Learn what a stroke is and how Stroke Medicine saves lives. Understand the difference between ischemic and hemorrhagic stroke and the role of neurologists.
Send us all your questions or requests, and our expert team will assist you.
Overview and Definition
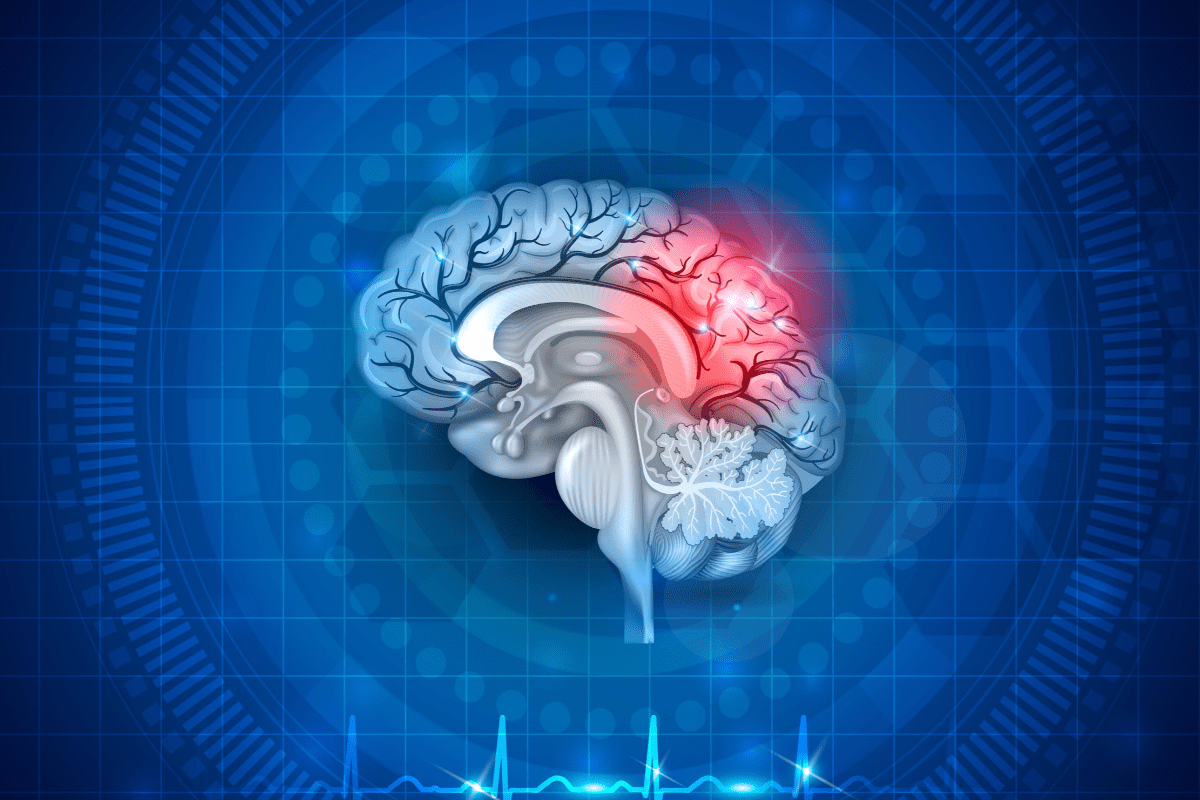
A stroke is often referred to as a brain attack and it occurs when the blood supply to part of your brain is interrupted or reduced preventing brain tissue from getting oxygen and nutrients. When asking what is a stroke it is critical to understand that brain cells begin to die in minutes. It is a medical emergency and prompt treatment is crucial.
Early action can reduce brain damage and other complications. The condition affects the arteries leading to and within the brain. It is the number five cause of death and a leading cause of disability in the United States. A stroke can happen to anyone at any time regardless of race sex or age.
There are two main causes of stroke a blocked artery or leaking or bursting of a blood vessel. Some people may have only a temporary disruption of blood flow to the brain known as a transient ischemic attack or TIA which does not cause lasting symptoms. Ischemic strokes are the most common type accounting for about eighty seven percent of all cases.
They occur when the arteries to your brain become narrowed or blocked causing severely reduced blood flow known as ischemia. Hemorrhagic strokes occur when a blood vessel in the brain leaks or ruptures. Brain hemorrhages can result from many conditions that affect your blood vessels including uncontrolled high blood pressure overtreatment with anticoagulants and aneurysms.
Symptoms and Risk Factors

The most effective way to recognize the symptoms is to remember the acronym FAST which stands for Face Arms Speech and Time. Face refers to drooping on one side of the face when the person tries to smile.
Arms refers to weakness or numbness in one arm where if the person tries to raise both arms one drifts downward. Speech refers to slurred or strange speech where the person may not be able to repeat a simple phrase. Time indicates that if you see any of these signs you must call emergency services immediately.
Other symptoms include sudden numbness or weakness in the leg confusion trouble seeing in one or both eyes sudden severe headache with no known cause and trouble walking or loss of balance.
Many factors can increase your risk of a stroke. Some factors can also increase your chances of having a heart attack. Potentially treatable risk factors include high blood pressure which is the single most important treatable risk factor.
Cigarette smoking or exposure to secondhand smoke increases the risk of stroke. High cholesterol diabetes and obstructive sleep apnea are also significant contributors. Cardiovascular disease including heart failure heart defects heart infection or abnormal heart rhythm such as atrial fibrillation carries a high risk.
Personal or family history of stroke or TIA also elevates the risk. COVID 19 infection has also been linked to an increased risk of ischemic stroke. Lifestyle factors such as physical inactivity heavy drinking and use of illegal drugs like cocaine and methamphetamine are major avoidable risks.
Diagnosis and Imaging
When you arrive at the hospital your emergency team will need to assess your condition quickly to determine the type of stroke you are having. They will perform a physical exam and check your blood pressure. The doctor will listen to your carotid arteries in your neck with a stethoscope to check for a rushing sound called a bruit that suggests altered blood flow.
They will ask about your medical history and when your symptoms started. This timing is critical because some treatment options are only effective if given within a short window after symptoms begin. They will also check your eyes specifically the blood vessels at the back of the eye which can provide clues about high blood pressure and other vascular issues.
Diagnostic imaging is essential to differentiate between an ischemic stroke and a hemorrhagic stroke as the treatments are vastly different. A computerized tomography or CT scan uses a series of X rays to create a detailed image of your brain.
A CT scan can show a hemorrhage a tumor stroke and other conditions. Magnetic resonance imaging or MRI uses powerful radio waves and magnets to create a detailed view of your brain. An MRI can detect brain tissue damaged by an ischemic stroke and brain hemorrhages. Carotid ultrasound uses sound waves to create detailed images of the inside of the carotid arteries in your neck to check for buildup of fatty deposits called plaques. Cerebral angiogram involves inserting a thin flexible tube through a small incision usually in your groin and guiding it through your major arteries to inject dye and view blood vessels in the brain.
Treatment and Rehabilitation
Emergency treatment depends on the type of stroke. For an ischemic stroke doctors must restore blood flow to the brain quickly. This is often done with emergency IV medication. Tissue plasminogen activator or tPA is the gold standard treatment. An injection of tPA is usually given through a vein in the arm within the first three to four and a half hours.
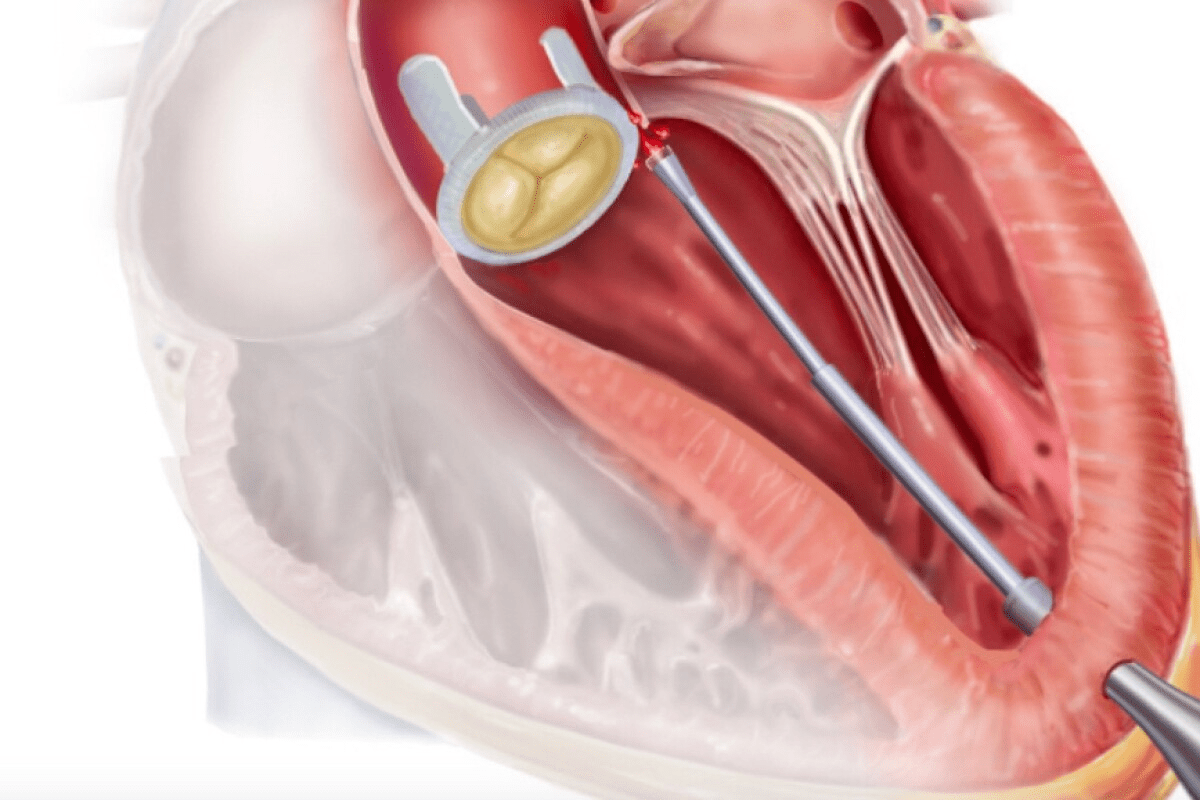
Emergency endovascular procedures may also be used such as removing the clot directly with a stent retriever in a procedure called a mechanical thrombectomy. For hemorrhagic stroke treatment focuses on controlling the bleeding and reducing pressure in the brain. Surgery may be performed to clip an aneurysm or coil it to prevent rupture. If the bleeding is caused by an arteriovenous malformation doctors may remove it surgically if it is accessible.
After emergency treatment stroke care focuses on helping you recover as much function as possible and return to independent living. The impact of the stroke depends on the area of the brain involved and the amount of tissue damaged. Rehabilitation may include speech therapy to help with problems producing or understanding language.
Physical therapy uses exercises to help you relearn movement and coordination skills you may have lost. Occupational therapy focuses on improving your ability to perform daily activities such as eating drinking dressing bathing reading and writing. Psychological evaluation and treatment may be necessary to test your thinking skills and monitor for depression which is common after a stroke.

Long-Term Care
Recovering from a stroke can be a long process and requires patience and hard work. Managing the underlying conditions that caused the stroke is vital to prevent a second one. This often means taking medications for the rest of your life to lower blood pressure and cholesterol or to thin the blood. Lifestyle changes are equally important.
Quitting smoking maintaining a healthy weight eating a diet rich in fruits and vegetables and limiting alcohol can significantly reduce risk. Regular exercise is recommended typically at least thirty minutes of moderate activity most days of the week. Joining a support group can be very beneficial for emotional health as connecting with others who understand the experience can reduce feelings of isolation.
Long term care also involves managing the lasting effects of the stroke. Many survivors experience paralysis or weakness on one side of the body which may require the use of a cane walker or brace. Trouble with swallowing known as dysphagia is common and may require dietary changes to prevent aspiration pneumonia.
Vision problems may persist requiring adaptive strategies. Cognitive changes such as memory loss or trouble concentrating can affect the ability to return to work. Emotional changes are also frequent including pseudobulbar affect where a person laughs or cries uncontrollably at inappropriate times. Addressing these complications with a multidisciplinary team is essential for maximizing quality of life.

Send us all your questions or requests, and our expert team will assist you.
A “mini stroke” is a lay term for a Transient Ischemic Attack, where stroke symptoms occur but resolve completely within 24 hours because the blockage was temporary.
While you cannot inherit a stroke directly, you can inherit risk factors such as high blood pressure, diabetes, and heart conditions that significantly increase your chance of having one.
Yes, having a stroke is the biggest risk factor for having another one; about one in four stroke survivors will have a recurrent event within five years without proper management.
“Time is brain” means that for every minute a stroke is left untreated, millions of brain cells die, so faster treatment directly results in less disability and a better chance of recovery.
Chronic stress can increase blood pressure and inflammation, which are major risk factors for stroke, and acute extreme stress can sometimes trigger an event in vulnerable individuals.

Cardiac ablation is a procedure to treat irregular heartbeats. It’s generally safe but comes with risks, like stroke. A study found that the risk of

Nearly 90,000 carotid endarterectomy procedures are done every year in the United States. This shows how important it is to know about the recovery process

Having a Transient Ischemic Attack (TIA), also known as a mini stroke, is a serious warning. It’s a short-term issue that doesn’t cause lasting harm.

Research shows that strokes are most likely to occur in the early morning hours, around 6:30 am. This timing is not a coincidence. Our circadian
Find the right stroke ICD codes for cerebrovascular disease. This is the essential guide for medical billing and coding professionals. Cerebrovascular disease is a significant

About 75% of strokes happen to people aged 65 and older. This makes it a big health issue for seniors. Knowing how to help them

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)