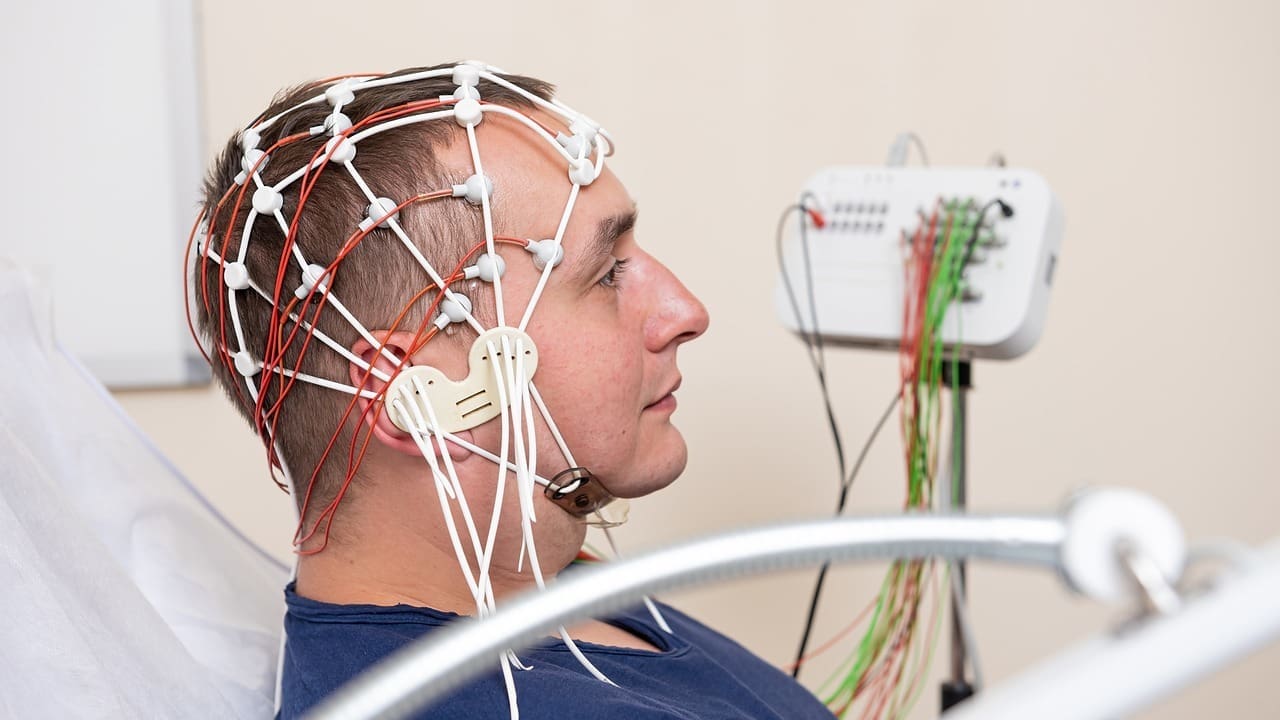
Neurology diagnoses and treats disorders of the nervous system, including the brain, spinal cord, and nerves, as well as thought and memory.
Send us all your questions or requests, and our expert team will assist you.
Symptoms of demyelinating diseases arise from impaired nerve signal transmission caused by damage to the myelin sheath. Because myelin loss can occur in different regions of the central or peripheral nervous system, symptom patterns vary widely. From a neurological standpoint, symptoms reflect the location, extent, and activity of demyelination rather than a single uniform clinical picture.

Demyelination disrupts the speed and reliability of neural communication, leading to symptoms that may fluctuate over time and worsen under physiological stress.
These symptoms may appear suddenly in acute demyelinating disease or develop gradually in chronic forms.

Motor pathways are particularly vulnerable to demyelination due to their reliance on rapid signal conduction.
Weakness may fluctuate and often worsens with heat, infection, or prolonged exertion, reflecting reduced conduction efficiency in demyelinated fibers.
Sensory pathways commonly exhibit demyelinating involvement, producing a range of abnormal sensations.
These symptoms can be persistent or episodic and may spread over time as additional pathways are affected.
Demyelination involving optic nerves or brainstem pathways produces distinctive symptom patterns.
Visual symptoms are often among the earliest signs in central nervous system demyelinating disease

When demyelination affects brain regions involved in cognition, higher neurological functions may be impaired.
These changes may be subtle initially and become more apparent during complex tasks or multitasking.
Some demyelinating diseases affect autonomic pathways, leading to systemic symptoms.
Autonomic symptoms often indicate more extensive nervous system involvement.
Risk factors reflect genetic susceptibility, immune system behavior, and environmental influences that increase vulnerability to myelin damage.
These factors influence immune recognition of myelin and inflammatory response intensity.
Non genetic factors also contribute to demyelinating disease risk.
These influences may act as triggers rather than direct causes.
Demyelinating diseases can present at any age, though many central nervous system demyelinating conditions appear in young or middle adulthood. Peripheral demyelinating diseases may occur later or follow immune activation events.
Age at onset helps narrow diagnostic consideration but does not determine disease severity or outcome.
Early recognition of demyelinating symptoms allows timely neurological evaluation and management. Because myelin damage may be partially reversible in early stages, prompt assessment can reduce long term neurological impairment.
Subtle sensory changes, visual disturbances, or unexplained weakness should not be ignored when persistent or progressive.

Send us all your questions or requests, and our expert team will assist you.
Early symptoms often include sensory changes, visual disturbance, or limb weakness. Fatigue may also be an early feature.
Not always. Some demyelinating diseases follow a relapsing pattern with periods of improvement.
Yes, increased body temperature and stress can temporarily worsen symptoms by reducing nerve conduction efficiency.
They may be symmetrical or asymmetrical depending on disease type and lesion location.
Risk is higher in individuals with autoimmune susceptibility, certain environmental exposures, or prior immune activation events.






Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)