Learn how Stroke Medicine specialists diagnose conditions using CT and MRI scans. Understand the examination process and how doctors locate the brain injury.
Send us all your questions or requests, and our expert team will assist you.
Diagnosis and Imaging
Diagnosing a stroke must happen very quickly. When a patient arrives at the hospital with suspected stroke symptoms, the medical team immediately activates a stroke protocol. The diagnosis is based on a combination of physical examination, imaging tests, and blood tests. The primary goal is to determine if the stroke is ischemic or hemorrhagic, as the treatments are opposites.
The doctor will first assess the patient’s medical history and the time the symptoms started. This “last known well” time is crucial for determining eligibility for certain treatments. The team will rule out other conditions that mimic stroke, such as low blood sugar, migraines, or seizures.
A stroke examination is a focused neurological assessment. In the emergency setting, doctors often use the National Institutes of Health Stroke Scale (NIHSS). This tool gives a score to the severity of the stroke. The exam is designed to be rapid and repeatable to monitor changes in the patient’s condition.
The exam focuses on:

During the examination, the doctor will ask the patient to perform specific tasks. They will ask the patient to smile to check for facial droop. They will hold up fingers and ask the patient to track them with their eyes. The patient will be asked to lift their arms and hold them up to check for drift or weakness.
The doctor will test sensation by touching the patient’s arms and legs with a pin or cotton swab. They will ask the patient to name objects, read a sentence, or repeat a phrase to check for aphasia. They will also listen to the heart for irregular rhythms and to the neck arteries for swooshing sounds that indicate narrowing.
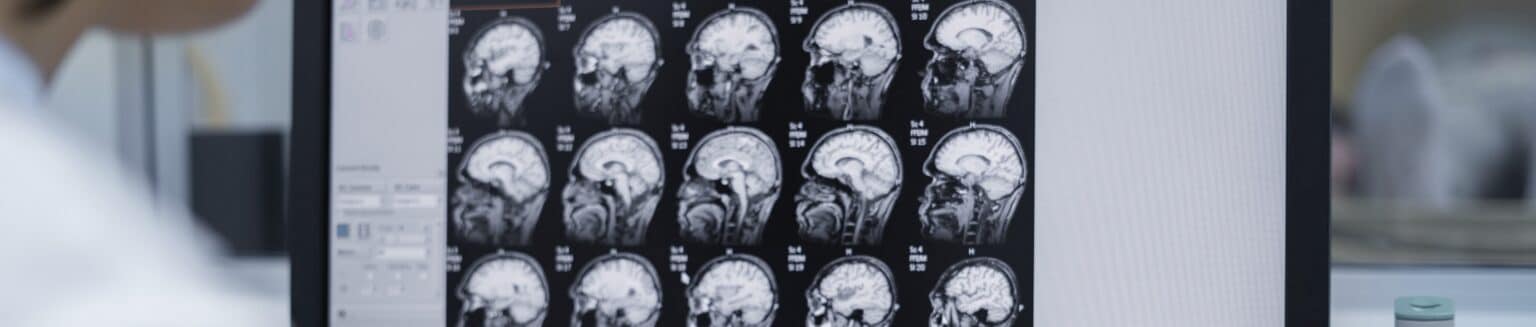
A Computerized Tomography (CT) scan is usually the first imaging test done. It uses X rays to create a detailed image of the brain. The main purpose of the initial CT scan is to rule out bleeding. It can quickly show if the patient is having a hemorrhagic stroke.
A CT scan is fast and available in most emergency rooms. If the CT scan does not show bleeding, and the symptoms suggest stroke, the doctors usually assume it is an ischemic stroke and proceed with treatment. Sometimes a CT angiogram is added, where dye is injected to visualize the blood vessels in the brain and neck.
Magnetic Resonance Imaging (MRI) uses strong magnetic fields and radio waves to create a very detailed view of the brain. An MRI is more sensitive than a CT scan and can detect ischemic strokes earlier. It can show the exact location and size of the damaged tissue.
An MRI is particularly useful for detecting small strokes or strokes in the back of the brain that might be missed on a CT scan. However, it takes longer to perform than a CT scan and may not be the first choice if time is extremely critical or if the patient has metal implants.
A carotid ultrasound is a non invasive test that uses sound waves to create images of the inside of the carotid arteries in the neck. These arteries supply blood to the front part of the brain. The test checks for the buildup of fatty deposits called plaque and for blood flow.
Narrowing of these arteries, known as stenosis, is a major cause of ischemic strokes. If significant narrowing is found, it may explain the cause of the stroke and indicate the need for surgery or stenting to prevent future strokes.
A cerebral angiogram is a more invasive procedure that provides a detailed map of the brain’s blood vessels. A thin tube called a catheter is inserted through a small incision in the groin or wrist and guided up to the brain. A dye is injected, and X rays are taken.
This test allows doctors to see the exact location of a blockage or a bleed. It is often done during the treatment phase of a stroke, specifically when mechanical thrombectomy or aneurysm repair is being considered. It gives the most accurate picture of the vascular anatomy.
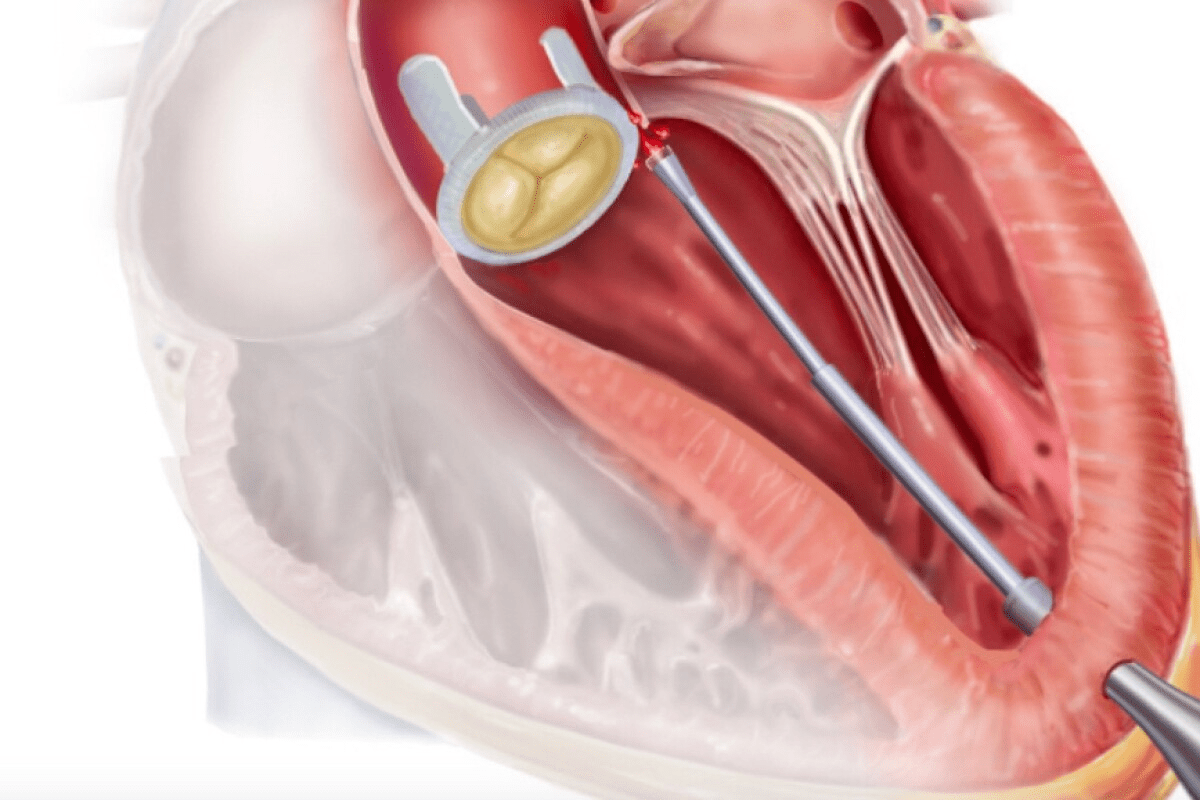
An echocardiogram is an ultrasound of the heart. Since many strokes are caused by blood clots that form in the heart and travel to the brain, checking the heart is essential. This test uses sound waves to create moving pictures of the heart.
Doctors look for sources of clots, such as thrombus inside the heart chambers. They also check for valve problems or a hole between the heart chambers (patent foramen ovale) that could allow clots to cross over and reach the brain.
Blood tests give the care team vital information about the patient’s overall health and potential stroke causes. A blood glucose test is done immediately because low blood sugar can mimic stroke symptoms. A platelet count and clotting tests measure how fast the blood clots, which is critical if clot busting drugs are being considered.
Doctors also check cholesterol levels to assess cardiovascular risk. Inflammatory markers might be checked to see if vasculitis (inflammation of blood vessels) is a cause. In younger patients, tests for genetic clotting disorders may be ordered.
After the initial phase, doctors need to determine if an irregular heart rhythm caused the stroke. A standard ECG captures the heart rhythm for only a few seconds. A Holter monitor is a portable device that the patient wears for 24 to 48 hours, or even longer.
It records the heart’s electrical activity continuously. This helps detect paroxysmal atrial fibrillation, which is an irregular heartbeat that comes and goes. Detecting this is crucial because it changes the long term medication plan to include strong anticoagulants.

Send us all your questions or requests, and our expert team will assist you.
For stroke imaging, the contrast is usually injected into a vein, not drunk; it lights up the blood vessels on the scan so doctors can see exactly where the blockage is.
Older pacemakers are dangerous in an MRI, but many modern devices are “MRI conditional,” meaning they can be scanned safely if specific protocols are followed by the technician.
A bubble study is done during an echocardiogram; salt water with tiny bubbles is injected into a vein to see if the bubbles cross a hole in the heart to the other side.
A carotid ultrasound cannot see the brain itself, but it is excellent for checking the carotid arteries in the neck to see if plaque buildup there caused the stroke.
This means a blood clot has blocked one of the main, large arteries supplying the brain; these strokes are the most dangerous but also the most treatable with mechanical removal.

Cardiac ablation is a procedure to treat irregular heartbeats. It’s generally safe but comes with risks, like stroke. A study found that the risk of

Nearly 90,000 carotid endarterectomy procedures are done every year in the United States. This shows how important it is to know about the recovery process

Having a Transient Ischemic Attack (TIA), also known as a mini stroke, is a serious warning. It’s a short-term issue that doesn’t cause lasting harm.

Research shows that strokes are most likely to occur in the early morning hours, around 6:30 am. This timing is not a coincidence. Our circadian
Find the right stroke ICD codes for cerebrovascular disease. This is the essential guide for medical billing and coding professionals. Cerebrovascular disease is a significant

About 75% of strokes happen to people aged 65 and older. This makes it a big health issue for seniors. Knowing how to help them

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)