
HSC transplantation: Learn the process, success rates, and when this crucial blood treatment is recommended for conditions like cancer.
Modern medicine is moving forward with stem cell transplant procedures. These have shown great promise in fighting blood cancers and other diseases.
HSCT, or bone marrow transplant, replaces damaged bone marrow with healthy stem cells and offers hope for patients with serious diseases.
Key Takeaways
- Hematopoietic stem cell transplantation is a medical treatment that replaces diseased or damaged bone marrow with healthy stem cells.
- HSCT is used to treat various conditions, including blood cancers and certain genetic disorders.
- The procedure involves using stem cells to restore the patient’s bone marrow.
- Bone marrow transplant is another term used to describe HSCT.
- Stem cell transplant procedures have shown promising results in modern medicine.
The Fundamentals of Hematopoietic Treatment
It’s important to understand the basics of hematopoietic treatment. This is key to seeing its value in medicine. Hematopoietic stem cell transplantation (HSCT) is a major treatment for many blood diseases.
Definition and Medical Significance
Hematopoietic stem cell transplantation, or bone marrow transplant, is a treatment. It involves giving stem cells to fix the bone marrow. This treatment is vital because it can cure serious blood diseases.
HSCT is important for several reasons:
- It replaces bad bone marrow with good ones.
- It helps fight cancer cells.
- It helps the immune system work right again.
Historical Development of Transplantation Techniques
The history of HSCT started in the mid-20th century. Techniques have grown from simple bone marrow transplants to advanced stem cell transplants.
Important steps in HSCT’s growth include:
- The first bone marrow transplant was successful in 1956.
- HLA typing was introduced to match donors and recipients better.
- Peripheral blood stem cells became an option instead of bone marrow.
These changes have made HSCT a safer and more effective treatment. It gives hope to those with hard-to-treat diseases.
Understanding Hematopoietic Stem Cells
Hematopoietic stem cells are key to making blood cells. They help our body heal and fight off diseases. These cells create red blood cells, white blood cells, and platelets.
What Makes Hematopoietic Stem Cells Special
These stem cells can renew themselves and turn into different blood cells. This makes them very important for keeping blood cell counts healthy and responding to our body’s needs. They can keep their numbers up and make the blood cells we need for oxygen, fighting off infections, and clotting.
These stem cells are also vital in medical treatments. They are used in stem cell transplants to replace damaged or diseased blood cells with healthy ones.
The Role of Stem Cells in Blood Formation
Blood formation, or hematopoiesis, is a complex process. Hematopoietic stem cells are at the top of this process. They create:
- Red blood cells, which carry oxygen
- White blood cells, which fight off infections
- Platelets, which help with blood clotting
The hematopoietic definition also includes the maturation and release of these cells into the bloodstream. This process is controlled by growth factors and cytokines. It ensures the body has the right balance of blood cells.
In summary, hematopoietic stem cells are essential for both normal body functions and medical treatments. Their unique abilities make them a key part of bone marrow transplants and other treatments to restore healthy blood cell production.
Types of HSC Transplantation

It’s important to know about the different types of Hematopoietic Stem Cell (HSC) transplantation. This treatment is key for many blood disorders. Each type is designed for a patient’s specific needs.
Autologous Transplantation: Using Your Own Cells
Autologous hematopoietic stem cell transplantation uses the patient’s own stem cells. It’s great for some cancer patients. It lets them get strong chemotherapy and then get their stem cells back.
This method has its perks. It lowers the chance of getting sick from the transplant and helps the body recover faster. But, there’s a chance of getting cancer cells back if the bone marrow is affected.
Allogeneic Transplantation: Donor-Recipient Matching
Allogeneic hematopoietic cell transplantation uses stem cells from a donor. How well it works depends on how well the donor and recipient match.
Allogeneic transplantation has its benefits. It can help fight cancer in the body. But, it also risks causing sickness from the transplant and needs careful matching.
Syngeneic Transplantation: Identical Twin Donors
Syngeneic transplantation uses stem cells from an identical twin. This is the best match, making it safe from transplant sickness without needing strong medicines.
Though rare, syngeneic transplantation is the best choice for those with an identical twin. It’s a great option for those who can find a twin donor.
In summary, picking the right HSC transplantation depends on many things. These include the patient’s condition, donor availability, and the risks and benefits of each type. Knowing these details helps make better treatment choices.
Medical Conditions Requiring HSC Transplantation
Hematopoietic Stem Cell (HSC) transplantation is a key treatment for serious blood-related conditions. We look at the medical conditions that might need HSC transplantation. These include blood cancers and non-malignant blood disorders.
Blood Cancers
Blood cancers are a main reason for HSC transplantation. These include leukemia, lymphoma, and multiple myeloma.
- Leukemia: A cancer of the blood or bone marrow with too many white blood cells.
- Lymphoma: A blood cell tumor from lymphocytes.
- Multiple Myeloma: A blood cancer with too many plasma cells in the bone marrow.
Table 1: Common Blood Cancers Treated with HSC Transplantation
| Type of Cancer | Description | Role of HSC Transplantation |
| Leukemia | Cancer of the blood or bone marrow | Replaces cancerous cells with healthy stem cells |
| Lymphoma | Cancer of the lymphatic system | Used for high-risk or relapsed lymphoma |
| Multiple Myeloma | Cancer of plasma cells in the bone marrow | Part of intensive treatment regimens |
“HSC transplantation offers a potentially curative option for patients with high-risk or relapsed blood cancers, providing a second chance at life.”
Non-Malignant Blood Disorders
Non-malignant blood disorders also benefit from HSC transplantation. These include aplastic anemia, sickle cell disease, and thalassemia major.
- Aplastic Anemia: A condition where the bone marrow fails to produce blood cells.
- Sickle Cell Disease: A genetic disorder affecting hemoglobin production.
- Thalassemia Major: A severe form of anemia requiring regular blood transfusions.
Table 2: Non-Malignant Blood Disorders Treated with HSC Transplantation
| Condition | Description | Benefit of HSC Transplantation |
| Aplastic Anemia | Bone marrow failure | Restores bone marrow function |
| Sickle Cell Disease | Genetic disorder affecting hemoglobin | Corrects genetic defect, potentially curing the disease |
| Thalassemia Major | Severe anemia requiring frequent transfusions | Can eliminate need for lifelong transfusions |
The Donor Selection Process
Choosing the right donor for HSCT is key. It involves HLA typing and matching. We’ll look at why HLA compatibility matters and where stem cells come from.
HLA Typing and Matching Criteria
HLA typing is a big part of picking a donor. It makes sure the donor’s immune system fits with the recipient’s. This lowers the chance of graft-versus-host disease (GVHD) and other issues. HLA matching checks for specific genetic markers to see if the donor and recipient are compatible.
The criteria for HLA matching include:
- Testing for HLA-A, HLA-B, and HLA-DRB1 loci
- High-resolution HLA typing for the best match
- Looking at other genetic factors that affect compatibility
Sources of Hematopoietic Stem Cells
Stem cells can come from different places, each with its own benefits. The main sources are:
- Bone Marrow: Bone marrow is full of stem cells. Getting bone marrow needs a surgery under general anesthesia.
- Peripheral Blood: Peripheral blood stem cells are collected through apheresis after using growth factors to mobilize them.
- Umbilical Cord Blood: Cord blood is a great source of stem cells. It’s available right away and doesn’t need as strict HLA matching.
In summary, picking a donor for HSCT is complex. It involves HLA typing and matching, and where the stem cells come from. Understanding these helps improve HSCT outcomes and care for our patients.
Pre-Transplant Evaluation and Preparation
The success of HSCT relies heavily on a detailed pre-transplant evaluation and preparation. This includes a thorough patient assessment and specific conditioning regimens. It’s a critical phase that prepares patients well for the transplant, boosting the chances of a successful outcome.
Patient Assessment and Eligibility Criteria
Before starting HSCT, patients go through a detailed evaluation to check if they’re eligible for the transplant. This evaluation looks at their medical history, current health, and disease specifics.
Key factors considered during patient assessment include:
- Disease status and previous treatments
- Overall health and presence of comorbidities
- Age and physical condition
- Donor availability and compatibility
A leading expert stresses, “A detailed pre-transplant evaluation is key to spotting risks and improving patient outcomes.”
“The evaluation process is not just about assessing the patient’s current health; it’s about predicting their ability to withstand the transplant and subsequent recovery.”
– Hematologist
Conditioning Regimens
Conditioning regimens are a vital part of pre-transplant prep. They involve giving chemotherapy and/or radiation to clear out the diseased bone marrow and weaken the immune system. This makes room for the donor stem cells.
The goals of conditioning regimens are:
- To eliminate malignant cells
- To suppress the immune system, reducing the risk of graft rejection
- To create space in the bone marrow for the incoming stem cells
The specific conditioning regimen used can change based on the patient’s disease, health, and the type of HSCT.
By carefully evaluating patients and customizing conditioning regimens, we can greatly enhance the success rate of HSCT.
The Stem Cell Collection Process
Hematopoietic stem cells can be collected in different ways. Each method has its own benefits. The choice depends on the patient’s health, the type of transplant, and the stem cell availability.
Bone Marrow Harvest Procedure
Bone marrow harvest is a surgical method. It takes stem cells directly from the bone marrow, usually from the hip. The process needs general or regional anesthesia and small incisions to reach the marrow.
The marrow is then processed to get the stem cells ready for transplant.
Advantages of bone marrow harvest include:
- A rich source of stem cells
- Potential for immediate availability
But, it’s a surgery with risks like infection, bleeding, and pain at the site.
Peripheral Blood Stem Cell Collection
Peripheral blood stem cell collection is less invasive than bone marrow harvest. It uses growth factors to release stem cells into the blood. Then, apheresis separates these stem cells from other blood components.
The benefits of peripheral blood stem cell collection include:
- Less invasive than bone marrow harvest
- Faster recovery time
This method is popular because it’s safer and doesn’t require surgery.
Cord Blood Collection and Banking
Cord blood collection gets stem cells from the umbilical cord after birth. It’s non-invasive and painless. The cord blood is full of stem cells and can be stored for future use.
Cord blood banking offers several advantages:
- A readily available source of stem cells
- Potential for use in unrelated transplants due to the immaturity of cord blood cells
Cord blood is very useful for patients needing a transplant without a matched donor.
The HSC Transplantation Procedure Step by Step
It’s important for patients and doctors to know about the HSC transplant process. This detailed process has many steps, each one is key to a successful transplant.
The Infusion Process
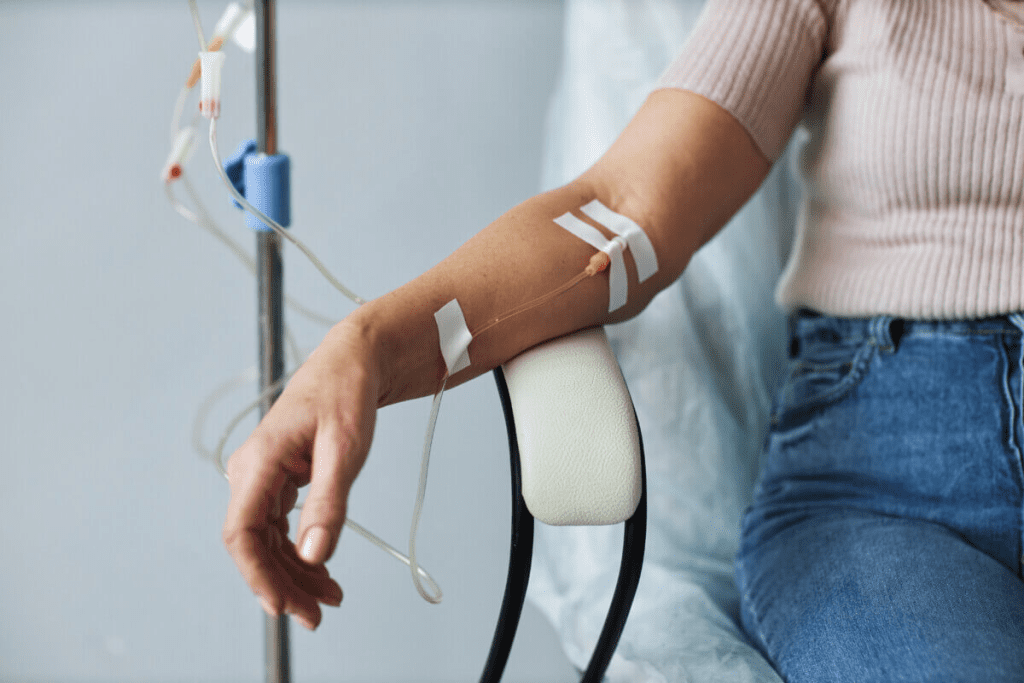
The infusion step is a big part of the HSC transplant. It’s when hematopoietic stem cells are given to the patient through their veins. This happens in a safe place like a hospital or special treatment center.
While the infusion happens, doctors keep a close eye on the patient. They watch for any bad reactions. The stem cells go into the body through a special tube in the vein.
Immediate Post-Infusion Monitoring
Right after the infusion, doctors start watching the patient closely. This is a very important time. They look for how the body reacts to the new stem cells and any problems.
Doctors check things like blood counts and how well organs are working. They also look for signs of graft-versus-host disease (GVHD). This is done in a hospital to make sure they can act fast if needed.
| Monitoring Parameter | Description | Clinical Significance |
| Blood Counts | Monitoring white blood cell, red blood cell, and platelet counts | Assesses engraftment and recovery of bone marrow function |
| Organ Function | Monitoring liver, kidney, and lung function | Detects possible organ damage or toxicity |
| GVHD Signs | Monitoring for symptoms such as skin rash, liver dysfunction, and gastrointestinal issues | Early detection of graft-versus-host disease |
By managing the infusion and watching the patient right after, doctors can make HSC transplants more successful.
The Engraftment Process Explained
Engraftment is when transplanted stem cells settle in the bone marrow of the patient. They start making blood cells. This is key for the success of stem cell transplants.
Timeline for Successful Engraftment
The time it takes for engraftment can change based on several things. This includes where the stem cells come from and the treatment plan. Usually, engraftment happens in 2-4 weeks after the transplant. During this time, patients are watched closely for signs of engraftment and any issues.
Waiting can be tough for patients and their families. Our medical team is here to offer full care and support during this time.
Monitoring Markers of Engraftment
We keep an eye on different markers to see how engraftment is going. These include:
- Blood cell counts: An increase in white blood cells is often the first sign of engraftment.
- Chimerism analysis: This test shows how many donor cells are in the bone marrow.
- Bone marrow biopsy: Sometimes, a bone marrow biopsy is done to check the marrow’s cells and shape.
By watching these markers, we can see if engraftment is on track. We can then adjust the patient’s care plan if needed.
Potential Complications and Side Effects
HSCT is a life-saving treatment for many, but it comes with risks. It’s important to know about these complications and side effects. Understanding them helps us manage them better.
Graft-Versus-Host Disease (GVHD)
Graft-Versus-Host Disease (GVHD) is a big risk after allogeneic HSCT. It happens when the donor’s immune cells attack the recipient’s body. GVHD can affect the skin, liver, and gut, and can be acute or chronic. Early detection and proper management are key to reducing GVHD’s impact.
Managing GVHD involves using immunosuppressive drugs and supportive care. We closely watch for GVHD signs and adjust treatments as needed.
Infections and Immune Suppression
HSCT patients face a higher risk of infections because of the treatment and weakened immune system. Infections can be a major cause of illness and death after transplant. We use many strategies to prevent infections, like antibiotics and watching for infection signs.
Immune suppression helps prevent GVHD but also raises infection risk. Finding the right balance in immune suppression is key to managing these risks.
Organ Damage and Long-term Effects
HSCT can cause long-term problems like organ damage and cancer. The treatment, GVHD, and long-term immune suppression can lead to these issues. Regular monitoring and follow-up care are vital to catch and manage these problems early.
Organ damage can affect the heart, lungs, or endocrine system, among others. We stress the need for long-term care to address these issues and improve patient outcomes.
Post-Transplant Care and Recovery Journey
After a hematopoietic stem cell transplant, patients start a recovery journey that needs careful care. The time after the transplant is key, and post-transplant care is vital for success.
The recovery journey is different for everyone. It depends on the transplant type, the patient’s health, and any complications. So, a care plan that fits each patient is important.
The First 100 Days
The first 100 days after the transplant are very important. Patients are watched closely for signs of engraftment, GVHD, and infections. A leading hematologist says,
“The first 100 days are a critical period where the foundation for long-term recovery is established.”
It’s key to stick to the follow-up schedule and report any symptoms or worries right away. This helps catch and manage problems early.
Long-term Follow-up Protocol
After the first 100 days, long-term follow-up is needed to keep an eye on the patient’s recovery. This includes regular check-ups, lab tests, and checks for long-term transplant effects.
- Regular monitoring for signs of GVHD
- Assessment of immune function
- Screening for secondary cancers
- Management of any long-term side effects
Immune System Reconstitution Timeline
The immune system reconstitution timeline is different for each patient but follows a general pattern. Knowing this timeline helps manage expectations and spot any problems.
As we keep improving in hematopoietic stem cell transplantation, focusing on post-transplant care and recovery is key. With full support and monitoring, we can greatly improve patient results.
Outcomes and Success Rates of HSC Transplantation
Hematopoietic Stem Cell (HSC) transplantation success depends on many factors. It’s important for patients and doctors to understand these factors. This knowledge helps in making informed decisions about treatment.
Factors Influencing Transplant Success
Several key factors affect HSC transplantation success. These include the patient’s diagnosis, age, and the match between donor and recipient. Donor-recipient matching is very important. A better match can lower the risk of serious complications like Graft-Versus-Host Disease (GVHD).
The patient’s health and any existing health conditions also play a role. Pre-transplant evaluation is key. It helps determine if the patient is a good candidate for the transplant and identifies possible risks.
Survival Statistics and Quality of Life Measures
Survival rates and quality of life are important for judging HSC transplantation success. Survival rates have gotten better thanks to new transplant methods and better care after the transplant. Quality of life measures show how well patients do physically and emotionally after the transplant.
Many patients live well after HSC transplantation, even returning to their life before the disease. But, long-term follow-up is needed. It helps catch any late effects and supports patients in their recovery.
Bone Marrow vs. Peripheral Blood Stem Cell Transplants
It’s important to know the differences between bone marrow and peripheral blood stem cell transplants. Both are used to treat blood-related disorders. They have different characteristics and effects on patients.
Terminology Clarification
First, let’s clear up some terms. A bone marrow transplant means moving stem cells from a donor’s bone marrow into a patient’s blood. A peripheral blood stem cell transplant collects stem cells from the donor’s blood and then gives them to the patient.
The term “stem cell transplant” can mean either. But knowing the source of the stem cells is key.
Clinical Advantages of Each Approach
Each transplant type has its own benefits. Bone marrow transplants are sometimes chosen because they have a lower risk of GVHD. GVHD is when the donor’s immune cells attack the patient’s body.
Peripheral blood stem cell transplants are faster. They help the patient’s blood counts recover quicker. This can lower the risk of infections and bleeding in the short term.
| Characteristics | Bone Marrow Transplant | Peripheral Blood Stem Cell Transplant |
| Source of Stem Cells | Bone Marrow | Peripheral Blood |
| Risk of GVHD | Lower | Higher |
| Engraftment Speed | Slower | Faster |
A study in a top medical journal says the choice between bone marrow and peripheral blood stem cell transplants depends on the patient’s needs and the situation.
“The decision to use bone marrow or peripheral blood stem cells for transplantation depends on a variety of factors, including the underlying disease, donor availability, and the recipient’s overall health status.”
– Expert Opinion
In summary, both bone marrow and peripheral blood stem cell transplants are important in HSCT. Each has its own benefits and things to consider. Understanding these differences helps healthcare providers and patients make better choices.
Recent Advances in HSC Transplantation
The field of hematopoietic stem cell transplantation (HSCT) is seeing big changes. These changes are making treatments better and safer for more people. They help make HSCT a good option for many patients.
Novel Conditioning Regimens
Conditioning regimens are key in HSCT. They get the patient ready for the transplant. New regimens are less harsh and more precise. They aim to cut down on side effects and make treatment easier to handle.
One big step is reduced-intensity conditioning (RIC). RIC uses less chemotherapy and radiation. This is good for older patients or those with health issues who can’t handle strong treatments.
| Conditioning Regimen | Description | Benefits |
| Myeloablative Conditioning | High-dose chemotherapy and/or radiation | Effective in eradicating cancer cells |
| Reduced-Intensity Conditioning (RIC) | Lower doses of chemotherapy and radiation | Less toxic, suitable for older patients or those with comorbidities |
| Non-Myeloablative Conditioning | Minimal chemotherapy and radiation | Minimal toxicity, promotes graft-versus-tumor effect |
Haploidentical Transplantation Techniques
Haploidentical transplantation uses a donor who is a half-match. This is often a family member. New techniques have made it a better option for those without a full match.
Post-transplant cyclophosphamide is a big help in haploidentical transplants. It helps control T cells and lowers the risk of GVHD while keeping the graft-versus-tumor effect.
Gene Therapy and Cellular Engineering
Gene therapy and cellular engineering are new and promising areas. They aim to improve HSCT results. These technologies modify cells to make them work better or fight disease better.
CRISPR-Cas9 gene editing is an exciting development. It lets us make precise changes to the genome. This could fix genetic problems and make HSCT safer and more effective.
As research keeps moving forward, we’ll see more breakthroughs in gene therapy and cellular engineering. These will help make HSCT even better.
Conclusion
Hematopoietic stem cell transplantation (HSCT) is a key treatment for serious diseases like blood cancers and non-malignant blood disorders. It involves moving healthy stem cells into a patient to help them make blood cells again. These stem cells can come from bone marrow, blood, or cord blood.
The success of HSCT depends on many things. These include matching the donor and recipient, the type of transplant, and the treatment plan. New ways to match donors and better treatment plans have made transplants more successful.
In short, HSCT has changed how we treat blood diseases, giving hope to many. As research keeps moving forward, we’ll see even better care for patients. This will greatly improve the lives of those with these conditions.
FAQ
What is hematopoietic stem cell transplantation?
Hematopoietic stem cell transplantation (HSCT) is a treatment. It replaces a patient’s sick or damaged blood system with healthy stem cells. These can come from the patient (autologous) or a donor (allogeneic).
What is the difference between bone marrow transplant and stem cell transplant?
Bone marrow transplant usually means transplanting bone marrow cells. Stem cell transplant can mean transplanting stem cells from bone marrow, blood, or cord blood.
What are the types of HSC transplantation?
There are three main types: autologous (using the patient’s own cells), allogeneic (using cells from a donor), and syngeneic (using cells from an identical twin).
What medical conditions require HSC transplantation?
It treats blood cancers and non-malignant blood disorders. This includes leukemia, lymphoma, and aplastic anemia.
How is a donor selected for HSCT?
Donor selection involves HLA typing and matching. This ensures the donor and recipient are compatible, reducing the risk of GVHD.
What is the engraftment process in HSCT?
Engraftment is when transplanted stem cells start working in the recipient’s bone marrow. They produce new blood cells. Successful engraftment is key to the transplant’s success.
What are the possible complications of HSCT?
Complications include GVHD, infections, organ damage, and long-term effects. These can be infertility and secondary cancers.
What is the post-transplant care and recovery journey like?
Post-transplant care involves close monitoring for the first 100 days. Then, long-term follow-up is needed to manage complications and ensure the immune system recovers.
What are the outcomes and success rates of HSC transplantation?
Success depends on the disease, donor-recipient match, and conditioning regimens. Survival rates and quality of life are used to measure outcomes.
What are the recent advances in HSC transplantation?
Advances include new conditioning regimens, haploidentical transplantation, and the use of gene therapy and cellular engineering.
How does a bone marrow transplant work for the donor?
Donors have their bone marrow cells collected, usually under general anesthesia. These cells are then given to the recipient. The donor’s bone marrow will grow back over time.
What is the role of hematopoietic stem cells in blood formation?
Hematopoietic stem cells create all blood cell types. This includes red blood cells, white blood cells, and platelets through hematopoiesis.
What is graft-versus-host disease (GVHD)?
GVHD is when the donor’s immune cells attack the recipient’s tissues. This can damage skin, liver, and the gastrointestinal tract.
How is immune system reconstitution achieved after HSCT?
The immune system rebuilds over time. Transplanted stem cells mature and produce new immune cells. This gradually restores the recipient’s immune function.
References
- Khaddour, K., & Armitage, J. O. (2023). Hematopoietic Stem Cell Transplantation. In StatPearls. National Center for Biotechnology Information. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK536951/
- Atkins, H. (2024). The HSCT procedure (I): Mobilization, collection, manipulation, and cryopreservation of a HSC graft. Handbook of Clinical Neurology, 202, 105-115.https://pubmed.ncbi.nlm.nih.gov/39111903/
- Hematopoietic stem cell transplantation (HSCT). (n.d.). Medscape. Retrieved from https://emedicine.medscape.com/article/208954-overview


































