Last Updated on October 21, 2025 by mcelik
Autoimmune hemolytic anemia (AIHA) affects about 1 in 100,000 people each year. This shows how important it is to know about autoimmune blood disorders. We’re exploring the complex world of these conditions, where the immune system mistakenly attacks healthy red blood cells.
These disorders, like AIHA, are a big deal in hematology. The immune system is meant to protect us, but in autoimmune diseases, it attacks our own cells. It’s key to understand how these conditions work to find good treatments.
Key Takeaways
- Autoimmune hemolytic anemia (AIHA) is a rare condition where the immune system attacks red blood cells.
- Understanding autoimmune blood disorders is essential for effective management and treatment.
- Treatments for AIHA include medication, surgery, or blood transfusions.
- Autoimmune diseases occur when the body’s immune response turns against its own cells.
- Hematology plays a critical role in diagnosing and treating blood-related autoimmune disorders.
The Immune System and Blood: A Complex Relationship
It’s key to grasp how the immune system and blood cells work together. The immune system fights off infections and diseases. But, it can sometimes harm blood cells, leading to serious issues.
Normal Immune Function in Blood Regulation
The immune system is vital for keeping blood cells in check. White blood cells fight infections, and red blood cells carry oxygen. It works by:
- Spotting and getting rid of harmful invaders
- Controlling blood cell production and destruction
- Keeping the body from attacking itself
When it works right, the immune system keeps us safe. But, in autoimmune diseases, it goes wrong.
When Protection Becomes Destruction
In autoimmune diseases, the immune system attacks the body’s own cells. This can cause autoimmune hemolytic anemia or immune thrombocytopenia. The reasons are complex, involving genes, environment, and immune system problems.
Knowing how this happens helps us find better treatments. These treatments aim to fix the immune system and protect blood cells.
Understanding Autoimmune Blood Disorders

It’s key to understand autoimmune blood disorders to diagnose and treat them well. These disorders happen when the immune system attacks the body’s own blood cells. This leads to health problems.
Definition and Classification
Autoimmune hemolytic anemia (AIHA) is a common autoimmune blood disorder. It’s when the body’s immune system attacks its own red blood cells. This is due to autoantibodies against these cells.
These disorders can be grouped by the type of blood cell attacked and the immune response. Knowing this helps doctors understand the condition better and choose the right treatment.
For example, AIHA can be warm or cold, based on when the autoantibodies work best. This helps in tailoring treatment plans.
Prevalence and Demographics
Autoimmune blood disorders are not common in all people. Some, like AIHA, are rare. Others might affect certain groups more.
Knowing who is most affected helps doctors find and treat these disorders early. It also helps in creating treatments that work best for those groups.
| Disorder | Prevalence | Commonly Affected Demographics |
| AIHA | 1-3 per 100,000 per year | Women, individuals with autoimmune diseases |
| Immune Thrombocytopenia (ITP) | 2-4 per 100,000 per year | Children, women under 40 |
Common Risk Factors
There are several risk factors for autoimmune blood disorders. These include genetics, environmental factors, and other autoimmune diseases.
Knowing these risk factors helps in catching and treating these disorders early. For instance, people with a family history of autoimmune diseases are at higher risk.
- Genetic predisposition
- Presence of other autoimmune diseases
- Environmental triggers
Understanding these factors and the nature of autoimmune blood disorders helps doctors manage and treat them better.
Autoimmune Hemolytic Anemia (AIHA)
Autoimmune Hemolytic Anemia (AIHA) is a condition where the immune system attacks and destroys red blood cells. This can greatly affect a person’s life, making it important to know about its types, how to diagnose it, and treatment options.
Types of AIHA: Warm vs. Cold
AIHA is divided into two types based on when the autoantibodies attack red blood cells: Warm AIHA and Cold AIHA.
Warm AIHA is more common. Autoantibodies bind to red blood cells at body temperature, marking them for destruction. It’s often linked to other autoimmune diseases or lymphoproliferative disorders.
Cold AIHA happens when autoantibodies react with red blood cells at lower temperatures. It can be caused by infections or certain medications.
Diagnostic Criteria
To diagnose AIHA, doctors use a mix of clinical evaluation, lab tests, and sometimes more tests to rule out other anemia causes.
- Direct Coombs test (Direct Antiglobulin Test) to detect antibodies or complement proteins attached to red blood cells.
- Complete Blood Count (CBC) to assess the severity of anemia.
- Reticulocyte count to evaluate bone marrow response.
- Lactate Dehydrogenase (LDH) levels to assess hemolysis.
Treatment Approaches
Treatment for AIHA varies based on the cause, severity, and type of AIHA.
First-line treatment often includes corticosteroids to reduce red blood cell destruction. Sometimes, immunosuppressive drugs are used to lessen the immune system’s attack on red blood cells.
For those not responding to initial treatments, splenectomy (removal of the spleen) might be considered. The spleen is a key site for red blood cell destruction.
In summary, AIHA is a complex autoimmune disorder needing a personalized approach to diagnosis and treatment. Knowing the differences between warm and cold AIHA, along with the right diagnostic methods and treatments, is key to managing it well.
Immune Thrombocytopenia (ITP)
Understanding immune thrombocytopenia (ITP) means knowing how the immune system can go wrong. ITP happens when the immune system attacks platelets, leading to low counts. This can cause serious bleeding problems.
Pathophysiology of Platelet Destruction
In ITP, the immune system sees platelets as enemies. It makes antibodies to attack them. The spleen is key in this fight, as it removes these marked platelets from the blood.
Platelets are destroyed mainly by antibody-mediated phagocytosis. Macrophages in the spleen and liver eat the antibody-coated platelets. This lowers platelet counts, raising the risk of bleeding.
Clinical Presentation
ITP symptoms vary from person to person. Common signs include:
- Petechiae (small spots on the skin due to bleeding)
- Purpura (larger areas of bruising)
- Nosebleeds or bleeding gums
- Easy bruising
- Heavy menstrual periods in women
Severe cases can lead to life-threatening bleeding, like bleeding in the brain. How bad symptoms are often depends on how low the platelet count is.
Management Strategies
Managing ITP involves several steps to stop platelet destruction and boost production. First, doctors often use:
- Corticosteroids to cut down antibody production and platelet destruction
- Intravenous immunoglobulin (IVIG) to quickly raise platelet counts
If these don’t work, or if the disease is chronic, other treatments might be needed. Thrombopoietin receptor agonists can help by encouraging the bone marrow to make more platelets.
In some cases, splenectomy (spleen removal) is considered. It can greatly reduce platelet destruction. But, this choice is made carefully, weighing the risks and benefits.
Autoimmune Neutropenia
Autoimmune neutropenia is when the immune system attacks neutrophils, a key white blood cell. This makes fighting infections hard. It’s important to know about its types, how to diagnose it, and treatment choices.
Primary vs. Secondary Forms
There are two main types of autoimmune neutropenia: primary and secondary. The primary form happens without any other condition causing it. Secondary autoimmune neutropenia is linked to other diseases, medicines, or conditions.
Primary autoimmune neutropenia often affects children and might go away by itself. Secondary autoimmune neutropenia is more common in adults. It’s tied to autoimmune diseases, infections, or some medicines.
Diagnostic Challenges
Finding out if someone has autoimmune neutropenia can be tough. Symptoms like frequent infections can also show up in other conditions. Doctors use blood tests to check for low neutrophil counts and antibodies against neutrophils.
The tests might include:
- Blood tests to check neutrophil counts
- Tests to find antibodies against neutrophils
- Bone marrow tests in some cases to rule out other neutropenia causes
Treatment Options
Treatment for autoimmune neutropenia depends on how bad it is and why it’s happening. For mild cases, especially in kids, doctors might just watch and wait. Some cases get better on their own.
For more serious cases or when symptoms are bad, treatment might be:
- Corticosteroids to lessen the immune system’s attack on neutrophils
- Intravenous immunoglobulin (IVIG) to help the immune system
- Granulocyte-colony stimulating factor (G-CSF) to make more neutrophils
Autoimmune neutropenia is a complex condition needing a detailed approach for diagnosis and treatment. Knowing its types, how to diagnose it, and treatment options is key to managing it well.
Evans Syndrome and Autoimmune Pancytopenia
Evans syndrome is when the immune system attacks many blood cell types. This leads to severe shortages of blood cells. It’s a rare condition that combines autoimmune hemolytic anemia (AIHA) and immune thrombocytopenia (ITP). Sometimes, it also includes autoimmune neutropenia.
Combined Autoimmune Cytopenias
In Evans syndrome, the immune system mistakenly attacks and destroys red blood cells, platelets, and sometimes white blood cells. This causes combined autoimmune cytopenias. It’s a condition where many cell types are affected.
- Autoimmune hemolytic anemia (AIHA) destroys red blood cells.
- Immune thrombocytopenia (ITP destroys platelets.
- Autoimmune neutropenia reduces neutrophils, a type of white blood cell.
Diagnostic Approach
To diagnose Evans syndrome, doctors check blood cell counts and look for autoantibodies. They use several tests:
- Complete Blood Count (CBC) checks different blood cells.
- Direct Antiglobulin Test (DAT) finds antibodies or proteins on red blood cells.
- Platelet antibody tests diagnose ITP.
These tests confirm the diagnosis by showing autoimmune cytopenias.
Therapeutic Challenges
Managing Evans syndrome is hard because of its complexity and varied treatment responses. Treatment plans often include:
- Corticosteroids as a first treatment to lessen the immune system’s attack.
- Immunosuppressive drugs for harder cases to suppress the immune system more.
- Intravenous Immunoglobulin (IVIG) to temporarily boost platelet counts and reduce red blood cell destruction.
In some cases, splenectomy might be considered to lower blood cell destruction. But, this choice depends on the patient’s situation, weighing risks and benefits.
Rare Autoimmune Blood Conditions
There are rare autoimmune blood conditions that need special care. These conditions are not as common but have a big impact on people’s lives. We will look at three of these: Pure Red Cell Aplasia, Autoimmune Lymphoproliferative Syndrome, and Paroxysmal Cold Hemoglobinuria.
Pure Red Cell Aplasia
Pure Red Cell Aplasia (PRCA) is when the bone marrow can’t make enough red blood cells. It can happen for many reasons, like medicines or infections. Doctors use bone marrow biopsies and blood tests to find out why.
To treat PRCA, doctors first try to find and fix the cause. If they can’t find the cause, they might use immunosuppressive therapy. This helps stop the immune system from attacking red blood cells.
Autoimmune Lymphoproliferative Syndrome
Autoimmune Lymphoproliferative Syndrome (ALPS) is a rare genetic disorder. It causes too many lymphocytes, leading to autoimmune problems and a higher risk of lymphoma. It often starts in childhood.
Doctors treat ALPS with a team effort. They use immunosuppressive drugs to control the immune system. Sometimes, they also use targeted therapies to manage the growth of lymphocytes.
Paroxysmal Cold Hemoglobinuria
Paroxysmal Cold Hemoglobinuria (PCH) is a rare condition where cold-reacting antibodies destroy red blood cells. It can be caused by infections or happen on its own.
To diagnose PCH, doctors do the Donath-Landsteiner test. This test finds the cold-reacting antibodies. Treatment includes staying warm and, in serious cases, immunosuppressive therapy or rituximab to lower antibody levels.
These rare conditions show how complex and varied autoimmune disorders can be. Knowing about them is key to helping patients get the right care and support.
Pediatric Autoimmune Blood Disorders
When a child is diagnosed with an autoimmune blood disorder, it’s a tough time for families. They need support and guidance. These conditions need a detailed treatment plan, made just for kids.
Unique Considerations in Children
Autoimmune blood disorders in kids are different from those in adults. Their immune systems are still growing. This means we have to think about how these conditions might affect their health for years to come.
We must also consider the child’s growth, the side effects of treatments, and how it affects the whole family. This is important for their well-being.
Specialized care is key to managing these conditions well. We need to keep a close eye on the child’s health. We also adjust treatments as needed and support the family through tough times.
Long-term Prognosis
The future looks different for each child with an autoimmune blood disorder. It depends on the condition, how severe it is, and how well it responds to treatment. Thanks to medical progress, many kids can live active lives.
But, they still need ongoing care. This includes regular check-ups and adjusting treatments to keep them healthy.
We help families understand their child’s future. This way, they can make informed decisions about their care.
Family Support Strategies
Supporting families is crucial when a child has an autoimmune blood disorder. We offer emotional support, educational resources, and connect them with others facing similar challenges. This builds a supportive community.
We also teach family members about the condition and how to manage it. This helps them be more involved in their child’s care. It also lets them know when to seek help.
By combining top-notch medical care with strong family support, we can make a big difference. We aim to improve the lives of kids with autoimmune blood disorders.
Diagnostic Approaches for Autoimmune Blood Diseases
Diagnosing autoimmune blood diseases needs a mix of tests and evaluations. We’ll look at the tools and methods used to spot and treat these conditions well.
Laboratory Testing
Laboratory tests are key in diagnosing autoimmune blood diseases. We run various tests to check for these conditions and how severe they are.
- Complete Blood Count (CBC): A CBC is often the first test for autoimmune blood disorders. It shows the types of blood cells.
- Direct Antiglobulin Test (DAT): Also known as the Coombs test, DAT finds antibodies or complement proteins on red blood cells. This helps diagnose autoimmune hemolytic anemia.
- Antibody Screening: Tests like the indirect antiglobulin test (IAT) find antibodies against red blood cells, platelets, or neutrophils.
Imaging Studies
Imaging studies also help in diagnosing. They let us check the spleen’s size and find any issues linked to autoimmune blood diseases.
- Ultrasound: This non-invasive imaging checks spleen size and finds any problems.
- Computed Tomography (CT) Scan: A CT scan gives detailed spleen and organ images. It helps in assessing autoimmune blood disorders.
Bone Marrow Evaluation
Bone marrow evaluation is vital, especially when other tests don’t give clear results. We look at the bone marrow to see how blood cells are made and mature.
- Bone Marrow Aspiration: This procedure takes a bone marrow sample for examination. It helps diagnose conditions like autoimmune neutropenia or pancytopenia.
- Bone Marrow Biopsy: A biopsy gives a detailed look at the bone marrow’s structure and cell makeup. It aids in diagnosing various autoimmune blood diseases.
By using lab tests, imaging, and bone marrow evaluation together, we can accurately diagnose and manage autoimmune blood diseases. This improves patient outcomes.
Conventional Treatment Strategies
For autoimmune blood disorders, treatments often mix medicines and sometimes surgery. We’ll look at these options, their uses, benefits, and possible downsides.
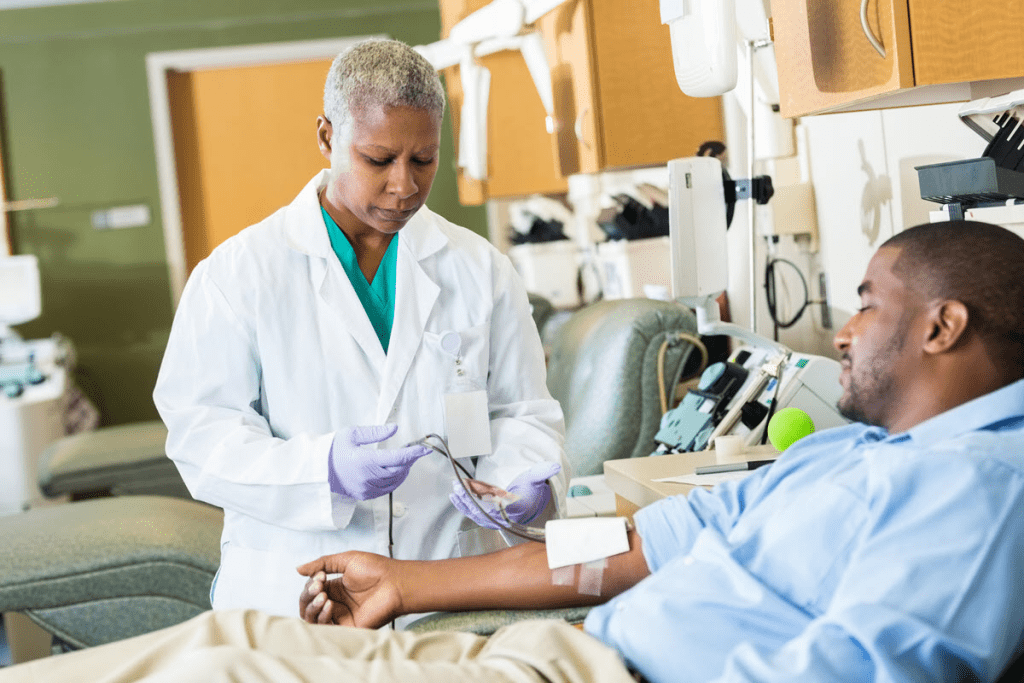
Corticosteroids and Immunosuppressants
Corticosteroids are a first choice for treating these disorders. They cut down inflammation and calm the immune system. Prednisone is a common corticosteroid used for conditions like autoimmune hemolytic anemia (AIHA) and immune thrombocytopenia (ITP).
Immunosuppressants are also key. They stop the immune system from attacking blood cells too much. We often pair them with corticosteroids for better results.
| Treatment | Indications | Benefits | Potential Side Effects |
| Corticosteroids | AIHA, ITP, other autoimmune blood disorders | Reduce inflammation, suppress immune system | Weight gain, mood changes, increased risk of infections |
| Immunosuppressants | AIHA, ITP, other autoimmune blood disorders | Suppress immune system, reduce blood cell destruction | Increased risk of infections, potential organ damage |
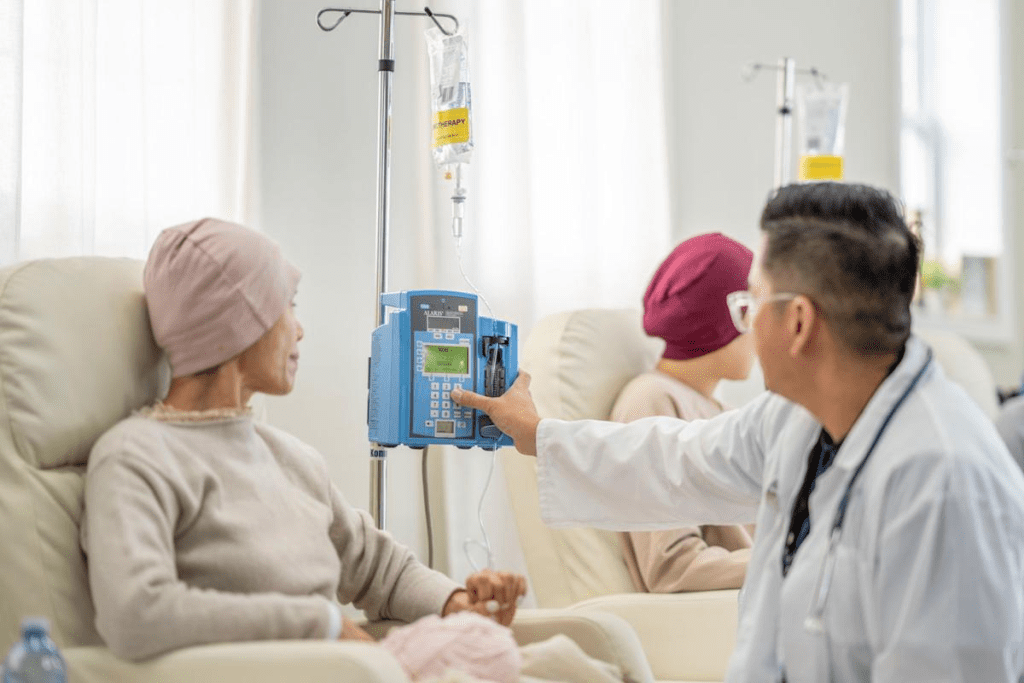
Intravenous Immunoglobulin (IVIG)
IVIG comes from donor plasma and is given through a vein. It’s used for ITP and AIHA, especially when other treatments don’t work.
IVIG helps by controlling the immune system. This reduces damage to platelets or red blood cells. It’s fast-acting and lowers the risk of bleeding.
Splenectomy Considerations
Splenectomy is an option for some autoimmune blood disorders, like ITP. It’s considered when other treatments don’t work well or when bleeding is severe.
Removing the spleen can lead to lasting improvement. But, it also comes with risks like infection and blood clots.
In summary, treating autoimmune blood disorders involves various methods. These include medicines like corticosteroids and immunosuppressants, and sometimes surgery. We choose the best treatment for each patient based on their condition and how they respond to treatment.
Emerging Therapies and Research Directions
New treatments are changing how we handle autoimmune blood disorders. Medical research has brought us new ways to treat these complex conditions. This gives patients new hope.
Targeted Biologics
Targeted biologics are a big step forward in treating autoimmune blood disorders. They aim at specific parts of the immune system. This helps avoid weakening the immune system too much.
- Rituximab: A monoclonal antibody that targets CD20-positive B cells, which are often implicated in autoimmune blood disorders.
- Other biologics: Such as belimumab and eculizumab, which target different aspects of the immune response.
These targeted therapies are showing great promise in trials. They are becoming more common in treating patients.
CAR-T Cell Therapy
CAR-T cell therapy is a new way to treat diseases. It changes a patient’s T cells to fight specific cells causing the disease.
Benefits include:
- Potential for long-term remission
- Targeted approach reducing harm to healthy cells
But, CAR-T cell therapy also has challenges. It can cause cytokine release syndrome and neurotoxicity.
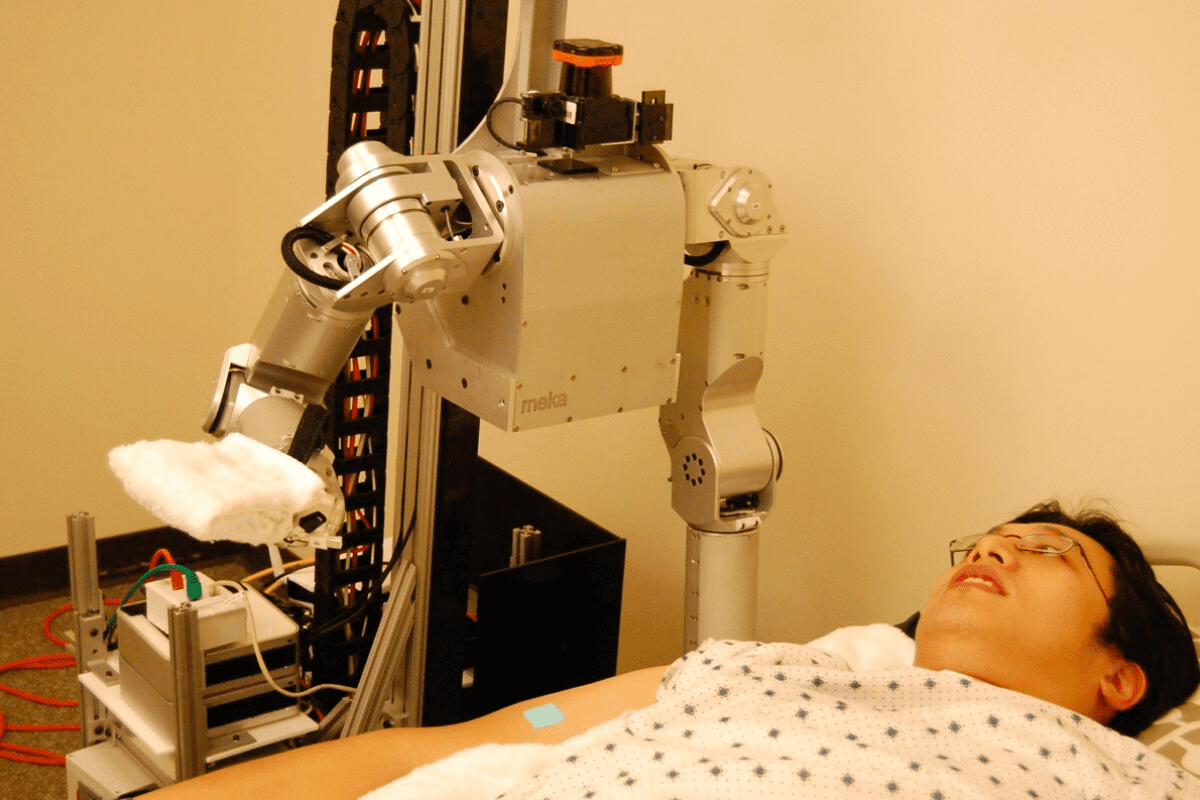
Stem Cell Transplantation
Stem cell transplantation is being looked at for severe autoimmune blood disorders. This includes hematopoietic stem cell transplantation (HSCT).
Autologous HSCT, where a patient’s own stem cells are used, is showing promise. It can lead to long-term remissions for some patients.
Using stem cell transplantation is a big decision. It needs careful thought about risks and benefits. More research is needed to make it better.
Living with Autoimmune Blood Disorders
Living with autoimmune blood disorders is more than just treatment. It’s about managing symptoms and improving life quality. We know it’s tough, but with the right strategies and support, you can live a fulfilling life.
Managing Flare-ups and Remissions
Managing flare-ups and remissions is key. Flare-ups can be unpredictable, so being ready is important. Keeping a symptom journal helps track when flare-ups happen and what might cause them. This info is crucial for adjusting treatment plans.
During a flare-up, follow your healthcare provider’s treatment plan. This might mean changing medications or adjusting your lifestyle. Eating well and exercising regularly can also help manage symptoms.
Quality of Life Considerations
Quality of life is a big concern for those with autoimmune blood disorders. It’s important to stay connected with loved ones and do things that make you happy. Stress-reduction activities like meditation or yoga can also help.
Staying informed about your condition and treatment options is vital. Don’t hesitate to ask questions or seek a second opinion. Being involved in your care can greatly improve your life quality.
Psychological Impact and Support Resources
The psychological effects of autoimmune blood disorders are real. Chronic illness can cause feelings of isolation, anxiety, and depression. Seeking help from mental health professionals, support groups, and online communities is crucial.
There are many support resources for those affected by autoimmune blood disorders. Look into counseling services, patient advocacy groups, and educational materials. Connecting with others who face similar challenges can be incredibly helpful.
In conclusion, managing autoimmune blood disorders requires a comprehensive approach. This includes managing flare-ups, improving life quality, and addressing mental health. By using available support resources and staying informed, you can overcome these challenges and enhance your well-being.
FAQ
What are autoimmune blood disorders?
Autoimmune blood disorders happen when the immune system attacks healthy blood cells. This leads to different health problems.
What is the difference between warm and cold AIHA?
Warm AIHA happens when antibodies attack red blood cells at body temperature. Cold AIHA occurs when antibodies attack at cold temperatures, below 32 °C (90 °F).
What is immune thrombocytopenia (ITP)?
ITP is an autoimmune condition. It happens when the immune system attacks platelets, causing low counts. This can lead to serious bleeding.
What is autoimmune neutropenia?
Autoimmune neutropenia is when the immune system destroys neutrophils. This makes it hard for the body to fight infections.
What is Evans syndrome?
Evans syndrome is a rare disorder. It combines autoimmune hemolytic anemia and thrombocytopenia, often with other cytopenias.
How are autoimmune blood disorders diagnosed?
Doctors use lab tests like complete blood counts and direct Coombs tests. They also do bone marrow biopsies and imaging studies to see how much blood cells are being destroyed.
What are the treatment options for autoimmune hemolytic anemia?
Treatments include corticosteroids and immunosuppressive medications. Some patients also get intravenous immunoglobulin (IVIG). In severe cases, removing the spleen may be needed.
Can autoimmune blood disorders be cured?
Some patients can go into long-term remission. But, autoimmune blood disorders are often chronic. They need ongoing treatment and management.
What is the role of splenectomy in treating autoimmune blood disorders?
Removing the spleen can help treat ITP and AIHA. It reduces the destruction of blood cells.
Are there new treatments on the horizon for autoimmune blood disorders?
Yes, new treatments are coming. They include targeted biologics, CAR-T cell therapy, and stem cell transplantation. These offer new hope for patients.
How can patients manage flare-ups and remissions?
Managing flare-ups and remissions requires sticking to medication and making lifestyle changes. Regular check-ups with healthcare providers help adjust treatment plans.
What support resources are available for patients with autoimmune blood disorders?
Patients can find support through patient groups, online forums, and counseling services. These help manage the emotional impact and improve life quality.
How do autoimmune blood disorders affect children differently than adults?
Children face unique challenges, like growth and development issues. They need special care and support from families and healthcare providers.
What is pure red cell aplasia?
Pure red cell aplasia is a rare condition. The bone marrow fails to make red blood cells, often due to an autoimmune response. Specific treatments are needed to help make red blood cells.
References
- Osborn, J. J., et al. (2025). Prevalence and incidence of primary autoimmune hemolytic anemia in the United States: A multi-database retrospective analysis. PLOS ONE, 20(6), e1234567. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12200825/