Neurology diagnoses and treats disorders of the nervous system, including the brain, spinal cord, and nerves, as well as thought and memory.
Send us all your questions or requests, and our expert team will assist you.
Diagnosis of demyelinating diseases is a structured neurological process that aims to confirm myelin injury, determine its anatomical distribution, identify the underlying mechanism, and distinguish demyelination from other neurological conditions with similar presentations. Because symptoms can be variable and fluctuating, accurate diagnosis relies on integration of clinical evaluation, neuroimaging, and supportive laboratory and neurophysiological findings rather than a single definitive test.

The diagnostic approach begins with establishing whether symptoms are consistent with impaired myelin dependent signal transmission. Neurologists assess the pattern, timing, and progression of symptoms to determine whether they align with central or peripheral demyelination.
Key diagnostic considerations include
• Acute versus chronic symptom onset
• Relapsing, progressive, or monophasic course
• Focal versus multifocal neurological deficits
• Central nervous system versus peripheral nervous system involvement
These elements guide subsequent imaging and testing strategies.

Clinical examination remains a critical component of diagnosis and helps localize dysfunction even before imaging is performed.
Clinical findings help narrow differential diagnosis and inform interpretation of imaging results.
Imaging plays a central role in confirming demyelination, assessing disease burden, and excluding alternative causes such as vascular, neoplastic, or infectious processes. Among imaging modalities, magnetic resonance imaging is the most important diagnostic tool.

MRI is the imaging modality of choice for evaluating demyelinating diseases of the central nervous system. It provides high resolution visualization of white matter and allows detection of lesions consistent with myelin loss.
MRI findings may include
• Hyperintense white matter lesions on T2 weighted images
• Lesions in characteristic anatomical locations
• Evidence of active inflammation with contrast enhancement
• Dissemination of lesions in space and time
The distribution and appearance of lesions provide essential diagnostic clues.
Central nervous system demyelinating diseases often show lesions in specific regions that reflect vulnerability of myelinated pathways.
Commonly involved areas include
• Periventricular white matter
• Juxtacortical regions
• Brainstem and cerebellum
• Spinal cord
• Optic nerves
Recognition of these patterns helps distinguish demyelinating disease from nonspecific white matter changes.
MRI can differentiate between active inflammatory demyelination and older, inactive lesions.
Active lesions may show
• Contrast enhancement indicating blood brain barrier disruption
• Edema surrounding lesions
• Clinical correlation with recent symptom onset
Chronic lesions often appear as stable areas of signal change without enhancement and may reflect past disease activity.
This distinction is important for understanding disease stage and activity rather than for establishing diagnosis alone.
Some demyelinating diseases produce large lesions that mimic tumors or abscesses on imaging. These tumefactive demyelinating lesions can present diagnostic challenges.
Features that suggest demyelination rather than neoplasm include
• Incomplete ring enhancement
• Lesion location along white matter tracts
• Clinical course inconsistent with rapidly growing tumors
Careful correlation with clinical findings and follow up imaging is essential in such cases.
Peripheral demyelinating diseases are not primarily diagnosed with brain MRI. Instead, imaging may be used to evaluate nerve roots or exclude compressive pathology.
MRI of the spine may show
• Nerve root thickening
• Enhancement of nerve roots in inflammatory demyelination
• Secondary spinal cord changes
However, peripheral demyelination is more directly assessed through neurophysiological testing.
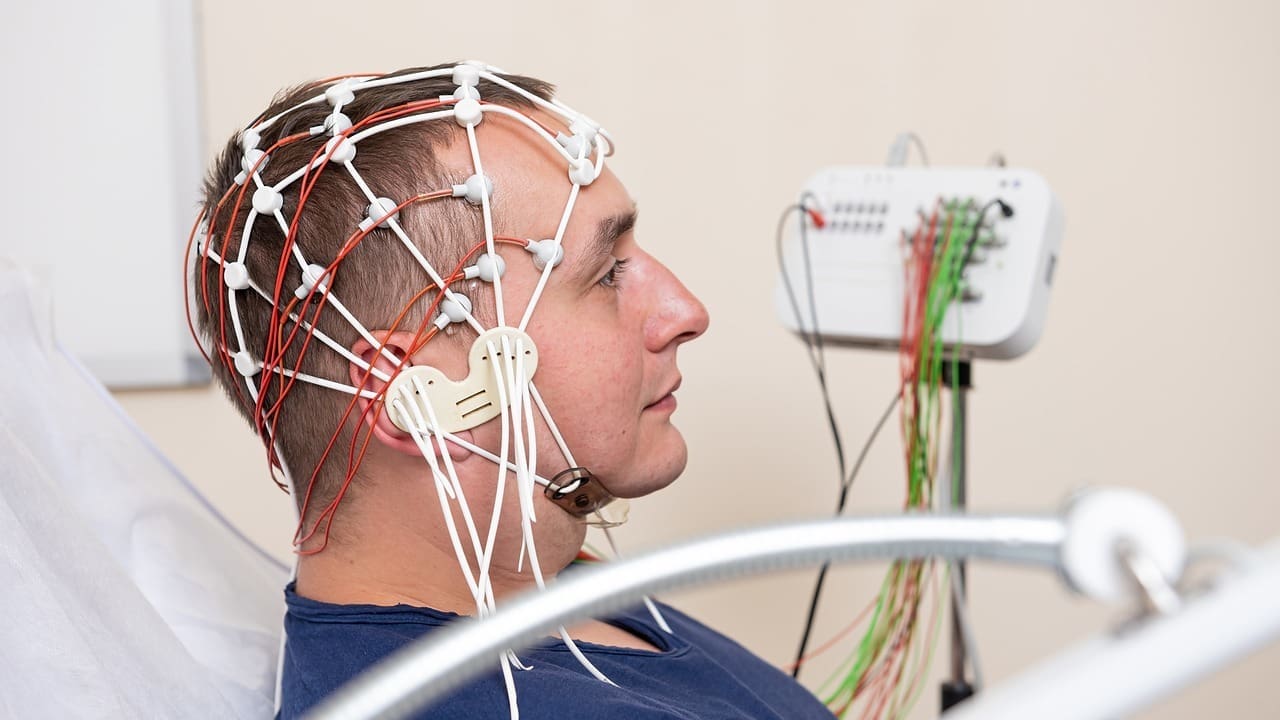
Neurophysiological testing plays a crucial supportive role, especially in peripheral demyelinating diseases.
Nerve conduction studies evaluate the speed and pattern of electrical signal transmission along peripheral nerves.
Findings suggestive of demyelination include
• Markedly slowed conduction velocities
• Prolonged dLaboratory And Supportive Testingistal latencies
• Conduction block
• Temporal dispersion of signals
These features distinguish demyelinating neuropathies from axonal neuropathies.
Additional testing may support diagnosis or help identify underlying mechanisms.
Supportive evaluations may include
• Cerebrospinal fluid analysis showing inflammatory markers
• Immune related testing when autoimmune disease is suspected
• Metabolic evaluation to exclude reversible causes
These tests complement imaging and clinical assessment but are not diagnostic in isolation.
A key diagnostic task is differentiating demyelinating diseases from other conditions with overlapping features.
Important considerations include
• Vascular white matter disease
• Neurodegenerative disorders
• Infectious or inflammatory encephalopathies
• Metabolic or toxic leukoencephalopathies
• Structural lesions such as tumors
Accurate diagnosis depends on integrating imaging patterns with clinical presentation and disease course.
Demyelinating diseases often evolve over time. Follow up imaging helps demonstrate dissemination of lesions or stability, which supports diagnostic confidence and informs management.
Serial MRI allows
• Monitoring of disease activity
• Identification of new lesions
• Assessment of treatment response
• Differentiation between active and inactive disease
Longitudinal assessment is often more informative than a single imaging study.
Normal imaging does not fully exclude demyelinating disease, particularly early in the course or in predominantly peripheral conditions. Conversely, imaging abnormalities may be incidental and unrelated to symptoms.
Diagnosis therefore relies on careful interpretation rather than imaging findings alone.
Clear explanation of diagnostic findings helps individuals understand the neurological basis of their symptoms. Framing imaging results within the context of myelin dysfunction supports realistic expectations and informed long term planning.
Accurate diagnosis also prevents unnecessary testing and reduces uncertainty during early disease stages.

Send us all your questions or requests, and our expert team will assist you.
No, white matter lesions can result from vascular, metabolic, or degenerative causes. Pattern and context are critical.
Not always. Early or peripheral demyelinating diseases may show minimal or no central imaging changes.
Demyelinating diseases evolve over time. Follow up imaging helps demonstrate disease activity or progression.
Imaging provides information about lesion burden and location but does not fully predict clinical outcome.






Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)