When you have a blood-related issue, your doctor might send you to a specialist. Millions of people worldwide suffer from blood disorders. These can include anemia, bleeding disorders, and blood cancers like leukemia.
Getting referred to a specialist can feel both a relief and scary. A hematologist, or blood doctor, is a medical expert who deals with blood disorders. In this article, we’ll look at why hematologists are key in managing blood issues and why your doctor might suggest seeing one.
Key Takeaways
- Understanding the role of a hematologist is key in managing blood disorders.
- A hematologist diagnoses and treats various blood-related conditions.
- Your primary care physician may refer you to a hematologist for advanced care.
- Blood disorders can range from common conditions like anemia to complex cancers.
- Seeking specialized care can significantly improve treatment outcomes.
What Is a Hematologist?
A hematologist is a healthcare expert who knows a lot about blood and its problems. They study blood and its parts, and how to fix its disorders.
Definition and Specialization of Hematology
Hematology is all about blood diseases. It covers anemia, bleeding issues, and blood cancers. Hematologists can handle these tough cases, working with others in healthcare.
To become a hematologist, you need a lot of education and training. They go to medical school, then do residency and sometimes extra training in hematology.
The Difference Between a Hematologist and Other Medical Specialists
Hematologists focus on blood problems, unlike other doctors. While oncologists deal with cancer, hematologists also work on blood cancers. But, not all hematologists are oncologists. They also treat non-cancer blood issues.
| Specialist | Area of Focus | Examples of Conditions Treated |
| Hematologist | Blood and blood disorders | Anemia, bleeding disorders, blood cancers |
| Oncologist | Cancer | Solid tumors, leukemia, lymphoma |
| Primary Care Physician | General health and common conditions | Diabetes, hypertension, common infections |
Hematologists are key in healthcare, helping with blood disorders. They are experts in diagnosing and treating blood problems, working with other doctors.
Common Blood Disorders That Require Specialized Care
Hematologists are key in diagnosing and treating blood disorders. These affect millions worldwide, impacting quality of life. Seeking specialized care is vital.
Anemia and Related Conditions
Anemia is when the body lacks healthy red blood cells. This makes it hard to get enough oxygen. There are many types, like iron deficiency and vitamin deficiency anemia.
Symptoms include fatigue, weakness, and pale skin. Treatment varies based on the cause. It might include diet changes, supplements, or addressing the root issue.
Bleeding and Clotting Disorders
Bleeding disorders, like hemophilia, prevent proper clotting. This leads to long-lasting bleeding. Clotting disorders, such as DVT, cause blood clots that block blood flow.
| Bleeding Disorders | Clotting Disorders |
| Hemophilia A and B | Deep Vein Thrombosis (DVT) |
| Von Willebrand Disease | Pulmonary Embolism |
| Platelet Disorders | Factor V Leiden Thrombophilia |
Both types need careful management by a hematologist. This helps prevent complications and improves life quality.
“The diagnosis and treatment of bleeding and clotting disorders require a thorough approach, including lab tests and clinical evaluation.” – A leading hematologist
White Blood Cell Abnormalities
White blood cell issues can signal infections or leukemia. Neutropenia and lymphocytosis need investigation. A hematologist will use blood tests and sometimes bone marrow biopsies to diagnose and treat.
Understanding these disorders highlights the importance of hematologists. They provide specialized care, improving patient outcomes.
The Connection Between Hematology and Oncology
Hematology and oncology are closely related. Many hematologists are also oncologists. This is because they need to care for patients with blood cancers. They have to understand both the blood system and cancer treatment.
Why Many Hematologists Are Also Oncologists
Many blood disorders, like anemia and blood cancers, need a deep understanding of both systems. Hematologist oncologists can diagnose and treat these conditions. They offer a complete care approach.
Some reasons for this overlap include:
- High rates of blood cancers like leukemia and lymphoma.
- The need for full management of cancers affecting the blood and bone marrow.
- The complexity of diagnosing and treating blood disorders with cancer implications.
Blood Cancers and Their Treatment Approaches
Blood cancers are challenging to diagnose and treat. Hematologist oncologists use various treatments like chemotherapy and targeted therapy. They also use immunotherapy and stem cell transplantation.
The treatment depends on the cancer type, stage, and patient’s health. Here are some common blood cancers and their treatments:
- Leukemia: Treatment may include chemotherapy, targeted therapy, or stem cell transplantation.
- Lymphoma: Therapy can include chemotherapy, radiation, and immunotherapy.
- Multiple Myeloma: Treatment often involves a combination of targeted therapy, chemotherapy, and stem cell transplantation.
When Cancer Affects Blood Components
Cancer can harm blood components, causing anemia and other issues. Hematologist oncologists manage these problems. They ensure patients get care for both their cancer and blood health.
Understanding the link between hematology and oncology helps patients. It shows the importance of hematologist oncologists. Their integrated care is key for treating blood cancers and disorders well.
Warning Signs That May Lead to a Hematologist Referral
If you notice unusual symptoms or get abnormal blood test results, you might need to see a hematologist. A hematologist is a doctor who deals with blood disorders. Knowing the signs that might lead to a referral can help you get ready for your visit.
Abnormal Blood Test Results That Raise Concerns
Abnormal blood test results often mean you’ll see a hematologist. These results can show many blood-related issues, like anemia or blood cancers. Some specific issues that might worry you include:
- Low red blood cell count or hemoglobin levels
- High or low white blood cell count
- Abnormal platelet count
- Unusual blood cell morphology
These problems can show up in a complete blood count (CBC) test. This is a common test doctors use.
Persistent Symptoms That Suggest Blood Disorders
Certain symptoms can hint at blood disorders, leading to a hematologist visit. These symptoms might be:
- Fatigue or weakness
- Pale skin or jaundice
- Frequent infections
- Easy bruising or bleeding
- Swollen lymph nodes or spleen
If you keep getting these symptoms, talk to your doctor. They might send you to a hematologist for more checks.
Family History Considerations for Blood Conditions
Having a family history of blood disorders raises your risk. For instance, if your family has:
- Hemophilia
- Sickle cell disease
- Thalassemia
- Blood cancers
Your doctor might suggest regular checks or send you to a hematologist for early care.
| Blood Condition | Family History Risk | Preventive Measures |
| Hemophilia | High | Regular monitoring, genetic counseling |
| Sickle Cell Disease | High | Genetic testing, preventive care |
| Thalassemia | High | Genetic testing, regular blood tests |
Unexplained Bleeding or Bruising
Unexplained bleeding or bruising might mean a blood disorder. If you notice:
- Frequent nosebleeds
- Bleeding gums
- Easy bruising
- Prolonged bleeding after injuries or surgery
See your doctor, who might send you to a hematologist for diagnosis and treatment.
The Referral Process: From Primary Care to Specialized Blood Care
Getting specialized blood care starts with the referral process. This step is key to finding the right healthcare specialist. Your primary care doctor will start this process if they think you need more help for a blood issue.
Understanding the AMB Referral System
The AMB referral system makes it easier to get to the right specialist. Here’s how it works: your primary care doctor checks if you need a hematologist. If yes, they’ll give you a referral. This might mean scheduling an appointment with the specialist or giving you a slip to take to the hematologist.
Insurance Considerations and Requirements
Insurance is a big part of the referral process. Each insurance company has its own rules for referrals. Some might need a doctor’s referral to see a specialist.
‘Understanding your insurance coverage is key,’ says a hematologist at a leading medical center. ‘Patients should check their insurance before getting specialized care to avoid surprise costs.’
Self-Referral vs. Physician Referral Options
Some insurance plans let you see a specialist without a doctor’s referral. This is called self-referral. But, you should always check with your insurance first. This way, you avoid any problems with coverage.
What to Expect During Your First Hematologist Appointment
Seeing a hematologist for the first time can be scary. Let’s go over what usually happens at your first visit. Your first hematologist appointment is key to understanding your condition and creating a treatment plan just for you.
Typical Examination Procedures
At your first visit, the hematologist will start by asking about your medical history and doing a physical exam. They might check for signs of bleeding or bruising, look at your lymph nodes, and check for symptoms related to your blood disorder.
A typical physical examination may include:
- Checking your vital signs
- Examining your skin for signs of bruising or petechiae
- Palpating your abdomen to check for spleen enlargement
- Inspecting your lymph nodes for swelling
Common Questions Your Hematologist Will Ask
Your hematologist will ask you many questions to understand your symptoms, medical history, and lifestyle. Being ready to answer these questions can make your visit more productive.
Some common questions include:
- Can you describe your symptoms and when they started?
- Do you have a family history of blood disorders?
- Have you recently traveled or been exposed to infections?
- What medications are you currently taking?
“The key to a successful diagnosis is a thorough understanding of the patient’s medical history and symptoms.” – Hematologist
Initial Tests and Evaluations
After your initial consultation, your hematologist might order several tests to diagnose your condition. These can include:
| Test | Purpose |
| Complete Blood Count (CBC) | To analyze the different components of your blood |
| Blood Smear | To examine the morphology of blood cells |
| Coagulation Tests | To assess your blood’s clotting ability |
Creating a Treatment Plan
Once your diagnosis is confirmed, your hematologist will work with you to create a personalized treatment plan. This might include medication, lifestyle changes, or other interventions tailored to your specific condition.
By knowing what to expect at your first hematologist appointment, you can feel more prepared and confident as you take this important step in your healthcare journey.
Diagnostic Tools and Tests Used by Hematologists
Hematologists use many advanced tools to diagnose blood disorders. These tests help them understand blood conditions well. This knowledge is key to creating effective treatment plans.
Complete Blood Count and What It Reveals
A Complete Blood Count (CBC) is a common test in hematology. It checks the blood’s red, white cells, and platelets. A CBC can show a lot about a patient’s health, like:
- Anemia or polycythemia
- Infections or inflammatory conditions
- Bleeding or clotting disorders
- Blood cancers or other malignancies
Specialized Blood Tests for Specific Conditions
Hematologists also use specialized blood tests for certain conditions. These include:
- Coagulation studies for bleeding disorders
- Flow cytometry for blood cancers
- Genetic testing for inherited blood conditions
Bone Marrow Biopsies and Aspirations
Bone marrow biopsies and aspirations are key in hematology. They take a bone marrow sample for study. These tests can find:
- Blood cancers like leukemia or lymphoma
- Bone marrow failure syndromes
- Metastatic cancer in the bone marrow
We do these procedures carefully. This ensures patients get accurate diagnoses and good treatment plans.
Advanced Imaging and Other Diagnostic Procedures
Hematologists also use advanced imaging techniques like MRI or CT scans. These help see how far blood disorders have spread. They can spot complications or related issues.
By combining these diagnostic tools and tests, we get a full picture of a patient’s condition. This lets us create a treatment plan that fits their needs.
How a Hematologist Works With Your Healthcare Team
Hematologists are key members of the healthcare team. They work with primary care physicians and other specialists. This team approach ensures all aspects of a patient’s health are considered.
Collaboration With Primary Care Physicians
Primary care physicians are often the first point of contact for patients. They play a key role in identifying when specialized care is needed. Hematologists work closely with primary care physicians to understand the patient’s medical history and current condition.
If a primary care physician suspects a patient has anemia, they may refer them to a hematologist. The hematologist can then communicate with the primary care physician about the diagnosis and treatment plan. This ensures the patient’s overall health is managed effectively.
Coordination With Other Specialists
Blood disorders can be complex and may require input from various medical specialists. Hematologists coordinate with other specialists such as oncologists and cardiologists. For example, a patient with a bleeding disorder may need to see a hematologist and an orthopedic surgeon.
This multidisciplinary approach ensures all aspects of the patient’s health are addressed. It also helps in managing complications and improving the patient’s quality of life.
Communication Between Healthcare Providers
Effective communication is the backbone of successful collaboration in healthcare. Hematologists, primary care physicians, and other specialists must communicate clearly and regularly. This includes sharing medical records, test results, and treatment plans to ensure everyone is on the same page.
Regular communication helps prevent misunderstandings and reduces the risk of medical errors. It ensures the patient receives cohesive care. It also facilitates adjustments to treatment plans as needed.
Treatment Approaches in Modern Hematology
Modern hematology has made big strides, with many treatment options for blood disorders. Each patient’s needs are unique, so treatments must be tailored. This ensures the best care for each person.
Medication-Based Treatments
Medications play a key role in treating blood disorders. They include:
- Anticoagulants: To prevent blood clots.
- Antiplatelet drugs: To stop platelets from sticking together.
- Clotting factor concentrates: For bleeding disorders.
- Immunosuppressants: To stop the immune system from attacking blood cells.
These drugs are often used with other treatments for better results.
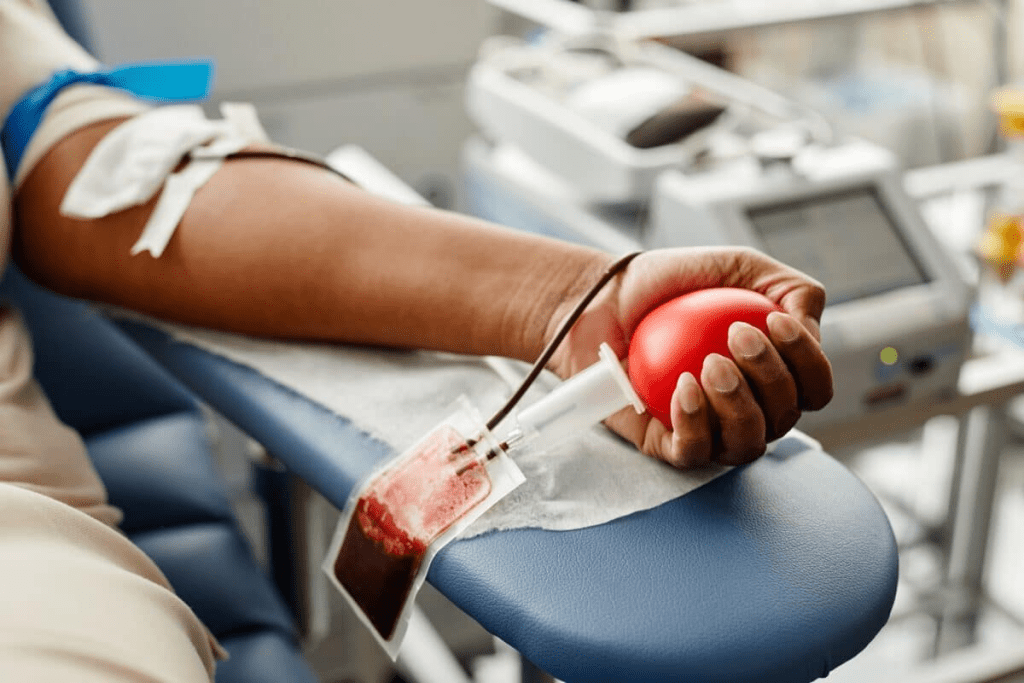
Transfusion Therapies and Blood Products
Transfusion therapies use blood products to replace or add to a patient’s blood. This includes:
- Red blood cell transfusions: To treat anemia or blood loss.
- Platelet transfusions: For low platelet counts.
- Plasma transfusions: To replace clotting factors or proteins.
These therapies are vital for managing blood disorders and are used in emergencies.
Surgical Interventions When Necessary
Surgery is sometimes needed to treat blood-related conditions. This includes:
- Splenectomy: Removing the spleen for certain blood disorders.
- Bone marrow transplantation: Replacing diseased marrow with healthy marrow.
Surgery is considered when other treatments don’t work or are not possible.
Emerging Treatments and Clinical Trials
Hematology is always evolving, with new treatments being developed. New options include:
- Gene therapy: To fix genetic defects in blood disorders.
- Targeted therapies: Drugs that target specific molecules in blood diseases.
- Immunotherapies: Treatments that use the immune system to fight blood cancers and disorders.
Joining clinical trials can give patients access to these new treatments. It also helps advance hematological care.
When Children Need to See a Hematologist
It’s important to know when a child needs to see a hematologist. Kids with blood disorders need special care that’s different from regular pediatric care.
Pediatric Blood Disorders and Their Unique Challenges
Pediatric blood disorders are special because kids’ health is delicate. Conditions like anemia, bleeding disorders, and blood cancers need careful diagnosis and treatment.
Some common pediatric blood disorders include:
- Sickle cell disease
- Hemophilia
- Leukemia
- Thalassemia
Special Considerations for Young Patients
Hematologists must think about a child’s age, health, and treatment effects. This means they need a care plan that’s different from adults.
| Condition | Common Symptoms | Treatment Approach |
| Sickle Cell Disease | Anemia, pain crises | Hydration, pain management, sometimes blood transfusions |
| Hemophilia | Bleeding into joints or muscles | Replacement of the missing clotting factor |
| Leukemia | Fever, fatigue, bleeding | Chemotherapy, sometimes bone marrow transplant |
Family Support for Children With Blood Conditions
Family support is key for kids with blood disorders. It includes emotional support, helping with medicine, and dealing with the condition’s effects.
Key aspects of family support include:
- Educating family members about the condition
- Encouraging open communication about feelings and concerns
- Helping manage the treatment regimen
With the right care and support, we can help kids with blood disorders live better lives.
The Education and Training of a Hematologist
Becoming a hematologist is a long and challenging journey. It involves many stages of education and training. This process prepares them to diagnose and treat blood disorders well.
Medical School and Residency Requirements
It starts with medical school. Here, future hematologists get a Doctor of Medicine (M.D.) or Doctor of Osteopathic Medicine (D.O.) degree. Medical school takes four years and teaches the basics of medicine and clinical practice.
After medical school, they enter a three-year internal medicine residency. They learn to diagnose and manage adult diseases, including blood-related ones. This hands-on experience is key.
Key components of internal medicine residency include:
- Direct patient care under the supervision of experienced physicians
- Learning to diagnose and manage various medical conditions
- Developing skills in patient communication and medical ethics
Fellowship and Specialization in Hematology
After the residency, they pursue a hematology fellowship. These programs last two to three years. They focus on blood disorders and provide deep clinical experience.
Fellowship training covers many topics. This includes bleeding and clotting disorders, blood cancers, and anemia. They learn to interpret tests, plan treatments, and manage complex cases.
Ongoing Education and Board Certification
Education for hematologists doesn’t stop after fellowship. They must keep learning to stay updated. Board certification is also a must.
To get certified, they pass a tough exam. They must also keep up with continuing education and follow professional standards. This ensures they provide top care for their patients.
“Continuing education is key for hematologists. It helps them keep up with new treatments and technologies.”
Through extensive education, specialized training, and ongoing learning, hematologists are ready to care for patients with complex blood disorders.
How to Prepare for Your Hematologist Visit
To get the most out of your hematologist visit, being prepared is key. It makes the visit more effective and helps lower your anxiety. It also ensures you get the best care possible.
Medical Records and Information to Bring
Gathering all your medical records and information is a must. This includes your medical history, test results, and current medications. Make a list of your medications, including dosages and how often you take them. Also, note any allergies you have. These documents help your hematologist understand your situation better and make informed decisions.
Questions to Ask Your Hematologist
It’s important to prepare a list of questions for your hematologist. Writing down your questions beforehand helps you remember to ask them. You might want to ask about your diagnosis, treatment options, possible side effects, and what to expect at future appointments. Being ready with questions ensures you get the most out of your visit.
Follow-up Appointment Guidelines
Knowing the rules for follow-up appointments is key to managing your health. Your hematologist will tell you how often to come back based on your condition and treatment. It’s important to remember these appointments and any tests or exams needed before your next visit. Using a calendar or a reminder app can help you stay on track.
Managing Anxiety About Your Appointment
It’s normal to feel anxious about seeing a hematologist, but there are ways to cope. Preparing mentally and having support can greatly reduce your anxiety. Consider bringing a friend or family member for support. Also, try relaxation techniques like deep breathing or meditation to calm your nerves before and during the visit.
Conclusion: The Vital Role of Hematologists in Modern Healthcare
Hematologists are key in diagnosing and treating blood disorders. They offer specialized care that is vital in today’s healthcare. These doctors focus on blood-related conditions like anemia, bleeding disorders, and blood cancers.
Their work is essential for better patient care. They use the latest tools and treatments for blood issues. By working with other doctors, hematologists give patients the best care possible. They help with both the physical and emotional needs of patients.
As medical research and technology improve, hematologists’ role becomes even more important. Their expertise is vital for handling blood disorders. They are a cornerstone of modern healthcare.
FAQ
What is a hematologist?
A hematologist is a doctor who deals with blood disorders and diseases. They diagnose, treat, and manage these conditions.
What does a hematologist do?
Hematologists treat blood disorders like anemia and blood cancers. They also handle blood transfusions and related therapies.
Why would I be referred to a hematologist?
You might see a hematologist if your blood tests show problems. Or if you have symptoms like unexplained bleeding or bruising.
What is the difference between a hematologist and an oncologist?
Hematologists focus on blood disorders. Oncologists deal with cancer. But, many hematologists also treat blood cancers.
What is hematology/oncology?
Hematology/oncology is a field that treats blood disorders and cancer. It often focuses on blood cancers and related issues.
Do I need a referral to see a hematologist?
It depends on your insurance and local healthcare rules. Some plans need a referral from your doctor. Others don’t.
What should I expect during my first hematologist appointment?
Expect a detailed medical history and physical exam. You’ll talk about your symptoms and might get some tests.
What diagnostic tests are used by hematologists?
Hematologists use blood tests, bone marrow biopsies, and imaging. These help diagnose and monitor blood disorders.
How do hematologists work with other healthcare providers?
Hematologists work with other doctors to ensure you get the best care. They share information and coordinate treatment plans.
What treatment approaches are used in hematology?
Treatments include medicines, transfusions, and sometimes surgery. They also participate in clinical trials for new treatments.
Can children see a hematologist?
Yes, children can see a hematologist for blood disorders. They need specialized care that considers their age and needs.
How do I prepare for a hematologist visit?
Gather your medical records and write down your questions. Be ready to discuss your symptoms and medical history in detail.
What is an AMB referral?
An AMB referral is part of the referral process for specialized care. Its meaning can vary depending on the healthcare system.
Are hematologists and oncologists the same?
Not always. But, many hematologists also treat blood cancers, which is part of oncology.
How long does it take to become a hematologist?
It takes years to become a hematologist. You need to finish medical school, residency, and fellowship training in hematology
References
National Center for Biotechnology Information. (2023, April 30). Techniques for hematological disorders. https://www.ncbi.nlm.nih.gov/books/NBK593683/


































