Last Updated on October 21, 2025 by mcelik
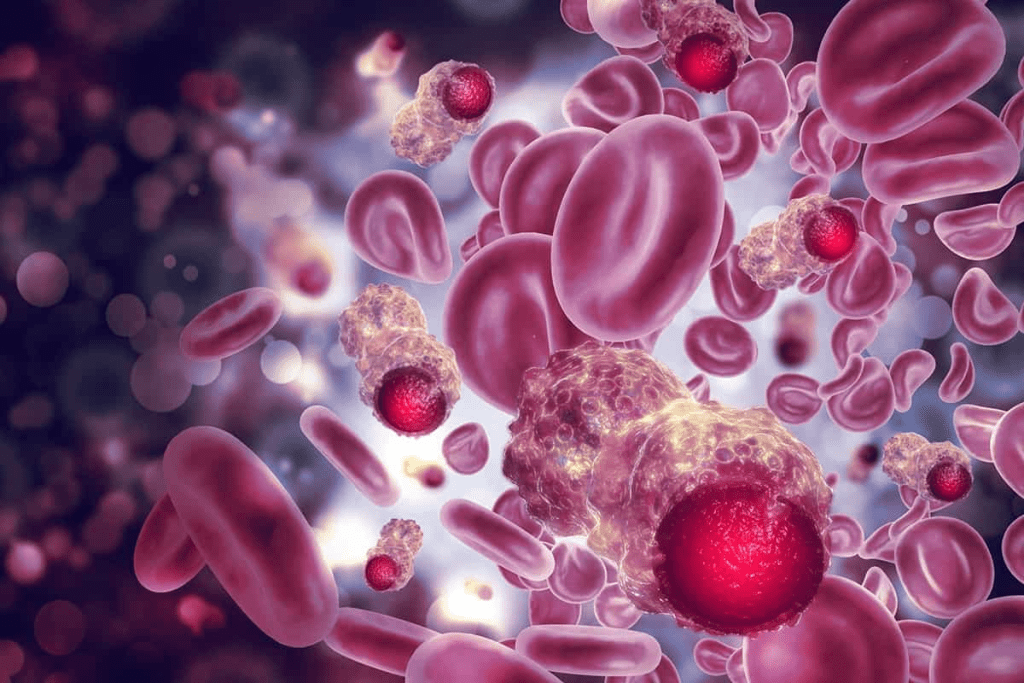
Hematologic cancers, also known as hematologic malignancies, affect the blood, bone marrow, and lymph nodes. These cancers are diverse, with types including leukemia, lymphoma, and multiple myeloma.
Leukemia is considered the most common form of hematologic cancer. According to recent medical research, it accounts for a significant portion of hematologic malignancy diagnoses.
Understanding the different types of blood cancer is key for diagnosis and treatment. We will dive deeper into these, sharing insights into their characteristics and impacts.
Key Takeaways
- Hematologic cancers include leukemia, lymphoma, and multiple myeloma.
- Leukemia is often the most common form of hematologic cancer.
- These cancers affect the blood, bone marrow, and lymph nodes.
- Understanding the types of hematologic cancers is key for effective treatment.
- Recent medical research provides valuable insights into these malignancies.
Understanding Hematologic Malignancies
Hematologic malignancies are a group of cancers that affect the blood, bone marrow, and lymph nodes. These cancers happen when abnormal cells grow out of control in the body’s blood-making tissues.
Definition and Basic Concepts
Blood cancers, or hematologic malignancies, start with a DNA mutation in blood cell-making cells. This mutation causes the growth of bad cells. These cells fill up the bone marrow and stop it from making normal blood cells.
There are different types of blood cancers, like leukemia, lymphoma, and multiple myeloma. Each type affects the blood and immune system in its own way.
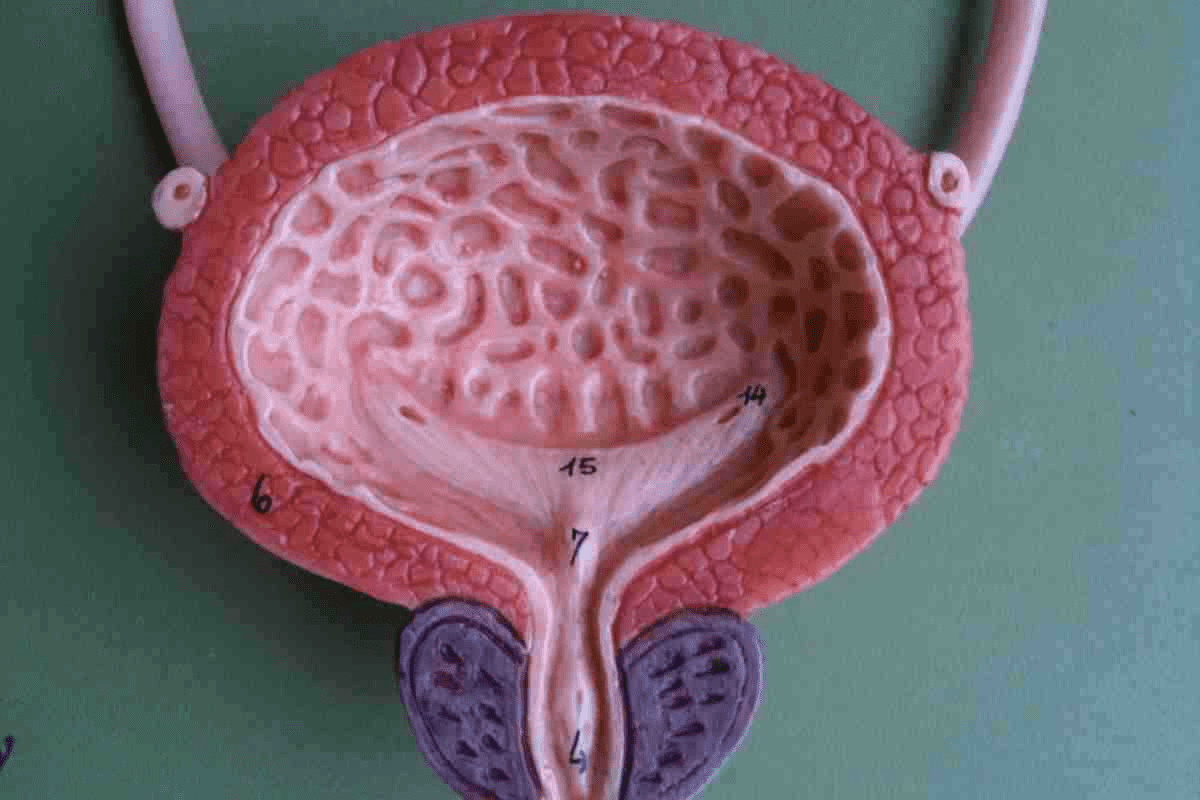
The Blood and Bone Marrow System
The blood and bone marrow system is key for making blood cells. These include red blood cells, white blood cells, and platelets. The bone marrow, a soft tissue inside bones, is where these cells are made.
It’s important to know how blood cancers affect the blood and bone marrow. This helps us understand how these cancers grow and their effects on the body.
| Type of Blood Cancer | Description | Affected Cells/Tissues |
| Leukemia | Cancer of the blood and bone marrow | Blood cells, bone marrow |
| Lymphoma | Cancer of the lymphatic system | Lymphocytes, lymph nodes |
| Multiple Myeloma | Cancer of plasma cells in the bone marrow | Plasma cells, bone marrow |
Knowing the basics of blood cancers helps us understand their complexity. It shows why finding the right diagnosis and treatment is so important.
Types of Blood Cancers and Their Prevalence
Leukemia, lymphoma, and multiple myeloma are the main blood cancers. Each has its own traits and how common it is. These cancers affect millions worldwide, impacting public health a lot.
Major Categories of Hematologic Cancers
Hematologic cancers are mainly leukemia, lymphoma, and multiple myeloma. Leukemia is a blood and bone marrow cancer with too many white blood cells. Lymphoma starts in the lymphatic system, part of our immune system. Multiple myeloma is a cancer of plasma cells in the bone marrow.
These three types make up most hematologic malignancies. Knowing the type of blood cancer is key for the right treatment and outlook.
| Type of Blood Cancer | Characteristics | Prevalence |
| Leukemia | Cancer of blood and bone marrow | High |
| Lymphoma | Cancer of the lymphatic system | High |
| Multiple Myeloma | Cancer of plasma cells in bone marrow | Moderate |
Global vs. U.S. Prevalence Patterns
The occurrence of blood cancers changes a lot around the world. It depends on age, genetics, and what we’re exposed to.
In the U.S., leukemia, lymphoma, and multiple myeloma are among the top cancers. The American Cancer Society keeps track of these cancers’ numbers.
“The incidence of hematologic malignancies has been steadily increasing over the past few decades, highlighting the need for continued research and improved treatment options.”
NCCN Guidelines
Looking at global and U.S. patterns shows some trends. For example, some lymphomas are more common in developed countries. Certain leukemias are more common in other areas.
It’s important for doctors and researchers to understand these patterns. This helps them create better treatments and improve patient care.
Leukemia: The Most Common Form of Blood Cancer
Leukemia is a cancer that affects the blood and bone marrow. It’s the most common blood cancer. It happens when blood cells grow too much, causing health problems. We’ll look at the different types of leukemia, their traits, and how they affect people.
Acute Myeloid Leukemia (AML)
Acute Myeloid Leukemia (AML) is a fast-growing leukemia. It starts in the bone marrow and can spread to the blood and other parts of the body. AML is more common in adults than in children and is very aggressive.
Symptoms of AML include feeling very tired, having fevers, and getting sick easily. You might also bruise or bleed easily. Doctors use bone marrow biopsies and blood tests to diagnose it.
Chronic Lymphocytic Leukemia (CLL)
Chronic Lymphocytic Leukemia (CLL) is a slow-growing leukemia. It’s more common in older adults. CLL is known for the gradual buildup of mature lymphocytes in the blood, bone marrow, and lymphoid tissues.
CLL symptoms include swollen lymph nodes, feeling very tired, and losing weight. Some people may not show symptoms for years. Doctors often find CLL during routine blood tests.
Other Leukemia Types
There are other types of leukemia too. Acute Lymphoblastic Leukemia (ALL) is more common in children and involves the quick production of immature lymphocytes. Chronic Myeloid Leukemia (CML) is known for the uncontrolled growth of myeloid cells and is often linked to a specific genetic abnormality.
| Type of Leukemia | Characteristics | Common Symptoms |
| Acute Myeloid Leukemia (AML) | Aggressive, rapid progression | Fatigue, fever, infections, easy bruising |
| Chronic Lymphocytic Leukemia (CLL) | Slow progression, accumulation of mature lymphocytes | Swollen lymph nodes, fatigue, weight loss |
| Acute Lymphoblastic Leukemia (ALL) | Rapid production of immature lymphocytes | Fever, fatigue, bone pain |
| Chronic Myeloid Leukemia (CML) | Uncontrolled growth of myeloid cells | Fatigue, weight loss, abdominal pain |
Leukemia includes many diseases, each with its own challenges. Knowing these differences is key for the right diagnosis and treatment.
“The diagnosis and treatment of leukemia have evolved significantly over the years, bringing new hope to patients worldwide.”
” Hematologist
Chronic Lymphocytic Leukemia: America’s Most Prevalent Blood Cancer
CLL is a cancer that affects the blood and bone marrow. It causes too many immature white blood cells. This problem is more common in older adults and is a big focus in research.
Pathophysiology
CLL happens when there’s too much of a certain type of lymphocyte. These cells can’t fight off infections well. They build up in the blood, bone marrow, and lymph nodes, causing problems.
It’s important to understand CLL’s genetic and molecular causes. This helps in finding new treatments.
Risk Factors and Demographics
Several factors increase the risk of CLL. These include age, family history, and certain genetic changes.
Most CLL cases are found in people over 60. The risk goes up with age.
Men are more likely to get CLL than women. People of European descent also have a higher risk.
Staging and Classification
Doctors use the Rai or Binet systems to stage CLL. These systems help predict how the disease will progress and decide on treatment.
The Rai system has five stages (0 to IV). The Binet system has three stages (A to C).
| Rai Stage | Binet Stage | Description |
| 0 | A | Lymphocytosis in blood and marrow |
| I | A | Lymphocytosis with lymphadenopathy |
| II | B | Lymphocytosis with hepatomegaly or splenomegaly |
| III | C | Lymphocytosis with anemia |
| IV | C | Lymphocytosis with thrombocytopenia |
Non-Hodgkin Lymphoma: A Close Second
Non-Hodgkin lymphoma (NHL) is a big group of lymphoid cancers. It’s different from Hodgkin lymphoma because it doesn’t have Reed-Sternberg cells. NHL can start from either B cells or T cells, but B-cell lymphomas are more common.
B-Cell vs. T-Cell Lymphomas
B-cell lymphomas come from B lymphocytes and are more common. They include types like DLBCL and follicular lymphoma. T-cell lymphomas, which start from T lymphocytes, are less common. They are often more aggressive and harder to treat.
| Lymphoma Type | Origin | Prevalence |
| B-Cell Lymphoma | B Lymphocytes | More Common |
| T-Cell Lymphoma | T Lymphocytes | Less Common |
Diffuse Large B-Cell Lymphoma (DLBCL)
DLBCL is a fast-growing type of NHL but can be cured with quick treatment. It’s made up of large B cells. Studies show that DLBCL makes up a big part of NHL cases.
“The aggressive nature of DLBCL necessitates immediate diagnosis and treatment. Advances in chemotherapy and targeted therapies have improved outcomes for many patients.”
Expert Opinion
Follicular Lymphoma and Other Subtypes
Follicular lymphoma is usually slow-growing and has a better outlook. Other types include marginal zone lymphoma and mantle cell lymphoma. Each has its own traits and treatment plans.
Knowing the exact type of NHL is key to finding the best treatment. Ongoing research brings new hope for those with these complex cancers.
Multiple Myeloma: Understanding Plasma Cell Cancer
Learning about multiple myeloma means exploring its causes and effects on patients. It’s a cancer that affects plasma cells, a key white blood cell in the bone marrow. These cancerous cells take over the bone marrow, pushing out healthy cells.
Pathophysiology and Progression
The disease’s workings involve a battle between cancerous plasma cells and the bone marrow. Malignant plasma cells make substances that help them grow and multiply. This battle harms bones, leads to anemia, and weakens the immune system.
How fast multiple myeloma grows can differ a lot between people. Some may see it grow slowly, while others face a quicker, more aggressive disease. Knowing what affects how fast it grows is key to finding the right treatment.
Diagnostic Criteria and Staging
Doctors use several methods to diagnose multiple myeloma. They look for diagnostic criteria like M-protein in blood or urine, the number of plasma cells in the bone marrow, and signs of damage to organs.
- Monoclonal protein (M-protein) detection
- Bone marrow biopsy to assess plasma cell percentage
- Imaging studies (e.g., PET/CT, MRI) to evaluate bone lesions
- Laboratory tests to assess kidney function and calcium levels
The staging of multiple myeloma uses the Revised International Staging System (R-ISS). It considers serum albumin, beta-2 microglobulin, lactate dehydrogenase (LDH), and chromosomal changes to sort patients into risk groups.
- Stage I: Low risk
- Stage II: Intermediate risk
- Stage III: High risk
Getting the staging right is vital for knowing what to expect and planning treatment. By grasping the disease’s nature, diagnosis, and staging, doctors can tailor treatments to help patients better.
Blood Cancers in the Elderly Population
As people get older, the chance of getting blood cancers like leukemia and lymphoma goes up a lot. This means we need to understand how these diseases affect older people more.
Age-Related Risk Factors
The risk of getting leukemia and lymphoma grows with age. Older adults face a higher risk because of their genes and the environment.
Changes in the immune system with age also play a role. This makes older people more likely to get blood cancers.
Treatment Considerations for Older Patients

Dealing with blood cancers in older patients is tough. They often have other health issues that make treatment harder.
When choosing a treatment, we must think about the patient’s health and what they can handle. Personalized medicine is key. It considers the patient’s health, wishes, and how well they can handle strong treatments.
Treatment for older patients might include special chemotherapy, targeted therapies, and care to help with symptoms. This helps improve their quality of life.
Recognizing the Symptoms of Blood Cancers
It’s important to know the symptoms of blood cancers like leukemia, lymphoma, and myeloma. These cancers can show similar signs as other diseases. This makes it hard to spot them early.
Common Warning Signs Across Blood Cancers
There are some symptoms that are common in blood cancers. These include:
- Unexplained weight loss: Losing weight without a clear reason can be a sign of an underlying health issue, including blood cancers.
- Fatigue: Persistent tiredness or weakness that doesn’t improve with rest is a common symptom.
- Recurrent infections: Blood cancers can weaken the immune system, leading to frequent infections.
- Bone pain or tenderness: Pain or tenderness in the bones or joints can occur, specially in leukemia or myeloma.
Leukemia-Specific Symptoms
Leukemia, a cancer of the blood and bone marrow, has its own symptoms. These include:
- Bleeding or bruising easily: Leukemia can affect the production of platelets, leading to easy bruising or bleeding.
- Pale skin: A decrease in red blood cells can cause paleness.
- Swollen lymph nodes: Enlarged lymph nodes can be a sign of leukemia.
Lymphoma and Myeloma Symptoms
Lymphoma and myeloma have their own symptoms. For lymphoma, these include:
- Swollen lymph nodes: Enlarged lymph nodes are a hallmark symptom of lymphoma.
- Fever and night sweats: Recurring fevers and night sweats can occur.
Myeloma symptoms include:
- Bone pain: Pain in the back, ribs, or hips is common due to bone damage.
- Hypercalcemia: High levels of calcium in the blood can lead to symptoms like confusion, weakness, and constipation.
Spotting these symptoms early can greatly improve treatment and outcomes. If you notice any of these signs, see a doctor right away.
Diagnostic Approaches for Hematologic Malignancies
We use many ways to find and understand hematologic malignancies. These methods mix old lab tests with new molecular techniques. This mix is key to diagnosing these complex diseases.
Complete Blood Count and Blood Smear Analysis
A Complete Blood Count (CBC) is often the first step. It checks the blood’s different parts, like red and white cells, and platelets. If the CBC shows odd results, it might mean a hematologic malignancy is present.
Blood smear analysis is also very important. It looks at blood under a microscope for abnormal cells. This test is key for spotting leukemia and lymphoma.
Bone Marrow Biopsy and Aspiration
Bone marrow biopsy and aspiration are vital for diagnosing and understanding hematologic malignancies. These tests take a bone marrow sample for study. The biopsy looks at the bone marrow’s structure, while aspiration checks the cells.
These tests are key for diagnosing diseases like multiple myeloma and some leukemias. They help figure out how far the disease has spread and guide treatment.
Advanced Molecular and Genetic Testing
Advanced molecular and genetic tests are very important for diagnosing and managing hematologic malignancies. Tests like PCR and NGS find specific genetic changes linked to blood cancers.
These tests help sort out different types of blood cancers, guess how the disease will progress, and find treatment targets. They’re essential for making treatment plans that fit each patient’s needs.
| Diagnostic Test | Purpose | Information Provided |
| Complete Blood Count (CBC) | Initial screening for hematologic malignancies | Overview of blood components, including red and white blood cells and platelets |
| Blood Smear Analysis | Identify abnormal cells | Microscopic examination of blood cells to diagnose leukemia and lymphoma |
| Bone Marrow Biopsy and Aspiration | Diagnose and stage hematologic malignancies | Information about bone marrow structure and cell composition |
| Advanced Molecular and Genetic Testing | Detect genetic mutations, subclassify malignancies, and predict prognosis | Identification of specific genetic abnormalities associated with blood cancers |
Treatment Modalities for Blood Cancers
Understanding the different treatment options is key to managing blood cancers well. The field of treating blood cancers has grown a lot. Now, there are many treatments that fit each patient’s needs.
Chemotherapy Regimens
Chemotherapy is a mainstay in treating blood cancers. Chemotherapy regimens change based on the cancer type, its stage, and the patient’s health. For example, acute myeloid leukemia (AML) often needs strong chemotherapy.
Common chemotherapy agents include:
- Cytarabine
- Anthracyclines
- Fludarabine
These drugs can be used alone or together. The right regimen depends on the diagnosis and the patient’s health.
Targeted Therapies and Immunotherapies
Targeted therapies have changed the game in treating blood cancers. They focus on specific molecular targets. For instance, tyrosine kinase inhibitors (TKIs) are used in chronic myeloid leukemia (CML) to target the BCR-ABL fusion protein.
Immunotherapies, like monoclonal antibodies and CAR-T cell therapy, are also promising. CAR-T cell therapy modifies a patient’s T cells to attack cancer cells. This offers new hope for patients with hard-to-treat diseases.
| Therapy Type | Examples | Indications |
| Targeted Therapy | Imatinib, Dasatinib | CML, Ph+ ALL |
| Immunotherapy | Rituximab, CAR-T cell therapy | Non-Hodgkin Lymphoma, CLL |
Stem Cell Transplantation
Stem cell transplantation is a key treatment for blood cancers. It includes both autologous and allogeneic transplants. Allogeneic stem cell transplantation replaces a patient’s bone marrow with a donor’s. This can cure some blood cancers.
Choosing stem cell transplantation depends on many factors. These include the patient’s age, health, and the disease’s specifics.
We’re seeing a big change in treating blood cancers. There’s a move towards more personalized and targeted treatments. As research keeps improving, we’ll see even more new treatments.
Prognosis and Survival Rates by Cancer Type
Prognosis and survival rates for blood cancer patients depend on many factors. These include the type of cancer, the patient’s age, and how well they respond to treatment. Knowing these factors is key for both patients and doctors to make the best treatment plans.
Factors Affecting Blood Cancer Outcomes
Several key factors affect blood cancer patients’ prognosis. Age is a big factor, as older patients may face more challenges. The overall health of the patient, including other medical conditions, also matters a lot. How well a patient responds to initial treatment is another strong indicator of survival.
Advances in genetic and molecular profiling have helped predict outcomes better. The type of blood cancer is also very important. For example, Chronic Lymphocytic Leukemia (CLL) usually has a better prognosis than Acute Myeloid Leukemia (AML), which is more common in older adults. The stage at diagnosis also greatly affects prognosis, with earlier stages leading to better outcomes.
Five-Year Survival Statistics
Five-year survival rates give a general idea of prognosis for different blood cancers. Recent data shows an improvement in overall five-year survival rates for blood cancers. For instance, CLL often has a high five-year survival rate, around 85-90% in many areas. On the other hand, AML has a more varied prognosis, influenced by age and genetic characteristics.
It’s important to remember that survival statistics are averages and may not apply to every individual. New treatments, like targeted therapies and immunotherapies, are helping improve survival rates for many blood cancers.
As medical research advances, we see better prognosis and survival rates for blood cancer patients. Understanding the factors that influence outcomes helps patients and doctors work together to improve treatment plans.
Living with Hematologic Cancer
Living with hematologic cancer means tackling it from all angles. This includes managing side effects and finding support. It’s a journey that touches every part of a person’s life, from physical health to emotional well-being.
Managing Treatment Side Effects
Handling treatment side effects is key to a better life for those with hematologic cancer. These effects can change a lot based on the cancer type, treatment, and the person’s health.
Common side effects include:
- Fatigue and weakness
- Nausea and vomiting
- Hair loss
- Increased risk of infections
We suggest patients team up with their doctors to create a plan for these side effects. This might involve medicines, changes in lifestyle, or other therapies.
Psychological and Social Support Resources
Dealing with hematologic cancer also means getting the right emotional and social support. The emotional toll of a cancer diagnosis is huge. Having a strong support network is essential for dealing with it.
Support can come in many forms:
- Professional counseling or therapy
- Support groups, either in-person or online
- Family and friends
- Online resources and educational materials
We urge patients to look into these options to find what suits them best. Talking to others who face similar challenges can be very helpful.
By looking at both the medical and emotional sides of care, we aim to offer full support for those with hematologic cancer. It’s about making a care plan that covers the whole person, not just the disease.
Advances in Blood Cancer Research
The world of blood cancer research is changing fast. New discoveries are being made all the time. Thanks to medical research and technology, we now understand and treat blood cancers differently.
Recent Breakthroughs in Treatment
Recently, we’ve seen big changes in how we treat blood cancers. Targeted therapies and immunotherapies have made a huge impact. For example, CAR-T cell therapy has been very effective against some types of leukemia and lymphoma.
- Targeted Therapies: Drugs that target specific molecules involved in the growth and survival of cancer cells.
- Immunotherapies: Treatments that harness the power of the immune system to fight cancer.
- Precision Medicine: An approach that tailors treatment to the individual characteristics of each patient’s cancer.
Promising Clinical Trials and Future Directions
Clinical trials are leading to exciting new treatments for blood cancers. We’re seeing great results from studies on new agents and combination therapies.
- Investigating the bispecific antibodies in treating blood cancers.
- Exploring gene editing technologies like CRISPR/Cas9 in cancer therapy.
- Developing more effective combination regimens that pair novel agents with existing treatments.
Conclusion
Blood cancers are complex and varied diseases. Our summary shows how common leukemia, lymphoma, and multiple myeloma are. It’s key to know about them early.
It’s important to understand the different blood cancers, their signs, and how doctors diagnose them. We’ve seen how new research and treatments are helping patients.
More research and support are needed to tackle blood cancer challenges. By learning more about these diseases, we can improve care and survival rates.
Our talk highlights the need for complete care and ongoing research into blood cancers. This will help those living with these conditions.
FAQ
What is hematologic cancer?
Hematologic cancer affects the blood, bone marrow, or lymphatic system. It includes leukemia, lymphoma, and multiple myeloma.
What are the main types of blood cancers?
Blood cancers are mainly leukemia, lymphoma, and multiple myeloma. Each affects different parts of the blood and bone marrow system.
Why is leukemia considered the most common blood cancer?
Leukemia is the most common blood cancer. It affects the blood cells and is common in certain age groups.
What is the difference between acute and chronic leukemia?
Acute leukemia needs quick treatment because it grows fast. Chronic leukemia grows slower and may not show symptoms for years.
What are the symptoms of blood cancers?
Symptoms include fatigue, weight loss, and frequent infections. Swollen lymph nodes and bleeding easily are also signs. Symptoms vary by cancer type.
How are blood cancers diagnosed?
Diagnosing blood cancers involves CBC tests, bone marrow biopsies, and imaging studies. Advanced tests also help identify the cancer type and stage.
What are the treatment options for blood cancers?
Treatments include chemotherapy, targeted therapies, and stem cell transplantation. The choice depends on the cancer type, stage, and the patient’s health.
How do age-related risk factors affect blood cancer development?
Age is a big risk factor for blood cancers. The risk grows with age, with older adults more likely to get certain cancers.
What is the prognosis for patients with blood cancers?
Prognosis varies by cancer type, stage, and treatment response. Five-year survival rates give a general idea, but outcomes can vary.
How can patients manage treatment side effects?
Managing side effects involves medical help, lifestyle changes, and support from healthcare providers. Resources for psychological and social support are also available.
What are the latest advances in blood cancer research?
Recent research has led to new treatments like targeted therapies and immunotherapies. Ongoing trials aim to improve treatment and patient outcomes.
Why is awareness and early detection of blood cancers important?
Awareness and early detection are key to better treatment outcomes. Recognizing symptoms and seeking medical help quickly can lead to earlier and more effective treatment.
References
National Cancer Institute (NCI). (2025). Global Burden and Trends of Hematologic Malignancies.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12273037
Provides global trends indicating non-Hodgkin lymphoma has the highest incidence globally among blood cancers, with leukemia having the highest mortality.