
Millions of people worldwide live with pacemakers and defibrillators. These devices help manage heart rhythms and are lifesaving. But, they can make everyday tasks tricky, like going through metal detectors or security screenings.
Things you can’t do with a pacemaker or ICD. Avoid metal detectors. Get best safety info. Hand searches are vital to prevent dangerous errors.
Living with these devices means being careful and aware. People with cardiac devices often face challenges at security checkpoints. Knowing how to handle these situations is key to staying safe.
Managing daily life with a pacemaker or defibrillator requires understanding its limits. We’ll look at the important things to know and do. This way, you can keep your device safe and working well.
Key Takeaways
- Understand the implications of having a pacemaker or defibrillator on daily activities.
- Learn how to navigate security screenings safely with cardiac devices.
- Discover the precautions to take when going through metal detectors with a pacemaker or defibrillator.
- Know the guidelines for living with cardiac devices to ensure their effectiveness.
- Be aware of the possible risks with cardiac devices and security screenings.
Understanding Cardiac Devices: Pacemakers and Defibrillators
Cardiac devices like pacemakers and implantable cardioverter defibrillators (ICDs) are key in managing heart rhythm issues. They help control the heartbeat, keeping it within a normal range. Knowing how these devices work and their differences is vital for patients and their caregivers.
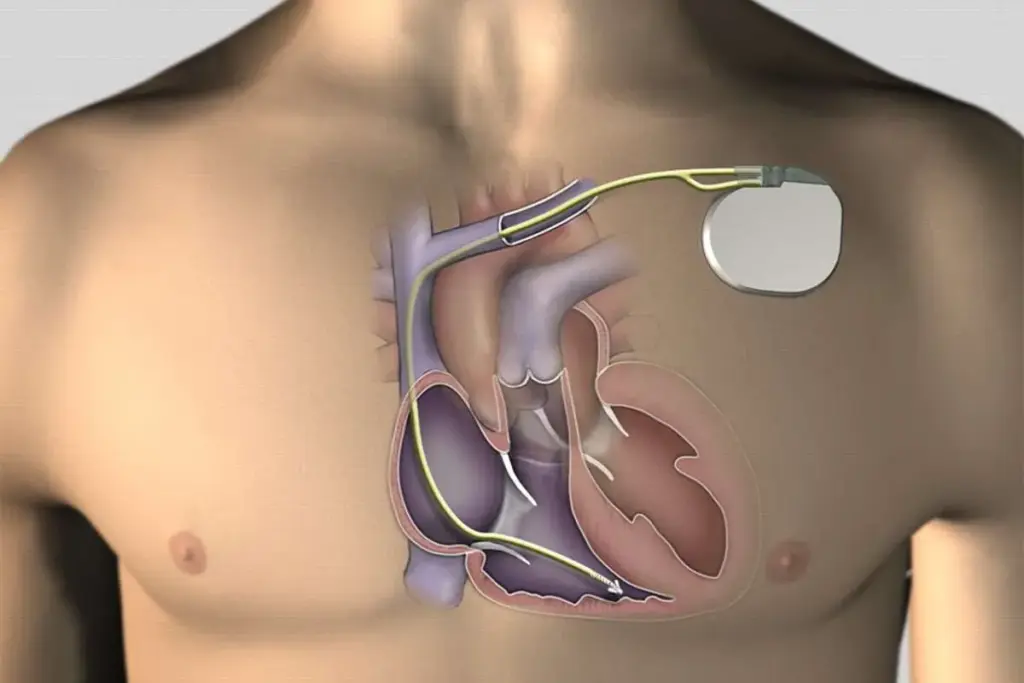
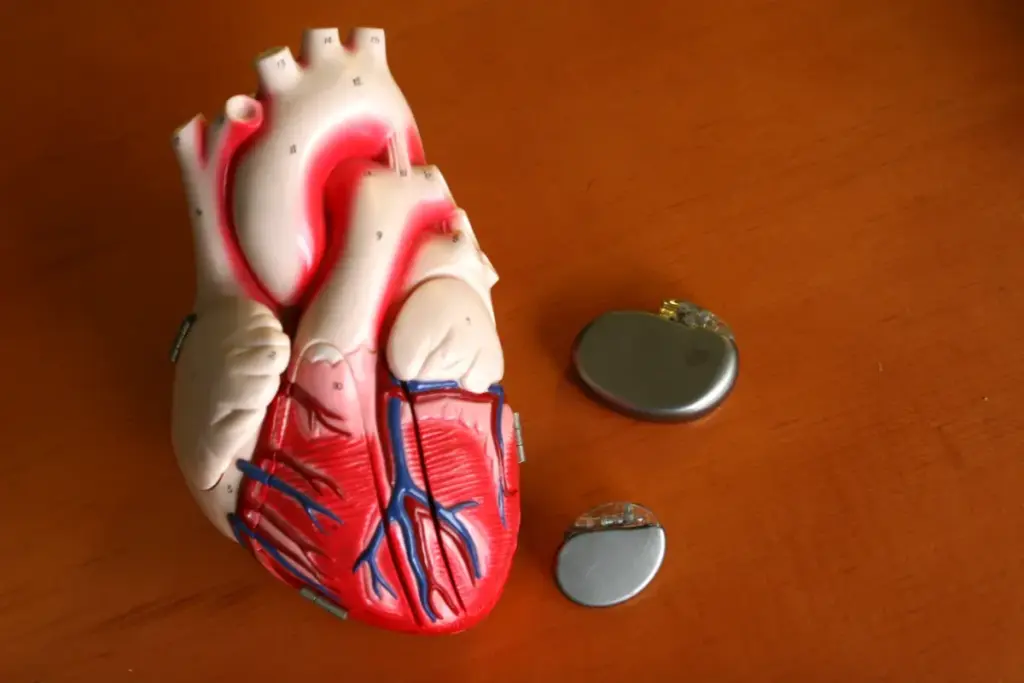
What is a Pacemaker?
A pacemaker is a small device implanted under the skin, usually near the collarbone. It sends electrical impulses to regulate the heartbeat, ensuring it beats at a normal rate. Pacemakers treat conditions like bradycardia, where the heart beats too slowly. They can adjust the heart rate to meet the patient’s needs, mimicking a natural heartbeat.
What is an Implantable Cardioverter Defibrillator (ICD)?
An ICD is also implanted and prevents sudden death from cardiac arrhythmias. It watches the heart’s rhythm and shocks it when it finds a dangerous arrhythmia. ICDs are for patients at high risk of ventricular fibrillation or tachycardia. Like pacemakers, they can be set to meet the patient’s specific needs, protecting against dangerous heart rhythms.
Key Differences Between These Devices
Pacemakers and ICDs both manage heart rhythm disorders but differ in their main functions. Pacemakers ensure the heart beats at a consistent, adequate rate. ICDs correct life-threatening arrhythmias. Some devices do both, providing full heart rhythm management. It’s important for patients to understand their device’s specific role.
Metal Detectors and Security Screening with Cardiac Devices
Going through airport security with a pacemaker or ICD needs careful thought. We’ll look at the safety of metal detectors and security screenings for these devices. It’s key to know the different methods and how to go through them safely.
Can You Go Through Airport Security with a Pacemaker?
It’s usually safe to go through airport security with a pacemaker or ICD. But, you must tell security about your device before screening. This lets them pick the best method for you.
The TSA says people with pacemakers or ICDs usually won’t have problems with metal detectors or scanners. But, some devices might be affected by the fields from the screening.
“Patients with implanted pacemakers or cardioverter-defibrillators should be screened using a pat-down or other alternative methods to avoid possible interference with their devices.” –
American Heart Association
Handheld Wands vs. Walk-Through Metal Detectors
Handheld wands and walk-through metal detectors are common security tools. They’re usually safe, but there are things to think about for people with cardiac devices.
- Handheld wands: Don’t put them right over the pacemaker or ICD site to avoid interference.
- Walk-through metal detectors: They might cause rare interference with cardiac devices. But, most modern devices can handle these fields.
|
Screening Method |
Safety Considerations for Cardiac Devices |
|---|---|
|
Handheld Wands |
Avoid direct placement over the device site |
|
Walk-Through Metal Detectors |
Generally safe, but may cause rare interference |
Full-Body Scanners and Alternative Screening Methods
Full-body scanners are also used for security. For people with pacemakers or ICDs, it’s best to use alternative methods.
Tell TSA officers about your device and ask for a pat-down or another screening. This keeps you safe and helps security know what to do.
What to Do When Traveling
Traveling with a pacemaker or ICD requires preparation. Here are some tips for airport security:
- Carry your device identification card with you.
- Inform security personnel about your device before screening.
- Request alternative screening methods if necessary.
- Be ready to explain your device and its impact on security screening.
Being informed and prepared helps people with cardiac devices go through airport security safely and smoothly.
Electromagnetic Interference: What You Need to Know
For those with implanted cardiac devices, knowing about electromagnetic interference is key. It helps keep your device working right and keeps you healthy. Electromagnetic interference (EMI) is when outside electromagnetic fields mess with electronic devices. This includes pacemakers and implantable cardioverter-defibrillators (ICDs).
How EMI Affects Pacemakers and Defibrillators
EMI can mess with pacemakers and ICDs. It can cause small problems or big issues. For example, strong fields can make a pacemaker think it’s getting the wrong signals. This can lead to it not working right or not working at all.
Common Sources of Electromagnetic Interference
Many everyday things can cause EMI. These include:
- Industrial equipment: Stuff used in making things and building can make a lot of EMI.
- Household appliances: Some home appliances, like big motors or microwaves, can also cause EMI.
- Wireless devices: Things like cell phones and tablets can sometimes mess with cardiac devices. But most modern devices are made to avoid this problem.
Safety Measures to Prevent EMI Issues
To avoid EMI problems, people with pacemakers or ICDs can do a few things:
- Stay away from things that make strong electromagnetic fields.
- Don’t lean against or stay near big machines or some home appliances for too long.
- Use wireless devices as the maker says, usually keeping them 6 inches away from your device.
Knowing where EMI can come from and taking steps to avoid it can help a lot. It can lower the chance of interference problems.
Things You Can’t Do With a Pacemaker
Knowing what you can’t do with a pacemaker is key to staying healthy. A pacemaker can greatly improve life for those with heart issues. But, it’s important to know which activities might be risky.
High-Risk Activities to Avoid Completely
Some activities are too risky for pacemaker users and should be avoided. These include:
- Contact sports like football or hockey, as they can harm the pacemaker or its leads.
- Working with strong magnetic fields, like certain industrial equipment or MRI machines, unless precautions are taken.
- High-voltage electrical work, as it can mess with the pacemaker’s function.
Talking to your doctor is vital to know what’s safe for you.
Moderate-Risk Activities Requiring Caution
Some activities are not completely off-limits but need caution. These include:
- Exercise is good, but heavy weightlifting might need to be avoided or modified.
- Travel, including flying, is usually safe, but tell the airline and security about your pacemaker.
- Household chores or hobbies with strong magnetic fields or strain should be done carefully.
Always check with your doctor before starting or continuing any activity you’re unsure about.
Misconceptions About Pacemaker Restrictions
There are many wrong ideas about pacemaker restrictions. For example:
- Many think pacemakers mean no physical activity, but most people can do normal activities with some changes.
- Some believe pacemakers are safe from all external influences, but strong magnetic fields or high-voltage equipment can affect them.
Knowing the truth and talking to healthcare experts can clear up what’s safe and what precautions are needed.
Medical Procedures and Imaging Restrictions
Medical imaging and procedures are key for diagnosing and treating health issues. But, for those with pacemakers or ICDs, there are special considerations. We will look at the restrictions and guidelines for these cardiac devices.
MRI Compatibility Concerns
Magnetic Resonance Imaging (MRI) is a powerful tool for diagnosis. But, its strong magnetic field can affect pacemakers and ICDs. MRI compatibility is a big concern for patients with these devices. It’s important to make sure the device is MRI-compatible and follow certain precautions during the procedure.
Some key considerations include:
- Checking if the pacemaker or ICD is MRI-compatible
- Following specific guidelines for MRI scanning, such as using a lower magnetic field strength
- Monitoring the patient during the MRI procedure
A study in the Journal of the American College of Cardiology found that MRI can be safe for patients with MRI-compatible pacemakers and ICDs. This is when the right precautions are taken.
“MRI compatibility is not just about the device itself, but also about the conditions under which the MRI is performed.”
– Expert Opinion
|
Device Type |
MRI Compatibility |
Precautions |
|---|---|---|
|
Pacemaker |
Yes/No |
Specific guidelines for scanning |
|
ICD |
Yes/No |
Monitoring during procedure |
Radiation Therapy Considerations
Radiation therapy is another treatment that needs careful thought for those with pacemakers or ICDs. The main worry is that radiation could harm the device or make it malfunction.
We recommend the following precautions:
- Assessing the radiation dose that the device will be exposed to
- Shielding the device if possible
- Monitoring the device’s function during and after radiation therapy
Dental Procedures and Other Medical Treatments
Dental procedures and other treatments can also be risky for those with pacemakers or ICDs. While the risks are generally lower than with MRI or radiation therapy, precautions are necessary.
For dental procedures, it is recommended to:
- Inform the dentist about the presence of a pacemaker or ICD
- Avoid certain equipment that could potentially interfere with the device
- Follow any specific guidelines provided by the device manufacturer
In conclusion, individuals with pacemakers or ICDs must take precautions with medical procedures or imaging tests. By understanding the risks and following guidelines, we can ensure their safety and the success of their treatment.
Technology and Electronic Devices: Safety Guidelines
Electronic devices are everywhere in our lives. They are important for people with pacemakers or ICDs. It’s key to know how to use them safely.
Cell Phones and Wireless Devices
Cell phones and other wireless devices are common today. They are usually safe to use. But, to be extra careful, keep your phone 6 inches away from your pacemaker or ICD.
Don’t carry your phone in a pocket near your device. Also, use the ear opposite to your implant when talking on the phone.
Additional Precautions:
- Use a headset or speakerphone for calls to keep the phone away from your implant.
- Don’t place your phone near your chest or in a breast pocket when it’s on.
Household Appliances and Tools
Most household appliances are safe with a pacemaker or ICD. But, it’s smart to be careful. Don’t lean against or stand very close to big appliances while they’re running.
For things like microwave ovens, make sure they’re well-maintained. This helps prevent electromagnetic field leaks.
Safe Practices:
- Keep a safe distance from appliances when they’re in use.
- Make sure appliances are working well.
Industrial Equipment and Workplace Hazards
Working with industrial equipment can be risky. Some equipment can create strong electromagnetic fields. These fields might affect your pacemaker or ICD. Talk to your device maker and workplace safety experts to figure out the risks.
Workplace Safety Measures:
- Do a workplace check to find out about electromagnetic interference risks.
- Use protective gear or different tools when near risky equipment.
Travel Considerations for Patients with Cardiac Devices
Patients with cardiac devices can travel safely. It’s important to know the guidelines and preparations needed. Whether you’re going to a nearby city or traveling internationally, managing your device during travel is key.
Air Travel Guidelines and Preparations
Air travel is safe for those with pacemakers or ICDs. Tell the airline about your device when booking. You might need to show your device card or give device details at check-in or security.
Security checks, like metal detectors or full-body scanners, are usually safe. But, tell security about your device first. Handheld wands are safer for screening.
International Travel with a Pacemaker
When traveling abroad, research healthcare options at your destination. Check if your device’s manufacturer has a representative there. This can be helpful for technical support or assistance.
Essential Documentation to Carry
Always carry your device identification card. It has important details about your pacemaker or ICD. This card helps medical staff in emergencies.
Also, keep a list of your medications and emergency contacts. Having this information can improve care if you need it while traveling.
Exercise and Physical Activity: What’s Safe and What’s Not
Exercise is key to a healthy life, but it’s different for those with pacemakers or ICDs. Knowing what’s safe is important. Regular activity can help manage heart conditions and improve health. But, some activities might be risky, like device malfunction or injury.
So, it’s important to know which exercises are good and which to avoid.
Recommended Exercise Options
For those with cardiac devices, low-to-moderate intensity exercises are best. These include:
- Brisk walking
- Swimming
- Cycling
- Light aerobics
- Yoga (with certain precautions)
These activities are safe because they don’t have high-impact movements or contact. This reduces the risk of damage to the device or disruption of its function.
Sports and Activities to Avoid
While many activities are safe, some should be avoided by those with cardiac devices. This is because of the risks involved:
- Contact sports (e.g., football, hockey)
- High-impact aerobics
- Activities involving significant changes in elevation or pressure
- Sports that could result in direct blows to the chest area where the device is implanted
Avoiding these activities can prevent damage to the device. It ensures it continues to work correctly.
Monitoring Your Heart During Physical Activity
It’s important to watch your heart rate and overall health during exercise. This can be done through:
- Regular check-ups with your healthcare provider
- Using a heart rate monitor or fitness tracker designed for people with cardiac devices
- Paying attention to your body’s signals, such as dizziness, chest pain, or shortness of breath
By being aware of your body’s responses, you can adjust your exercise routine. This helps maximize benefits while minimizing risks.
|
Activity |
Safety Level |
Precautions |
|---|---|---|
|
Brisk Walking |
Safe |
Monitor heart rate |
|
Swimming |
Safe |
Avoid diving |
|
Cycling |
Safe |
Wear protective gear |
|
Contact Sports |
Not Recommended |
Avoid due to risk of device damage |
Understanding Shockable Rhythms and How Defibrillators Work
For people with certain heart conditions, knowing about shockable rhythms is key. These rhythms are abnormal and can be treated with a defibrillator. This device gives an electric shock to help the heart beat normally again.
There are two main types of shockable rhythms: ventricular fibrillation (VF) and ventricular tachycardia (VT). It’s important to know the difference to treat them right.
Ventricular Fibrillation vs. Ventricular Tachycardia
Ventricular fibrillation is a serious heart condition. It makes the heart’s ventricles quiver fast and erratically. This is very dangerous and needs quick treatment.
Ventricular tachycardia, on the other hand, is a fast heart rate from the ventricles. It can also be dangerous if not treated fast enough.
|
Condition |
Description |
Treatment |
|---|---|---|
|
Ventricular Fibrillation |
Rapid, erratic quivering of the ventricles |
Defibrillation |
|
Ventricular Tachycardia |
Fast heart rate originating in the ventricles |
Cardioversion or Defibrillation |
How ICDs Detect and Treat Dangerous Arrhythmias
Implantable Cardioverter Defibrillators (ICDs) are advanced devices. They watch the heart’s rhythm and can give a shock or pacing therapy to fix it.
ICDs are set to spot certain heart rhythms and act on them. If they find a dangerous rhythm, they give a shock to get the heart beating right again. This is key to stop sudden cardiac death.
What to Expect During and After a Shock Event
If an ICD shocks you, it’s good to know what happens. The device gives a brief electric shock to fix the heartbeat. After, you might feel some discomfort, but the device keeps watching the heart.
After a shock, it’s important to talk to a doctor. They can help manage the condition and make sure the ICD is working right.
Non-Shockable Rhythms and Their Clinical Management
Non-shockable rhythms, like PEA and asystole, are tough to handle in cardiac care. They need quick and effective treatment to help patients.
These rhythms don’t respond to defibrillation. Knowing about them is key for doctors to give the right care.
Pulseless Electrical Activity (PEA)
PEA means the heart should have a pulse but doesn’t. It can happen for many reasons, like too little blood or a blocked heart valve.
Fixing PEA means finding and treating the cause. This might include giving special medicines or fluids, or draining fluid from around the heart.
Asystole and Other Non-Shockable Conditions
Asystole, or flatline, means no heart activity at all. It’s very serious and needs quick action. Other non-shockable issues include slow heart rates or fake PEA.
Handling asystole means finding things that can be fixed and starting treatments like CPR and epinephrine.
How Medical Professionals Respond to These Rhythms
Doctors use set steps for non-shockable rhythms. The American Heart Association (AHA) guides them. This includes checking the ABCs, doing CPR, and giving medicines.
Good teamwork is vital in these situations. Working together can really help patients.
|
Condition |
Characteristics |
Management Strategies |
|---|---|---|
|
Pulseless Electrical Activity (PEA) |
Presence of electrical activity without a palpable pulse |
Identify and treat underlying cause, vasopressors, fluid resuscitation |
|
Asystole |
No cardiac electrical activity |
CPR, epinephrine administration, identify reversible causes |
It’s important for doctors to know about non-shockable rhythms and how to manage them. By sticking to guidelines and teaming up, they can make a big difference for patients.
Daily Life with a Cardiac Device
Getting a cardiac device is just the start. Learning to live with it is key for your health. There are many things to think about in your daily life with a pacemaker or ICD.
Clothing and Physical Comfort
What you wear matters a lot. Try to avoid tight clothes that might press on the device. Wearing loose shirts or dresses can help avoid irritation. Also, think about the device’s spot when you get dressed to avoid discomfort.
Sleeping Positions and Considerations
Sleeping on the side of the device can be uncomfortable. Try different sleeping positions to find what feels best. Using a supportive pillow or adjusting how you sleep can help with any issues.
Managing Device-Related Anxiety
It’s normal to feel nervous about having a cardiac device. Knowing how it works and being aware of it can help reduce anxiety. Activities like meditation or yoga can also help.
Intimacy and Relationships
A cardiac device shouldn’t stop you from being intimate. Talk openly with your partner about any worries. Knowing what the device can and can’t do helps keep your relationship strong.
Here are some tips for daily life with a cardiac device:
|
Activity |
Precautions |
Tips |
|---|---|---|
|
Exercise |
Avoid contact sports |
Choose low-impact activities like walking or swimming |
|
Dressing |
Avoid tight clothing |
Opt for loose-fitting clothes |
|
Sleeping |
Be mindful of device location |
Experiment with different sleeping positions |
By knowing these tips and taking the right steps, you can live a full and active life with a cardiac device. Always stay informed and talk to your healthcare team when you need to.
Device Monitoring and Follow-Up Care
Regular check-ups and device monitoring are key for those with cardiac devices. They ensure the device works right and safely. This care helps spot problems early, improving health outcomes.
Remote Monitoring Systems
Remote monitoring systems are vital for cardiac device management. They let doctors check on the device and patient health from afar. This cuts down on hospital visits. Remote monitoring can catch issues early, like battery running low or device problems, so doctors can act fast.
Many pacemakers and ICDs today have remote monitoring. This tech sends data to a secure server, where doctors can see it. It keeps the device and patient under constant watch, alerting everyone to any issues.
Regular Check-Up Schedule
Keeping up with regular check-ups is essential for cardiac device health. How often depends on the device, patient health, and doctor advice.
|
Device Type |
Typical Check-Up Frequency |
Key Checks |
|---|---|---|
|
Pacemaker |
Every 3-6 months |
Battery status, lead integrity, device function |
|
ICD |
Every 3-6 months |
Battery status, shock therapy readiness, device function |
Battery Life and Replacement Timing
Knowing your cardiac device’s battery life is important for planning replacements. The life span varies by device and use.
Pacemaker batteries last 5 to 15 years. ICDs usually need replacement every 5 to 7 years. Regular visits help keep track of battery life, ensuring timely replacements.
Signs That Warrant Immediate Medical Attention
While regular monitoring is important, some symptoms need quick medical help. It’s vital for patients to know these signs.
- Palpitations or irregular heartbeats
- Dizziness or fainting spells
- Swelling in the legs or feet
- Shortness of breath
- Pain or discomfort at the device site
Spotting these signs early can save lives. If any of these happen, patients should reach out to their doctor right away.
Communicating Your Medical Needs Effectively
Living with a cardiac device means more than just medical care. It’s about clear communication about your needs. This ensures your healthcare team, family, and friends understand your condition and the precautions needed. This understanding is key to getting the best support and care.
Medical ID Bracelets and Cards
Wearing a medical ID bracelet or carrying a card is a simple yet effective way to share your medical needs. These tools tell medical staff about your pacemaker or ICD, helping them act quickly in emergencies. Always wear a medical ID bracelet or carry a card.
Benefits of Medical ID:
- Immediate identification of your medical condition
- Informs healthcare providers about your cardiac device
- Ensures appropriate emergency response
Informing Family, Friends, and Coworkers
Telling your family, friends, and coworkers about your condition is also vital. Teaching them about your condition helps prevent misunderstandings and ensures they know how to help in emergencies. Consider having a meeting or sending information to your close contacts.
Emergency Response Planning
Having a plan for emergencies is essential. This plan should include your healthcare providers’ contact info, a list of medications, and details about your cardiac device. We help you create a personalized emergency plan that meets your needs.
Working with Your Healthcare Team
Your healthcare team is a great resource for managing your condition. Regular check-ups and open communication with your cardiologist and other healthcare professionals are key. We encourage you to ask questions, report any changes, and follow the recommended care schedule.
Effective communication is a two-way process. By keeping your healthcare team informed and proactive about your care, you can enjoy a better quality of life with your cardiac device.
|
Communication Method |
Description |
Benefits |
|---|---|---|
|
Medical ID Bracelet/Card |
Informs medical personnel about your cardiac device |
Immediate identification, appropriate emergency response |
|
Informing Family/Friends |
Educates close contacts about your condition and response |
Prevents misunderstandings, ensures correct response |
|
Emergency Response Plan |
Outlines steps to take in case of an emergency |
Ensures preparedness, quick response |
Conclusion
Knowing how to live with a pacemaker or ICD is key for a safe and healthy life. We’ve looked at the main differences between these devices, their roles, and safety tips for daily life. This includes security checks, medical procedures, and everyday activities.
By sticking to safety guidelines, people with these devices can avoid risks from electromagnetic interference. They can also make sure their devices work well with medical treatments. This way, they can live a pretty normal life.
It’s important to stay up-to-date and follow your doctor’s advice. Taking the right steps helps manage life with a pacemaker or ICD. This knowledge lets you make better choices for a better life.
We suggest talking to your doctor for specific advice on living with these devices. Following their safety tips is important for keeping your health safe.
FAQ
Can I go through a metal detector if I have a pacemaker or defibrillator?
It’s best to avoid metal detectors with a pacemaker or defibrillator. Tell security about your device. They might use a pat-down or a handheld wand instead.
What are the differences between a pacemaker and an implantable cardioverter-defibrillator (ICD)?
A pacemaker sends electrical impulses to control the heartbeat. An ICD can prevent sudden death by delivering an electric shock when needed.
How does electromagnetic interference (EMI) affect pacemakers and defibrillators?
EMI can mess with pacemakers and defibrillators, making them malfunction. Strong magnetic fields and some devices can cause this.
What activities should I avoid with a pacemaker?
Stay away from strong magnetic fields and high-impact sports. Always check with your doctor first.
Can I undergo an MRI if I have a pacemaker or ICD?
Some devices are safe for MRI under certain conditions. Always tell your doctor and the MRI place about your device.
How do ICDs detect and treat shockable rhythms like ventricular fibrillation?
ICDs watch the heart rhythm and shock it back to normal when needed. This is for dangerous arrhythmias like ventricular fibrillation.
What are non-shockable rhythms, and how are they managed?
Non-shockable rhythms need CPR and medicine, not a shock from an ICD. This includes pulseless electrical activity and asystole.
How can I manage anxiety related to my cardiac device?
Talk to your doctor, join a support group, and try relaxation techniques. These can help with device-related anxiety.
What should I do during a security screening at the airport with a pacemaker or ICD?
Tell security about your device before screening. They can use other methods. Having your device card ready is also helpful.
Are there specific exercises or physical activities I should avoid with a cardiac device?
Avoid high-impact sports and heavy lifting. Talk to your doctor about safe exercises for you.
How often should I have my cardiac device checked?
Check-ups depend on your device and condition. Your doctor will tell you how often, possibly including remote monitoring.
Why is it important to wear a medical ID bracelet or carry a device identification card?
A medical ID bracelet or card tells others about your device. This ensures you get the right care in emergencies.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/22041947/









