
hematopoietic stem cell transplantation
Did you know that over 50,000 hematopoietic stem cell transplantations are done every year? They help treat serious diseases like some cancers and blood disorders.
Dealing with hematopoiesis disorders can be tough. Hematopoietic stem cell transplantation (HSCT) is a complex process. It replaces a patient’s bone marrow with healthy stem cells. This treatment has changed how we manage many blood-related diseases.
We’ll look into the importance of HSCT, its process, and its benefits. Our guide aims to give you deep insights into this life-saving treatment.
Key Takeaways
- HSCT is a medical procedure used to treat various life-threatening diseases.
- The treatment involves replacing a patient’s bone marrow with healthy stem cells.
- Over 50,000 HSCT procedures are performed worldwide each year.
- HSCT has revolutionized the management of hematological malignancies and disorders.
- Our comprehensive guide will explore the importance and benefits of HSCT.
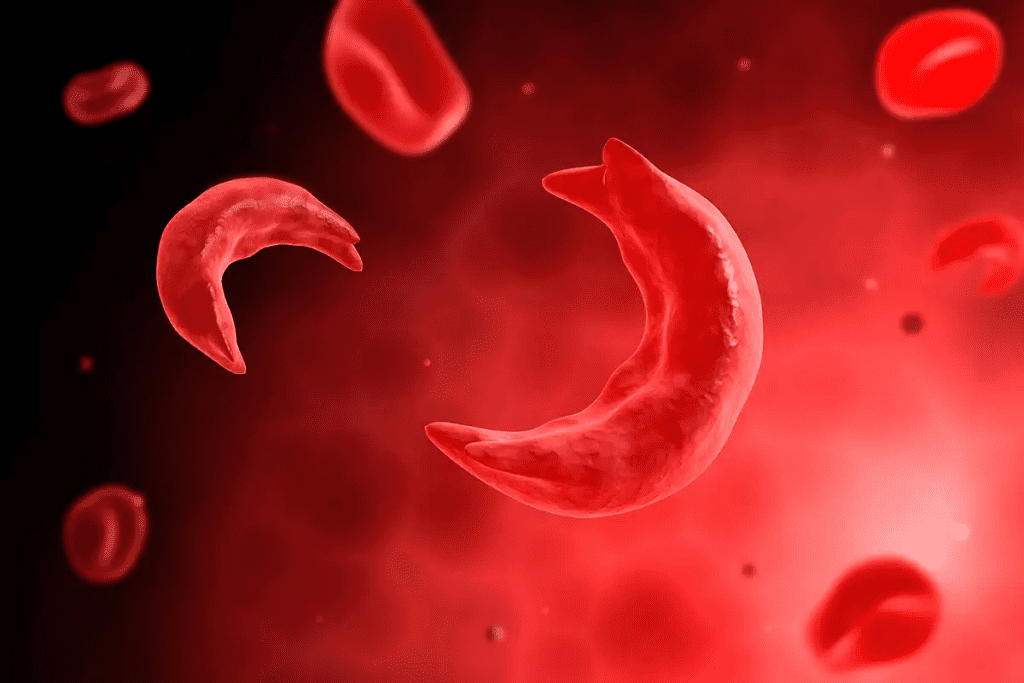
Understanding Hematopoiesis and Its Disorders
A cross-section of the hematopoiesis process within the bone marrow. Detailed view of the multipotent hematopoietic stem cells dividing and differentiating into various blood cell lineages. Warm, soft lighting illuminates the intricate network of blood vessels, stromal cells, and developing erythrocytes, leukocytes, and platelets. Crisp focus captures the dynamic process of blood cell production, highlighting the complexity and importance of this fundamental biological mechanism. Realistic medical illustration with a serene, educational atmosphere.
Hematopoiesis is key to keeping our blood cells healthy. It’s how our body makes red, white blood cells, and platelets. This process is vital for oxygen delivery, fighting infections, and stopping bleeding.
The Process of Blood Cell Formation
Blood cell formation happens in the bone marrow, a spongy tissue in our bones. Hematopoietic stem cells turn into all blood cells. They can change into different cell types.
The process has many stages, from stem cell renewal to blood cell maturation. Growth factors, cytokines, and molecular signals control it. For example, erythropoietin helps make red blood cells, and granulocyte-colony stimulating factor (G-CSF) aids in white blood cell production.
Common Disorders of Hematopoiesis
Disorders in hematopoiesis can cause health problems. Some common ones are:
- Anemia: A lack of red blood cells or hemoglobin, causing fatigue and weakness.
- Leukemia: A blood or bone marrow cancer that messes with blood cell production.
- Myelodysplastic syndromes: Bone marrow fails to make healthy blood cells.
- Aplastic anemia: Bone marrow doesn’t produce blood cells.
When Treatment Becomes Necessary
Treatment for hematopoietic disorders varies by cause and severity. Sometimes, hematopoietic stem cell transplantation (HSCT) is needed. HSCT replaces damaged bone marrow with healthy stem cells, from the patient or a donor.
Choosing HSCT depends on disease type, stage, patient health, and donor availability. Knowing these factors helps decide the best treatment.
Overview of Treatment Approaches for Hematopoietic Disorders
A realistic photo of a hematopoietic stem cell transplantation procedure, with a close-up of the physician’s hands performing the delicate procedure. The foreground should focus on the sterile medical instruments and the stem cell sample being carefully extracted. The middle ground should depict the patient’s arm with the IV line, and the background should show the medical equipment and monitoring devices in a well-lit, clinical environment. The overall atmosphere should convey a sense of precision, care, and the importance of this life-saving treatment for hematopoietic disorders.
Treatment for hematopoietic disorders can involve several methods. These include medicines, blood transfusions, and therapies like hematopoietic stem cell transplantation (HSCT). The right treatment depends on the disorder, its severity, and the patient’s health.
Medication-Based Treatments
Medicines are often the first step in treating hematopoietic disorders. They can include:
- Immunosuppressants to reduce the immune system’s attack on the bone marrow
- Growth factors to stimulate the production of blood cells
- Chemo therapy to kill cancerous cells in the bone marrow
For example, in aplastic anemia, immunosuppressive therapy can help the bone marrow recover.
Transfusion Therapies
Transfusion therapies involve giving blood components to replace missing or faulty cells. This can include:
| Blood Component | Indication |
| Red Blood Cells | Severe anemia |
| Platelets | Thrombocytopenia or platelet dysfunction |
| Granulocytes | Severe neutropenia with infection |
Regular transfusions can help manage symptoms and improve life quality for patients with certain disorders.
“Transfusion therapy is a critical component of supportive care for many patients with hematopoietic disorders, helping to alleviate symptoms and prevent complications.”
Cellular Therapies
Cellular therapies, including HSCT, are a big step forward in treating hematopoietic disorders. HSCT replaces a patient’s diseased or damaged bone marrow with healthy stem cells. This can:
- Reconstitute the patient’s bone marrow
- Restore normal blood cell production
- Potentially cure certain hematologic malignancies or disorders
The decision to do HSCT is based on a detailed look at the patient’s condition. This includes the type and severity of their disorder, overall health, and the risks of the procedure.
Hematopoietic Stem Cell Transplantation: Fundamentals
A high-resolution, photorealistic image of a hematopoietic stem cell transplantation procedure. The foreground shows a medical team carefully extracting stem cells from a patient’s bone marrow, using advanced medical instruments. The middle ground depicts the isolated stem cells being carefully processed and prepared for transplantation. The background showcases a modern, well-equipped hospital laboratory with state-of-the-art medical equipment, conveying a sense of medical expertise and innovation. Soft, natural lighting illuminates the scene, creating a calm, focused atmosphere. The overall composition emphasizes the precision and care involved in this complex medical procedure.
Understanding HSCT is key to seeing its importance in medicine today. It’s a major treatment for many blood cancers and disorders. This section will cover what HSCT is, its basic principles, and its history.
Definition and Basic Principles
Hematopoietic Stem Cell Transplantation uses stem cells to fix the bone marrow’s blood-making ability. It treats diseases like leukemia and genetic disorders. The success of HSCT depends on the stem cells’ source, donor match, and the treatment prep.
The main idea of HSCT is to replace a sick or damaged bone marrow with a healthy one. This is done by using strong chemotherapy or radiation to clear the old marrow. Then, healthy stem cells are given to the patient.
Historical Development of Bone Marrow Transplantation
The idea of bone marrow transplants started in the mid-20th century. Since then, we’ve learned a lot about HSCT and made it safer and more effective.
| Year | Milestone |
| 1968 | First successful bone marrow transplant |
| 1970s | Advancements in HLA typing and donor matching |
| 1980s | Introduction of cyclosporine to prevent GVHD |
| 1990s | Increased use of peripheral blood stem cells |
| 2000s | Development of reduced-intensity conditioning regimens |
Evolution to Modern HSCT Techniques
HSCT has changed a lot over the years. We’ve improved how we choose donors, harvest stem cells, and care for patients. Now, we use peripheral blood stem cells and umbilical cord blood as stem cell sources.
HSCT has also gotten better in how we prepare patients and prevent complications. These improvements have made HSCT more effective and available to more people.
In summary, HSCT has made huge strides since it started. Knowing about HSCT helps us understand its current and future roles in treating blood diseases.
Types of Hematopoietic Stem Cell Transplants
A detailed, realistic photographic illustration showcasing the various types of hematopoietic stem cell transplants. In the foreground, a clear visual representation of autologous, allogeneic, and syngeneic transplants, with labeled diagrams and cross-sectional views. In the middle ground, high-quality images of the medical equipment and procedures involved, captured with a professional camera lens. In the background, a softly blurred medical facility setting, with clean, sterile lighting to convey the clinical atmosphere. The overall mood should be informative, educational, and visually engaging, capturing the complexity and importance of these life-saving transplant techniques.
Hematopoietic Stem Cell Transplantation (HSCT) comes in different types. These are based on who the donor is and who gets the transplant. Each type offers unique treatment options.
Autologous Transplantation
Autologous transplantation uses the patient’s own stem cells. It’s often for patients with certain cancers like multiple myeloma or lymphoma. First, the patient’s stem cells are harvested. Then, they get high-dose chemotherapy. Finally, the stem cells are put back to help the bone marrow heal.
Advantages include no risk of graft-versus-host disease (GVHD) and quicker recovery. But, there’s a chance the graft could have cancer cells.
Allogeneic Transplantation
Allogeneic transplantation uses stem cells from a donor, usually a sibling or an unrelated donor with a matching Human Leukocyte Antigen (HLA) type. It’s for patients with leukemia or blood disorders.
Benefits include a chance for the donor’s immune cells to fight the patient’s cancer. But, it carries risks of GVHD and needs careful donor matching.
Syngeneic Transplantation
Syngeneic transplantation uses stem cells from an identical twin. It has the best HLA match, lowering GVHD risk.
But, finding an identical twin donor is rare. This limits its use.
Haploidentical Transplantation
Haploidentical transplantation uses a donor who is a half-match, often a family member. New technology has made it more possible, increasing the donor pool.
Key benefits include a bigger donor pool and quicker transplant times. But, it needs careful management to avoid GVHD and ensure the transplant works.
Sources of Hematopoietic Stem Cells
A detailed, scientifically accurate medical illustration depicting the primary sources of hematopoietic stem cells in the human body. In the foreground, an anatomical cross-section of bone marrow, highlighting the niche where hematopoietic stem cells are produced. In the middle ground, a magnified view of a hematopoietic stem cell, showcasing its distinctive morphology and capacity for self-renewal and differentiation. In the background, a wider view of the human body, with the locations of other significant hematopoietic stem cell reservoirs, such as the spleen and liver, clearly delineated. The overall image should convey a sense of scientific rigor and medical precision, with careful attention to lighting, depth of field, and anatomical accuracy to best support the "Sources of Hematopoietic Stem Cells" section of the article.
Hematopoietic stem cells come from different places, each with its own benefits and ways to collect them. These cells can be found in bone marrow, peripheral blood, and umbilical cord blood. The right source depends on the patient’s health, the availability of donors, and the transplant’s needs.
Bone Marrow Harvesting
Bone marrow harvesting is a classic way to get these cells. It takes stem cells from the bone marrow, usually from the hips. The process is done under general anesthesia to make it less painful. For years, it has been a reliable source of stem cells.
Peripheral Blood Stem Cell Collection
Peripheral blood stem cell collection is gaining favor because it’s less invasive than bone marrow harvesting. It moves stem cells from the bone marrow to the blood using special factors. Then, apheresis separates these cells from other blood parts. This method helps donors recover faster.
Umbilical Cord Blood Banking
Umbilical cord blood banking is also a key source of stem cells. It uses blood from the umbilical cord after birth. This is especially useful for patients without a matched donor. Cord blood banks store these cells for future use, making them ready for transplants.
The variety in sources of hematopoietic stem cells has opened up new ways to treat blood diseases. Each source has its own benefits, and the choice depends on the patient’s specific needs.
Patient Evaluation and Eligibility for Transplantation

A close-up view of a medical professional’s hands carefully pipetting liquid samples into a multi-well plate, with a high-resolution microscope and laboratory equipment in the background. The scene is bathed in a cool, neutral lighting, capturing the precise, scientific nature of the HLA typing process. The focus is sharp, drawing attention to the delicate movements and the intricate details of the lab equipment. The overall mood is one of meticulous, clinical efficiency, reflecting the importance of this evaluation step in the patient’s treatment journey.
To see if a patient can get a hematopoietic stem cell transplant (HSCT), we look at many things. This includes their health and other factors. It’s important to know if the transplant will help and if it’s safe.
Medical Assessment Criteria
When checking if someone can get HSCT, we look at their health closely. We check their disease, past treatments, and any other health issues. Important things are how bad the disease is, how well they’ve done with treatment before, and if their organs work well. We also see if they can handle the treatment and care after the transplant.
Some patients with heart or lung problems might face more risks. A team of experts looks at each case to decide the best plan.
HLA Typing and Donor Matching
HLA typing is key for finding the right donor for allogeneic HSCT. It helps find the best match between donor and recipient. A good match lowers the risk of complications and improves chances of success.
- HLA typing checks for specific genetic markers important for the immune system.
- Matching donors is done to find the best one, whether they’re related or not.
- The match affects the risk of problems and the treatment plan.
Psychological and Social Considerations
We also look at the patient’s mental and social health. This includes their mental health, support system, and ability to follow care instructions after the transplant. Having a strong support system is crucial for dealing with HSCT challenges.
Age-Related Considerations
Age is also a factor. While age isn’t a direct no for HSCT, older patients might face more challenges. We carefully check the health and fitness of older patients to see if they’re good candidates for HSCT.
- Older patients get a detailed geriatric assessment to check their physical and functional status.
- We consider their health issues and how they might affect transplant success.
- We create special plans to meet the needs of older patients getting HSCT.
Pre-Transplant Conditioning Regimens
A sterile, well-lit hospital room with a patient lying in a hospital bed undergoing pre-transplant conditioning regimens. Bright, crisp lighting illuminates the scene, casting long shadows and highlighting the various medical equipment and IV bags surrounding the patient. In the foreground, a nurse or doctor administers medications or treatments, with a focused, professional expression. In the middle ground, various medical instruments, tubes, and monitors indicate the complex procedures taking place. The background features additional hospital beds and medical personnel, creating a sense of a bustling, high-intensity medical environment. The overall atmosphere conveys the gravity and importance of the pre-transplant conditioning process, with a sense of care and attention to detail.
Pre-transplant conditioning regimens are key in getting patients ready for hematopoietic stem cell transplantation (HSCT). They aim to remove the old bone marrow, weaken the immune system, and make room for new stem cells.
Myeloablative Conditioning
Myeloablative conditioning uses strong chemotherapy and/or radiation to wipe out the bone marrow. It’s mainly for those with certain cancers like leukemia or lymphoma.
Benefits and Risks: This method can kill cancer cells but also risks harming the bone marrow and organs.
Reduced-Intensity Conditioning
Reduced-intensity conditioning (RIC) uses less chemotherapy and/or radiation. It’s gentler, making it safer for older patients or those with health issues.
Advantages: RIC is less harsh, reducing the risk of serious side effects and organ damage.
Non-Myeloablative Conditioning
Non-myeloablative conditioning is a form of RIC. It uses even less chemotherapy and/or radiation. The goal is to weaken the immune system enough for new stem cells to take hold without destroying the bone marrow.
Targeted Conditioning Approaches
Targeted conditioning uses specific treatments to target certain cells, like cancer or immune cells. This method aims to lower the harm from traditional treatments.
For instance, monoclonal antibodies can target specific cells. This helps reduce the risk of graft-versus-host disease (GVHD) and other problems.
| Conditioning Regimen | Intensity | Primary Use |
| Myeloablative | High | Leukemia, Lymphoma |
| Reduced-Intensity | Moderate | Older patients, Comorbidities |
| Non-Myeloablative | Low | Immune suppression |
| Targeted | Varies | Specific cell populations |
As shown in the table, each regimen has its own strengths and uses. The right choice depends on the patient’s disease, age, and health.
The Hematopoietic Stem Cell Transplantation Procedure
Getting ready for HSCT is a big deal. It starts with getting ready and goes all the way to aftercare. This detailed process has many important steps to make sure the treatment works.
Preparation Phase
The first step is getting ready for the transplant. We check the patient’s health and pick the best treatment plan. This step helps lower the risk of problems during the transplant.
Stem Cell Collection and Processing
Collecting stem cells is a key part of the transplant. We get them from bone marrow, blood, and umbilical cord blood. Then, we clean and freeze them until it’s time to use them.
Stem Cell Infusion Process
Infusing stem cells is like getting a blood transfusion. We thaw and put the stem cells into the patient’s blood. Patients might feel a bit sick or get a rash, but it’s usually okay.
Immediate Post-Transplant Care
After the transplant, we keep a close eye on the patient. We watch for infections or other problems. We also give them medicine and blood to help them get better.
| Phase | Description | Key Considerations |
| Preparation | Medical assessments and conditioning regimen | Minimizing risks and complications |
| Stem Cell Collection | Obtaining stem cells from various sources | Ensuring sufficient stem cell count |
| Stem Cell Infusion | Infusing cryopreserved stem cells | Managing potential side effects |
| Post-Transplant Care | Monitoring and managing complications | Providing supportive care |
Engraftment and Recovery Process
After a Hematopoietic Stem Cell Transplantation (HSCT), patients start a key phase. This is when the new stem cells start to grow. It’s a time when the patient’s blood-making system starts to work again.
Timeline for Blood Cell Recovery
The time it takes for blood cells to recover can vary. Neutrophil recovery usually happens in the first few weeks, between 2 to 4 weeks. Platelet recovery takes a bit longer, often 3 to 6 weeks.
| Blood Cell Type | Typical Recovery Time |
| Neutrophils | 2-4 weeks |
| Platelets | 3-6 weeks |
| Red Blood Cells | Several months |
Monitoring Engraftment Success
Checking how well the transplant is working is very important. Doctors do regular blood tests to see how the blood cells are doing. They also do chimerism analysis to see how many donor cells are in the bone marrow.
Supportive Care During Recovery
Supportive care is crucial during recovery. It helps manage problems, prevent infections, and keeps the patient feeling well. This can include growth factors, antibiotics, and nutrition support.
A team of doctors and nurses work together to care for patients during this time. They watch how the patient is doing and adjust the care as needed. This helps ensure the best possible recovery.
Managing Complications of Stem Cell Transplantation
HSCT can save lives but comes with risks. Knowing the possible complications and how to handle them is key.
Graft-Versus-Host Disease (GVHD)
Graft-versus-host disease (GVHD) is a big risk with allogeneic HSCT. It happens when the donor’s immune cells attack the recipient’s body. GVHD can be acute or chronic, with different levels of severity.
Management Strategies: To prevent GVHD, we use drugs to suppress the immune system. Treatment for GVHD includes stronger immune suppression and supportive care.
Infections and Immune Reconstitution
After HSCT, infections are a big worry because the body’s immune system is weak. It’s important to watch for infections and take preventive steps.
Management Strategies: We use antibiotics to prevent infections, watch for signs of infection, and use isolation when needed.
Organ Toxicities
Organ damage can happen because of the treatment and HSCT itself. This includes liver and heart problems.
Management Strategies: To prevent liver damage, we use ursodeoxycholic acid. We also closely watch the heart’s function.
Graft Failure
Graft failure is when the stem cells don’t work or make blood cells. It’s a serious issue.
Management Strategies: We keep a close eye on how well the graft is working. If it fails, we might use growth factors or do another transplant.
| Complication | Management Strategies |
| Graft-Versus-Host Disease (GVHD) | Prophylactic immunosuppressive drugs, intensifying immunosuppression, and supportive care |
| Infections | Antimicrobial prophylaxis, monitoring for infection signs, isolation precautions |
| Organ Toxicities | Ursodeoxycholic acid for hepatic veno-occlusive disease prevention, cardiac function monitoring |
| Graft Failure | Monitoring engraftment, growth factors, second transplants |
Pediatric Versus Adult Hematopoietic Stem Cell Transplantation
Understanding the differences between pediatric and adult HSCT is key for better patient care. Hematopoietic Stem Cell Transplantation is a complex process. It has different needs for kids and adults.
Unique Considerations in Pediatric Patients
Pediatric HSCT patients face special challenges. These include differences in disease, organ maturity, and long-term survival hopes.
Key considerations include:
- Immune system development
- Organ maturity and function
- Disease types and stages
Long-Term Developmental Impacts
HSCT can have big effects on kids long-term. It can affect their growth, development, and life quality.
Family-Centered Care Approaches
Family-centered care is vital in pediatric HSCT. It involves the patient and their family in the treatment.
| Aspect | Pediatric HSCT | Adult HSCT |
| Family Involvement | High | Variable |
| Support Systems | Family-centered | Patient-centered |
| Long-term Care | Extended follow-up | Standard follow-up |
Long-Term Follow-Up After Transplantation
After a hematopoietic stem cell transplantation (HSCT), patients need careful long-term care. This phase is key for watching for complications, managing late effects, and keeping survivors’ quality of life high.
Monitoring for Disease Recurrence
Long-term follow-up focuses on watching for disease return. Regular visits and tests help doctors catch relapse early. This early catch can greatly improve treatment results, studies show.
We tailor follow-up plans to each patient. This depends on their condition, transplant type, and other factors. This way, patients get the right care without feeling overwhelmed.
Managing Late Effects
HSCT can cause late effects like organ damage, endocrine issues, and new cancers. Managing these needs a team effort from different specialists. We work with patients to quickly spot and fix these problems.
For example, chronic graft-versus-host disease (cGVHD) needs ongoing treatment. We also watch for long-term side effects of treatments, like infertility and hormonal issues.
Quality of Life Considerations
Follow-up after HSCT is about more than just medical care. It’s also about improving patients’ quality of life. We look at physical health, mental well-being, and how well patients fit back into society.
One survivor said, “Getting back to normal life after HSCT is a journey. It takes patience, support, and understanding.” We offer counseling, rehab, and support groups to help patients on this journey.
Survivorship Programs
Comprehensive survivorship programs are crucial for long-term care. These programs meet the special needs of HSCT survivors. They give them the tools and support to live well.
Our programs include personalized care plans, healthy lifestyle education, and psychological support. By giving patients knowledge and resources, we help them live their best lives after HSCT.
Alternative Treatments to Hematopoietic Stem Cell Transplantation
New treatments are giving hope to patients. Medical research keeps growing. It’s important to look at these new options and their benefits.
Novel Targeted Therapies
Novel targeted therapies are a big step forward. They aim at specific parts of the disease, not harming healthy cells. Examples include tyrosine kinase inhibitors and monoclonal antibodies, which help treat blood cancers.
These therapies are more precise and have fewer side effects than old treatments. Clinical trials are showing they are safe and effective.
Immunotherapy Approaches
Immunotherapy is also making big strides. It uses the immune system to fight cancer. CAR T-cell therapy is a notable example, where T-cells are made to attack cancer cells.
Comparative Effectiveness and Decision-Making
When looking at new treatments, we must compare them. We need to see how well they work, how safe they are, and their benefits. This depends on the patient’s condition and health.
| Treatment Option | Efficacy | Safety Profile |
| Novel Targeted Therapies | High | Fewer side effects |
| Immunotherapy Approaches | Variable | Potential for severe side effects |
| Hematopoietic Stem Cell Transplantation | High | Risk of GVHD and other complications |
Choosing a treatment should be a team effort. The patient and their healthcare team should work together. They should consider the latest research and the patient’s unique situation.
Emerging Advances in Hematopoietic Treatments
New treatments for blood disorders are changing how we manage them. Breakthroughs in cellular and gene therapies are giving hope to those with few options before.
CAR T-Cell Therapy
CAR T-cell therapy is a big step forward for some blood cancers. It turns a patient’s T cells into cancer fighters. First, T cells are taken, then changed to find and kill cancer cells, and finally put back in the patient.
Studies show good results in some B-cell lymphomas and leukemias. But, it can cause serious side effects like cytokine release syndrome and neurotoxicity. So, choosing the right patients and managing their care is key.
Gene Therapy for Blood Disorders
Gene therapy is another new area for treating blood disorders. It fixes or changes genes to treat blood conditions. Viral vectors carry the gene to the patient’s cells.
- It’s showing promise for genetic diseases like sickle cell disease and beta-thalassemia.
- It’s also being looked at for acquired conditions like HIV.
Genome Editing Approaches
Genome editing, like CRISPR/Cas9, is being studied for editing genes in blood cells. It could fix genetic blood disorders by fixing the gene problem.
It’s still early, but genome editing might be a way to cure some conditions. Scientists are working to make it safer and more precise.
Artificial Hematopoiesis Research
Artificial hematopoiesis is about making artificial blood cells. It could change the game by offering a new way besides bone marrow transplants.
Stem cell biology and bioengineering are leading the way in this field. They could help treat many blood disorders.
The Economic and Practical Aspects of Transplantation
The cost of hematopoietic stem cell transplantation (HSCT) can be very high. It’s important to look at the economic and practical sides of this treatment. Understanding the financial side is key for patients, healthcare providers, and insurance companies.
Cost Considerations
The overall cost of HSCT depends on multiple factors, including transplant type, stem cell source, and patient health. These include the type of transplant, where the stem cells come from, and the patient’s health. Things like pre-transplant treatments, hospital stays, and care after the transplant add up a lot. We need to think about these costs when deciding if HSCT is affordable for each patient.
Insurance Coverage in the United States
In the U.S., how much insurance covers HSCT can vary a lot. It’s very important to know what your insurance covers to handle the costs of HSCT. We’ll talk about the general trends in insurance to help patients and families understand better.
- Most insurance plans cover some HSCT, but how much can differ a lot.
- You often need to get approval before getting treatment, and not all plans cover the same types or sources of stem cells.
- Patients should check their policy and talk to their insurance to know what’s covered.
Accessing Transplant Centers
Getting to specialized transplant centers is key for HSCT. These centers have the right skills and setup for successful transplants. We’ll talk about what affects access to these centers and how patients can get the care they need.
Things that affect access include where you live, your insurance, and what services the center offers. Sometimes, patients have to travel far to get to a good center. This adds to the cost and makes things more complicated.
Patient Assistance Programs
There are programs to help with the cost of HSCT. These programs offer financial help, support with getting things done, and emotional support to patients and their families. We’ll look at some important programs and resources.
- The National Marrow Donor Program (NMDP) helps with resources and support for HSCT patients.
- Groups like the Leukemia & Lymphoma Society give financial help and support services.
- Pharmaceutical companies also have programs to help with the cost of medications for HSCT.
Conclusion: The Future of Hematopoietic Disorder Treatments
Hematopoietic stem cell transplantation (HSCT) has changed how we treat many blood disorders. The field keeps growing, with new research and better ways to do HSCT. This includes finding better donors and improving care for patients.
New treatments like gene editing and CAR T-cell therapy are on the horizon. These could make treatments even better and give more options for patients. We’re excited about the possibilities these new therapies bring.
As treatments for blood disorders evolve, it’s crucial for doctors and patients to keep up with the latest. This way, we can give the best care and help those with these conditions live better lives.
FAQ
What is hematopoietic stem cell transplantation (HSCT)?
HSCT is a treatment that replaces a patient’s sick or damaged blood system with healthy stem cells. These stem cells can come from the patient themselves or a donor.
What is the difference between autologous and allogeneic HSCT?
Autologous HSCT uses the patient’s own stem cells. Allogeneic HSCT uses stem cells from a donor. Autologous is often for cancer, while allogeneic is for blood disorders like leukemia.
What are the sources of hematopoietic stem cells?
Stem cells can come from bone marrow, blood, or umbilical cord blood. Each source has its own benefits and is used in different situations.
What is the role of HLA typing in HSCT?
HLA typing is key in allogeneic HSCT. It makes sure the donor and recipient are compatible. This reduces the risk of complications like graft-versus-host disease.
What are the potential complications of HSCT?
HSCT can lead to graft-versus-host disease, infections, organ damage, and graft failure. Managing these risks is crucial after the transplant.
How long does it take for blood cells to recover after HSCT?
Blood cell recovery after HSCT takes weeks to months. It depends on how well the bone marrow starts producing healthy cells again.
What is the significance of long-term follow-up after HSCT?
Long-term follow-up is vital after HSCT. It helps monitor for disease return, manage late effects, and improve quality of life. Survivorship programs are key in this process.
Are there alternative treatments to HSCT?
Yes, there are alternatives like targeted therapies and immunotherapy. The choice between HSCT and these alternatives depends on the condition and patient needs.
What are the emerging advances in hematopoietic treatments?
New advances include CAR T-cell therapy, gene therapy, and genome editing. These innovations aim to improve treatment results.
What are the cost considerations for HSCT?
HSCT can be expensive. Costs vary based on the type of transplant, the center, and insurance. Patient assistance programs can help with costs.
How do I access transplant centers for HSCT?
To access transplant centers, start with a healthcare provider. They can refer you to a center. Then, you’ll go through an evaluation to see if you’re eligible for HSCT.
References
- Bazinet, A. (2019). A general practitioner’s guide to hematopoietic stem-cell transplantation. Canadian Medical Association Journal, 191(22), E601-E607. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6588058/
- UnitedHealthcare. (2025). Hematopoietic Stem Cell Transplantation “ Clinical Guideline. Retrieved from https://www.uhcprovider.com/content/dam/provider/docs/public/policies/clinical-guidelines/transplant-review-guidelines-hematopoietic-stem-cell-transplantation.pdf


































