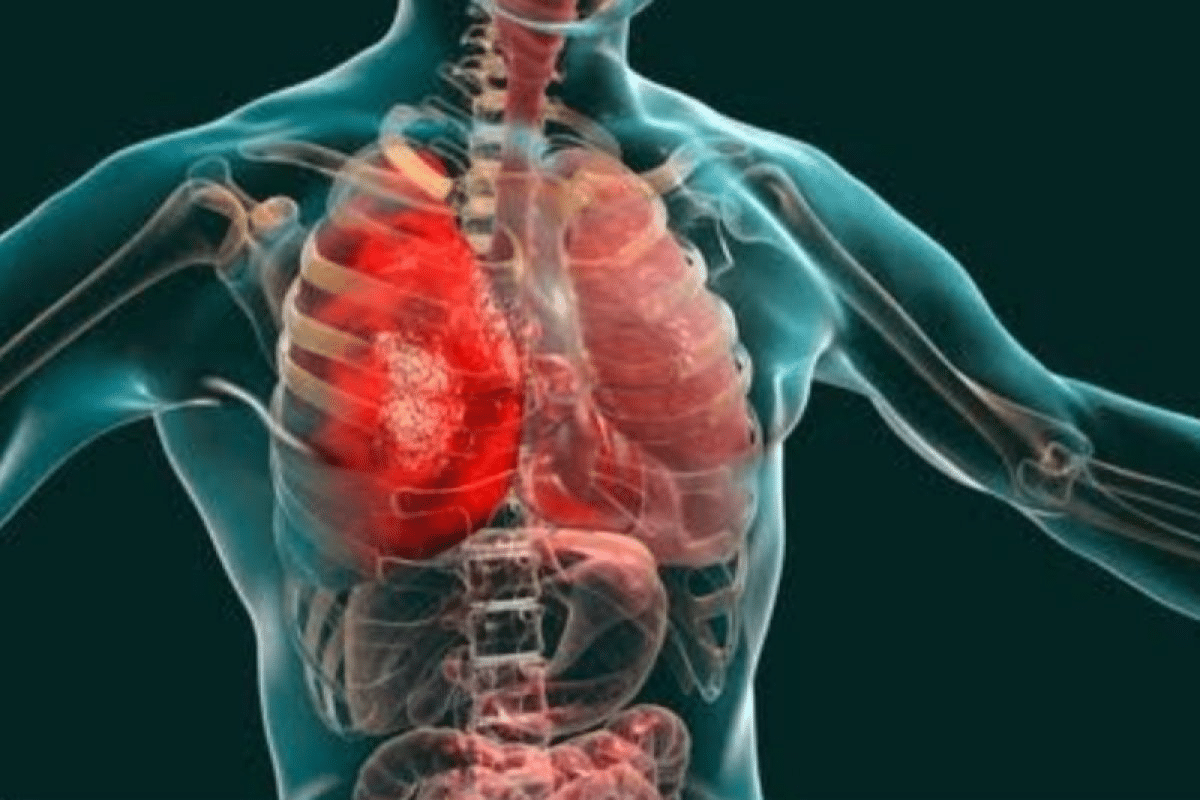
Pulmonology focuses on diagnosing and treating lung and airway conditions such as asthma, COPD, and pneumonia, as well as overall respiratory health.
Send us all your questions or requests, and our expert team will assist you.
Emphysema represents a pathological condition of the lungs characterized by the abnormal and permanent enlargement of the airspaces distal to the terminal bronchioles, accompanied by the destruction of their walls without obvious fibrosis. It is one of the two main conditions that constitute Chronic Obstructive Pulmonary Disease, the other being chronic bronchitis. While chronic bronchitis affects the conducting airways, emphysema destroys the lung parenchyma, the functional tissue responsible for gas exchange. The disease process involves the gradual disintegration of the delicate alveolar sacs, which are the sites where oxygen enters the bloodstream and carbon dioxide is eliminated. As these walls rupture, the surface area available for gas exchange is drastically reduced.
Furthermore, destruction of the alveolar attachments results in a loss of elastic recoil. In a healthy lung, elastic fibers tether the small airways open; in emphysema, these tethers are snapped, causing the airways to collapse during exhalation. This leads to air trapping, hyperinflation, and a significant increase in the work of breathing. At Liv Hospital, we define emphysema not just as a structural defect, but as a systemic inflammatory state that fundamentally alters the mechanics of respiration.
To understand the definition of emphysema, one must look at the microscopic level, where the battle between injury and repair occurs. The lung maintains a delicate balance between proteases, enzymes that break down proteins, and antiproteases, which inhibit them.
In a healthy individual, antiproteases like alpha-one antitrypsin protect the lung’s elastic fibers from degradation. In emphysema, this balance is tipped towards destruction. Inhaled irritants, particularly tobacco smoke, recruit inflammatory cells, including neutrophils, macrophages, and CD8 lymphocytes, into the lung. These cells release massive amounts of proteases, including neutrophil elastase, cathepsins, and matrix metalloproteinases. Simultaneously, the oxidants in smoke inactivate the protective antiproteases. The result is the unchecked digestion of the lung’s structural scaffolding, specifically elastin and collagen. This enzymatic destruction creates larger, flaccid air sacs that have lost their ability to bounce back after stretching.
The definition of the disease is clinically tied to the phenomenon of air trapping. Because the airways collapse during exhalation due to loss of elastic recoil, air cannot entirely escape the lungs. With each subsequent breath, more air is inhaled than is exhaled, leading to dynamic hyperinflation. This forces the diaphragm to flatten, putting the respiratory muscles at a severe mechanical disadvantage. The chest wall changes shape, becoming barrel-like, and the neck and shoulder muscles must be recruited to assist with breathing. This creates the sensation of breathlessness known as dyspnea, which is the hallmark of the condition.
Emphysema is not a uniform disease; it is classified into distinct subtypes based on the specific part of the acinus (the functional unit of the lung) that is affected.
While the majority of cases are acquired through environmental exposure, a significant minority are genetic. Alpha-1 antitrypsin deficiency is an inherited disorder that predisposes individuals to early-onset panlobular emphysema.
Emphysema is a major contributor to the global burden of chronic respiratory disease. It affects millions of people worldwide and is a leading cause of disability and death. The prevalence is expected to rise due to the aging population and the continued use of tobacco products in many developing nations. While historically considered a disease of older men, the prevalence in women is increasing, reflecting changes in smoking habits over the past few decades and potentially a higher biological susceptibility to tobacco smoke. The disease imposes a significant economic burden due to healthcare costs, hospitalizations, and lost productivity. It is also associated with significant comorbidities, including cardiovascular disease, lung cancer, and osteoporosis, which are driven by the same systemic inflammatory processes.
It is essential to distinguish pulmonary emphysema from subcutaneous emphysema, although they share a name. Subcutaneous emphysema refers to the presence of air or gas beneath the skin.
Historically, emphysema was defined strictly by pathological findings at autopsy. With the advent of high-resolution computed tomography, the definition has evolved to include radiological characteristics that enable in vivo diagnosis and quantification. Modern medicine views emphysema as a component of a heterogeneous syndrome. We now understand that patients can have varying degrees of emphysema and airway disease, and treating the specific phenotype is key to successful management. At Liv Hospital, we use this nuanced definition to move beyond a one-size-fits-all approach, recognizing that emphysema is a complex interaction among genetics, environment, and aging.


Send us all your questions or requests, and our expert team will assist you.
CT scans use X-rays to create detailed cross-sectional images and are excellent for visualizing kidney stones, detecting tumors, and evaluating traumatic injuries. They are fast and widely available. MRI uses strong magnetic fields and radio waves to produce detailed images of soft tissues, making it superior for staging prostate cancer, evaluating bladder wall invasion, and assessing pelvic floor disorders without ionizing radiation.
Contrast dye, usually iodine-based, is injected into a vein to highlight the blood vessels and urinary tract organs. As the kidneys filter the dye from the blood, it opacifies the urine. This allows the radiologist to see the internal structure of the kidneys, the ureters, and the bladder clearly, revealing blockages, tumors, or structural abnormalities that would be invisible on a non-contrast scan.
Multiparametric MRI is an advanced imaging technique that combines standard anatomical sequences with functional sequences like Diffusion-Weighted Imaging and Dynamic Contrast-Enhanced imaging. This provides a comprehensive assessment of the prostate, allowing doctors to distinguish between benign conditions like BPH and significant prostate cancer, and to guide targeted biopsies.
CT scans do involve exposure to ionizing radiation, which carries a small theoretical risk of cellular damage over time. However, modern CT scanners use dose-modulation technology to minimize this exposure to the lowest level necessary for a diagnostic image. The benefit of an accurate and timely diagnosis for serious urological conditions typically far outweighs the minimal risk of radiation.
Many modern orthopedic implants are MRI-safe, although they may cause some image distortion. However, older pacemakers, defibrillators, and certain metal clips may be unsafe in the strong magnetic field. It is critical to inform the imaging team of any metallic implants so they can verify their safety compatibility or recommend an alternative test like a CT scan.


Allergies are a common reason for red eyes, affecting millions each year. During allergy season, eyes can become itchy, red, and watery. This can really

Get rid of a deep chest cough fast. Discover 5 best relief solutions that break up mucus and soothe the irritation effectively. A cough that
Detailed cap disease definition, covering its infectious etiology and the common pathogens involved in its development. Community-acquired pneumonia (CAP) is a serious lung infection that

Understand COPD death and end stages. Learn critical facts about final symptoms and the importance of palliative care during decline. End-stage COPD, also known as


Sleep disorders are a big health problem worldwide. They affect millions, including about 70 million Americans. These issues can really change how we live our

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)