried about pain during future treatments. He worked with a therapist and had family support to cope.
These stories show the need for a complete approach to pain management. This includes medical help, lifestyle changes, and emotional support.
Long-Term Pain Issues After Completing Chemotherapy
Chemotherapy doesn’t end the journey. For some, long-term pain can start after treatment. It’s key to understand and manage these issues to keep quality of life high.
Persistent Neuropathy
Chemotherapy-Induced Peripheral Neuropathy (CIPN) is a common side effect. It causes numbness, tingling, or pain in hands and feet. Managing CIPN requires a mix of treatments, like medicines, physical therapy, and lifestyle changes.
Some find relief in alternative therapies like acupuncture or massage. It’s vital to work with healthcare providers to find the best treatment.
Joint and Muscle Problems
After chemotherapy, some face joint and muscle pain. This can be due to treatment or changes in activity levels. Physical therapy is often suggested to improve mobility and lessen pain.
| Issue | Symptoms | Management Strategies |
| Neuropathy | Numbness, tingling, pain in hands and feet | Medications, physical therapy, acupuncture |
| Joint Pain | Ache or stiffness in joints | Physical therapy, exercise, pain relief medications |
| Muscle Pain | Muscle ache or cramps | Stretching, massage, heat or cold therapy |
Rehabilitation Options
Rehabilitation is key in managing long-term pain after chemotherapy. It includes physical therapy, occupational therapy, and sometimes psychological support.
A rehabilitation program is customized to meet individual needs. It aims to improve function and reduce pain. It’s a step towards regaining control after cancer treatment.
When Pain Becomes Chronic
For some, pain can become chronic, needing ongoing management. Creating a chronic pain management plan involves working with a healthcare team. They aim to find a balance between pain relief and avoiding side effects.
It’s important to keep track of pain levels and adjust the plan as needed. This might include a mix of medications, lifestyle changes, and alternative therapies.
Conclusion: Navigating the Challenge of Chemotherapy Pain
Dealing with chemotherapy pain needs a full plan. This includes knowing about the treatment and getting ready for side effects. It also means using both medical and non-medical ways to manage pain.
Chemotherapy pain is different for everyone. So, it’s key to make pain plans that fit each person’s needs. This way, we can help manage pain better.
Good pain management mixes medical and non-medical methods. This includes medicines and treatments, plus physical therapy and mindfulness. Knowing about chemotherapy pain and what affects it helps patients find relief.
We believe in a complete approach to chemotherapy pain. This ensures patients get care that meets their specific needs. By doing this, we can make chemotherapy better and help with pain relief.
FAQ
Is chemotherapy painful?
Chemotherapy itself is not usually painful. But, some ways it’s given and side effects can cause discomfort or pain.
What are the common types of pain associated with chemotherapy?
Common pains include injection site pain, nerve pain (neuropathy), and muscle and joint pain. Bone pain can also occur from certain chemotherapy drugs.
How does the method of chemotherapy administration affect pain levels?
The way chemotherapy is given can affect pain levels. Methods like IV, oral, intrathecal, and intraperitoneal can change how much discomfort or pain patients feel.
What are some painful side effects of chemotherapy?
Painful side effects include mouth sores, headaches, and abdominal pain. Skin issues can also be painful.
Can individual health factors influence the pain experienced during chemotherapy?
Yes, health factors like previous pain and overall health can change the pain experienced during chemotherapy.
How can patients prepare for chemotherapy to minimize pain?
To prepare, patients should have pre-treatment consultations and use preventative medications. Physical conditioning and mental readiness also help minimize pain and make treatment smoother.
What happens during a chemotherapy infusion session?
During a session, patients may feel a range of sensations. Some may feel discomfort afterward. Knowing what to expect can help reduce anxiety.
What is Chemotherapy-Induced Peripheral Neuropathy (CIPN)?
CIPN is a side effect of some chemotherapy agents. It causes nerve damage, leading to pain, numbness, and tingling.
How can chemotherapy pain be managed?
Pain can be managed with medical treatments like pain medications and preventative treatments. Non-pharmacological strategies include physical therapy, heat and cold therapy, massage, acupuncture, mindfulness, and meditation.
Can pain persist after chemotherapy has ended?
Yes, some patients experience pain that lasts after chemotherapy ends. Understanding the causes and available management strategies is key to maintaining quality of life.
What are some long-term pain issues that can occur after chemotherapy?
Long-term pain issues include persistent neuropathy, joint and muscle problems, and chronic pain, among others.
Are there any rehabilitation options available for managing long-term pain after chemotherapy?
Yes, rehabilitation options like physical therapy can help manage long-term pain after chemotherapy.
References
Colvin, L. A., & Fallon, M. (2019). Chemotherapy-induced peripheral neuropathy: A multistep approach to prevention and management. Pain, 161(Supplement 1), S9“S14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6499732/