Last Updated on October 21, 2025 by mcelik
Myelodysplastic syndrome (MDS) is a serious condition that affects how blood cells are made. Every year, about 4,000 to 5,000 people in the United States get diagnosed with MDS. This highlights the significance of understanding this pre-cancerous blood condition.
MDS makes the bone marrow produce abnormal blood cells. This can cause many health problems. It’s key for patients, caregivers, and doctors to understand MDS’s causes, symptoms, and treatments.
Key Takeaways
- MDS is a pre-cancerous blood condition that affects blood cell production.
- The condition can lead to severe health complications if left untreated.
- Understanding MDS is key for patients, caregivers, and healthcare professionals.
- MDS diagnosis involves various tests, including blood tests and bone marrow biopsy.
- Treatment options for MDS vary depending on the severity and type of the condition.
Pre-Cancerous Blood Conditions Explained
Pre-cancerous blood conditions, like myelodysplastic syndrome (MDS), are disorders where blood cells grow abnormally. They can turn into serious cancers if not caught early.
Definition and General Characteristics
A pre-cancerous blood condition means blood cells are not normal but not cancer yet. MDS is a case where the bone marrow can’t make healthy blood cells. This leads to problems like anemia, infections, and bleeding issues.
MDS is marked by abnormal cells in the bone marrow and blood. This shows a problem with making blood cells right.
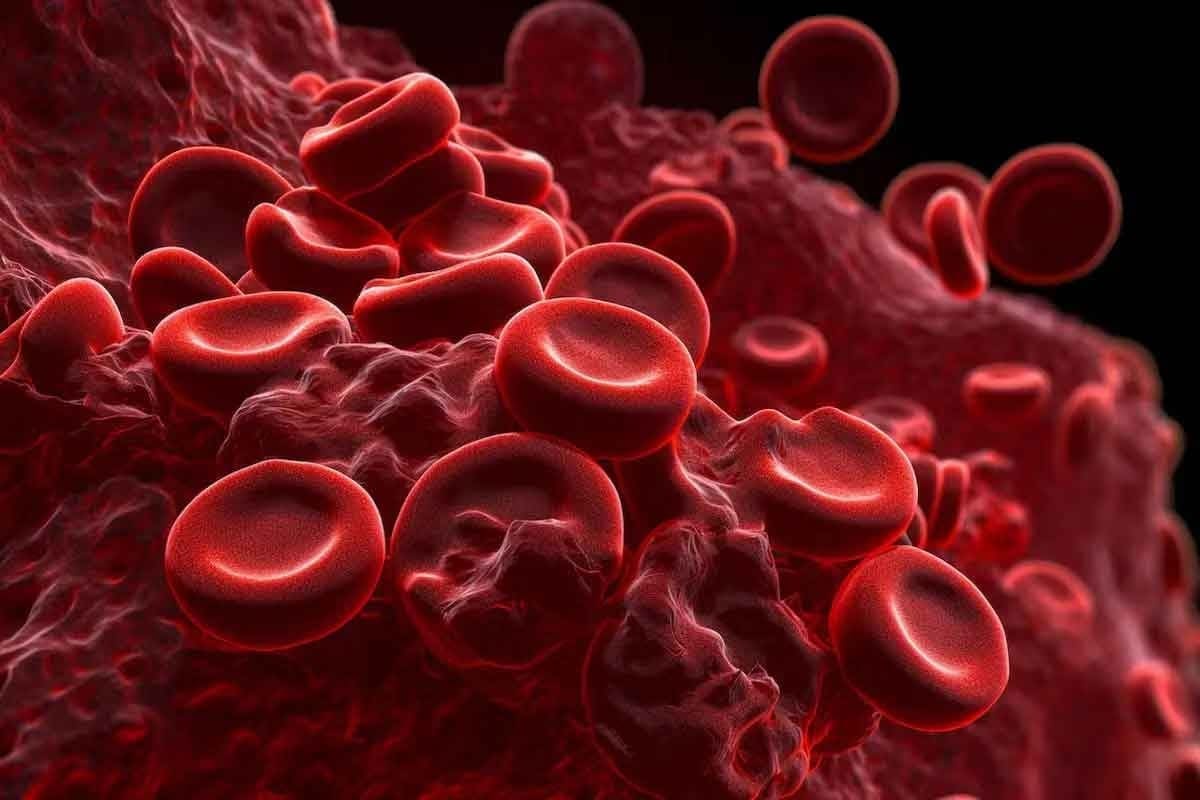
The Blood and Bone Marrow System
The blood and bone marrow system is key for making blood cells. The bone marrow, a soft tissue in bones, makes:
- Red blood cells, which carry oxygen
- White blood cells, important for fighting infections
- Platelets, needed for blood to clot
In healthy people, the bone marrow makes these cells well. But in MDS, it makes bad cells instead.
Myelodysplastic Syndrome: An Overview
MDS, or myelodysplastic syndrome, is a condition where the bone marrow can’t make healthy blood cells. This leads to a range of blood problems.
Definition and Basic Characteristics
Myelodysplastic syndrome (MDS) is a group of disorders that affect the bone marrow. It makes it hard for the bone marrow to produce blood cells. This results in anemia, infections, and bleeding problems.
The bone marrow in people with MDS has abnormal cells. These cells don’t turn into healthy blood cells. This causes fatigue, more infections, and bleeding issues.
Prevalence and Demographics
MDS can happen to anyone, but it’s more common in older adults. Most cases are found in people over 60. Studies show that MDS happens in 3 to 5 people per 100,000 each year. This number goes up for those over 70.
Some studies suggest MDS is more common in men. Knowing who gets MDS helps doctors find it early and treat it better.
How MDS Affects Blood Cell Production
MDS affects the production of red, white blood cells, and platelets. The bone marrow doesn’t work right, leading to:
- Anemia because of too few red blood cells
- More infections because of low white blood cells
- Bleeding problems because of low platelets
These problems show how complex MDS is. It needs a detailed plan to manage its effects.
Types of Myelodysplastic Syndrome
MDS is divided into subtypes based on the number of blasts in the bone marrow and genetic changes. Knowing these subtypes helps doctors predict outcomes and choose treatments.
Low-Risk MDS Types
Low-risk MDS has fewer blasts and less cytopenia. People with these types usually have a better outlook.
- MDS with single lineage dysplasia
- MDS with multilineage dysplasia
High-Risk MDS Types
High-risk MDS has more blasts and a higher chance of turning into acute myeloid leukemia (AML).
- MDS with excess blasts-1
- MDS with excess blasts-2
MDS with Specific Genetic Abnormalities
Some MDS types are marked by specific genetic changes. These changes affect how well the disease can be treated and how it will progress.
| Genetic Abnormality | Subtype | Prognostic Implication |
| del(5q) | MDS with isolated del(5q) | Favorable |
| -7 or del(7q) | MDS with -7 or del(7q) | Poor |
The variety in MDS subtypes shows how complex the disease is. It emphasizes the importance of tailored treatments for each patient.
Causes and Risk Factors of MDS
Knowing the causes and risk factors of MDS is key for early treatment. Myelodysplastic Syndrome (MDS) is a disorder where blood cells don’t form right. This often leads to the bone marrow failing.
Primary (De Novo) MDS
Primary MDS, or de novo MDS, happens without any known cause. It’s not clear why it happens, but genetics are thought to be a big part of it.
Secondary MDS
Secondary MDS comes after being exposed to harmful substances like chemotherapy or radiation. This type is usually more aggressive and has a worse outlook than primary MDS.
Age and Gender Factors
Age is a big risk factor for MDS, with most cases in people over 60. Men are slightly more likely to get MDS than women.
Genetic Predisposition
Genetics also play a role in MDS. Some genetic mutations can make you more likely to get MDS.
| Risk Factor | Description | Impact on MDS Risk |
| Age | Majority of cases diagnosed over 60 years old | Increased risk with age |
| Gender | Men slightly more likely than women | Moderate increase in men |
| Genetic Mutations | Certain mutations increase MDS risk | Significant increase with specific mutations |
| Chemotherapy/Radiation Exposure | Secondary MDS risk factor | High risk for secondary MDS |
The table above lists main risk factors for MDS, like age, gender, genetics, and exposure to harmful substances. Knowing these can help spot MDS early and manage it better.
Myelodysplastic Syndrome Symptoms
Myelodysplastic syndrome (MDS) has symptoms that can really affect a person’s life. Knowing these symptoms is key for catching it early and managing it well.
Common Early Symptoms
Early signs of MDS include fatigue, weakness, and shortness of breath. These are mainly because of anemia. These symptoms can be hard to spot because they’re similar to other health issues.
Pallor, or paleness, is another early sign, also tied to anemia. People might also feel dizziness or lightheadedness because of not enough red blood cells.
Advanced Symptoms
As MDS gets worse, symptoms get more serious. This includes infections because the immune system is weak, bleeding or bruising easily from low platelet counts, and weight loss.
Advanced MDS can lead to severe anemia needing frequent blood transfusions. It also raises the risk of deadly infections.
Symptom Variations by MDS Type
The symptoms of MDS can change based on the subtype and how severe it is. For example, some types of MDS cause more anemia or thrombocytopenia (low platelet count).
| MDS Subtype | Common Symptoms |
| Low-Risk MDS | Fatigue, weakness, shortness of breath |
| High-Risk MDS | Infections, bleeding, weight loss |
This highlights the significance of understanding this pre-cancerous blood condition.
Diagnosing Myelodysplastic Syndrome
Diagnosing MDS is complex. It involves blood tests and bone marrow exams. Getting it right is key to the right treatment.
Blood Tests and Complete Blood Count
Blood tests start the MDS diagnosis. A Complete Blood Count (CBC) checks blood cell levels. This includes red, white blood cells, and platelets. If these levels are off, it might be MDS.
- Red Blood Cell Count
- White Blood Cell Count
- Platelet Count
- Hemoglobin and Hematocrit levels
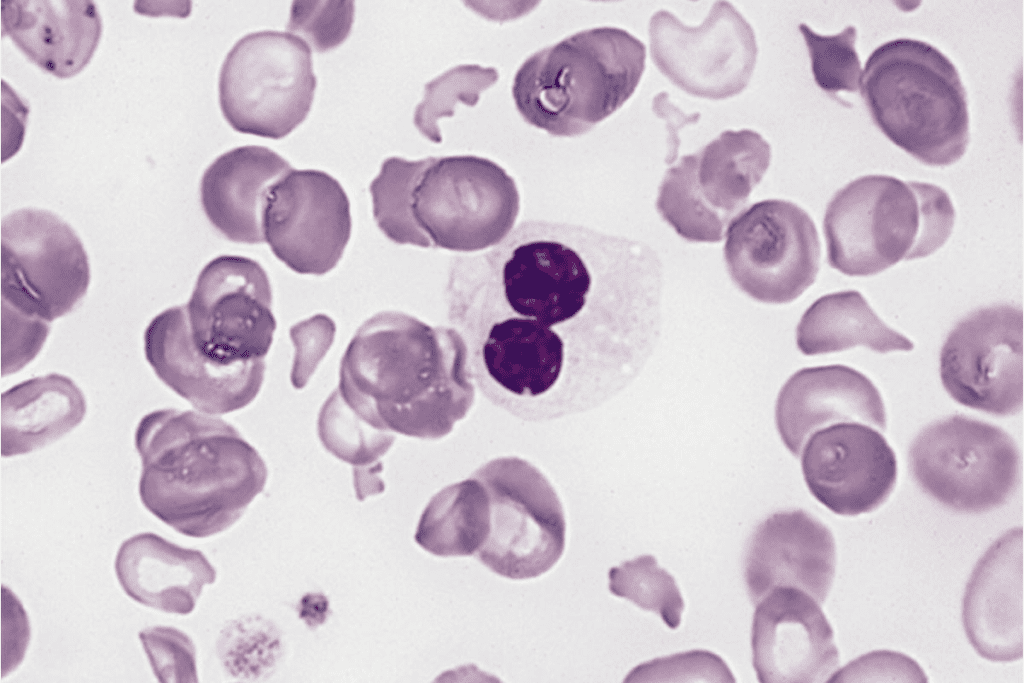
Bone Marrow Biopsy and Aspiration
A bone marrow biopsy and aspiration are key. They remove bone marrow for a closer look. The biopsy shows cell details and morphology, spotting MDS signs.
Cytogenetic Testing
This highlights the significance of understanding this pre-cancerous blood condition.
Molecular and Genetic Testing
Molecular and genetic tests find specific MDS mutations. They offer insights into the disease’s outlook and help choose treatments.
Healthcare teams use these tests together. They accurately diagnose MDS and plan the best treatment.
Differential Diagnosis of Blood Disorders
Diagnosing Myelodysplastic Syndrome (MDS) needs a detailed approach. It’s important to tell it apart from other blood disorders. Getting the diagnosis right is key to choosing the right treatment.
Distinguishing MDS from Other Anemias
MDS often shows up as anemia, making it hard to tell apart from other anemias. A key difference is the presence of dysplastic changes in bone marrow cells of MDS patients.
To diagnose, doctors look closely at blood cell shape and bone marrow samples. They also do genetic tests to find MDS-specific genetic changes.
Overlap with Myeloproliferative Neoplasms
MDS can look like myeloproliferative neoplasms (MPNs), making diagnosis tricky. Some patients show traits of both, known as MDS/MPN overlap syndromes.
| Characteristics | MDS | MPNs |
| Primary Feature | Dysplasia in one or more cell lines | Proliferation of one or more cell lines |
| Cytogenetic Abnormalities | Common, often complex | Less common, often simple (e.g., JAK2 mutation) |
| Risk of Leukemic Transformation | High, in high-risk MDS | Varies by MPN subtype |
Distinguishing from Acute Leukemia
Telling MDS apart from acute leukemia, like Acute Myeloid Leukemia (AML), is vital. AML has more blasts in the bone marrow or blood.
Diagnosing MDS involves clinical checks, blood tests, bone marrow exams, and genetic tests. Getting it right means patients get the right treatment.
MDS Classification Systems
Understanding MDS classification systems is key for predicting outcomes and treatment plans. Several systems categorize MDS, each highlighting different aspects of the disease.
WHO Classification
The World Health Organization (WHO) system is a top choice for MDS categorization. It looks at bone marrow blasts, genetic changes, and more. This helps in understanding the disease’s severity and predicting patient outcomes.
International Prognostic Scoring System (IPSS)
The International Prognostic Scoring System (IPSS) is vital for MDS assessment. It considers bone marrow blasts, karyotype, and cytopenias to predict prognosis. The IPSS groups patients by risk, aiding in treatment planning.
Revised IPSS (IPSS-R)
The Revised IPSS (IPSS-R) updates the IPSS with more detailed cytogenetic data and a refined blast assessment. It offers a more precise prognosis, helping tailor treatments to each patient.
WHO Prognostic Scoring System (WPSS)
The WHO Prognostic Scoring System (WPSS) combines WHO classification with other factors. It offers a detailed prognosis, guiding treatment choices. The WPSS is great for assessing AML risk.
In summary, MDS classification and prognostic systems are vital for disease management. They provide essential information on disease characteristics, prognosis, and guide treatment decisions, improving patient outcomes.
Treatment Options for Myelodysplastic Syndrome
This highlights the significance of understanding this pre-cancerous blood condition.
Supportive Care Treatments
Supportive care is key in managing MDS. It aims to ease symptoms and improve your life quality. This includes:
- Blood transfusions to address anemia and reduce fatigue
- Antibiotics to treat infections
- Growth factors to stimulate the production of blood cells
Growth Factors
Growth factors are proteins that help your bone marrow make more blood cells. They can cut down on the need for blood transfusions and help with symptoms.
Disease-Modifying Medications
Some patients might need disease-modifying medications. These include:
- Immunomodulatory drugs
- Hypomethylating agents
- Other targeted therapies
Stem Cell Transplantation
Stem cell transplantation is a possible cure for MDS. It replaces your diseased bone marrow with healthy stem cells from a donor.
Choosing stem cell transplantation depends on many things. These include your age, health, and the details of your MDS.
| Treatment Option | Description | Potential Benefits |
| Supportive Care | Manages symptoms and improves quality of life | Reduces fatigue, infection risk |
| Growth Factors | Stimulates production of blood cells | Reduces need for blood transfusions |
| Disease-Modifying Medications | Targets underlying disease processes | May improve blood counts, delay progression |
| Stem Cell Transplantation | Replaces diseased bone marrow with healthy cells | Potential cure, improved survival |
The Relationship Between MDS and Leukemia

MDS, often called “pre-leukemia,” can turn into acute myeloid leukemia (AML). It’s key to know the risks and how to watch for changes in MDS patients.
MDS as “Pre-Leukemia”
The term “pre-leukemia” for MDS shows its risk of becoming leukemia. MDS means the bone marrow can’t make healthy blood cells. This problem can get worse over time.
Transformation to Acute Myeloid Leukemia (AML)
Patients with MDS face a big risk of turning into AML. AML starts in the bone marrow and quickly spreads into the blood. It grows fast and needs quick treatment.
AML happens when bone marrow cells get genetic changes. This leads to too many immature white blood cells. This can take months or years, based on several factors.
Risk Factors for Progression
Some things make MDS more likely to turn into AML. These include:
- Genetic changes in bone marrow cells
- More blast cells in the bone marrow
- Chemotherapy or radiation therapy before
- High-risk MDS subtypes
Monitoring for Leukemic Transformation
It’s important for MDS patients to get checked often. This helps catch any signs of AML early. This includes:
- Regular blood tests for cell count changes
- Bone marrow biopsies to check blast cells
- Genetic tests to find changes
Finding AML early can help with treatment choices and results.
Prognosis and Life Expectancy with MDS
The outlook for MDS patients varies a lot. This depends on the type of MDS and the patient’s health. Knowing these factors helps patients and their families make better choices about treatment and care.
Prognostic Factors
Several things can affect how well a patient with MDS will do. These include:
- Subtype of MDS: Different types have different outlooks.
- Patient’s Age: Older patients usually face a tougher time.
- Cytogenetic Abnormalities: Some genetic issues can change the outlook.
- Blood Cell Counts: The levels of blood cells also play a role.
Survival Rates by Risk Group
Doctors often group MDS patients by how likely they are to do well. The International Prognostic Scoring System (IPSS) is a common way to do this.
| Risk Category | Median Survival (Years) |
| Low | 5.7 |
| Intermediate-1 | 3.5 |
| Intermediate-2 | 1.2 |
| High | 0.4 |
These survival rates come from the IPSS. They give a general idea of what to expect.
Quality of Life Considerations
While knowing the prognosis is important, living well is just as key for MDS patients. Things that affect how well a patient lives include:
- Fatigue: A common symptom that can really affect daily life.
- Infection Risk: Patients with MDS are more likely to get sick.
- Treatment Side Effects: Managing these side effects is key to a good quality of life.
Impact of Treatment on Prognosis
Treatment can really change the outlook for MDS patients. Options range from just managing symptoms to more aggressive treatments like stem cell transplants. This depends on how sick the patient is and the type of MDS they have.
Supportive care aims to improve symptoms and quality of life. Disease-modifying treatments try to change the course of the disease.
Living with Myelodysplastic Syndrome
Living with MDS means understanding the condition and finding ways to deal with it. Patients and their caregivers face many challenges. These include managing symptoms and finding emotional support.
Managing Fatigue and Daily Activities
Fatigue is a big problem for MDS patients. It affects their quality of life a lot. Effective management strategies include:
- Pacing activities to conserve energy
- Prioritizing tasks based on importance and urgency
- Engaging in regular, gentle exercise to maintain physical function
Changing daily routines and getting support can also help fight fatigue.
Infection Prevention Strategies
Infections are a big risk for MDS patients because their immune systems are weak. Prevention is key, and strategies include:
- Avoiding close contact with individuals who are sick
- Practicing good hygiene, such as frequent handwashing
- Staying up-to-date with recommended vaccinations
By avoiding infections, patients can lower their risk of serious problems.
Nutritional Considerations
Eating well is very important for MDS patients. It helps them stay strong and healthy. Nutritional considerations include:
- Consuming a variety of foods rich in essential nutrients
- Avoiding foods that may pose an infection risk, such as undercooked meats or unpasteurized dairy products
- Staying hydrated by drinking plenty of fluids
Getting advice from healthcare providers or a registered dietitian can help make a good diet plan.
Emotional and Psychological Support
Living with MDS can really affect a person’s emotions and mind. Support systems are very important. They may include:
- Counseling or therapy to address anxiety, depression, or stress
- Support groups for connecting with others who understand the challenges of MDS
- Family and friends who can provide emotional support and practical assistance
Using these resources can really help patients deal with their condition better.
Monitoring and Follow-up Care
Monitoring and follow-up care are key for MDS patients. They help manage Myelodysplastic Syndrome (MDS) effectively. Regular checks and treatment plan adjustments are essential.
Regular Blood Tests
Regular blood tests are vital for MDS management. They track blood cell counts, spotting any issues or changes. This helps see how the disease is progressing or how well treatment is working.
Key components of regular blood tests include:
- Complete Blood Count (CBC) to assess red blood cell, white blood cell, and platelet counts
- Peripheral blood smear to examine the morphology of blood cells
- Monitoring for signs of anemia, infection, or bleeding disorders
Bone Marrow Examinations
Bone marrow exams, like biopsies and aspirations, are critical. They check the bone marrow’s health and MDS progression. These tests reveal cell count, abnormal cells, and genetic issues.
| Procedure | Purpose | Information Gained |
| Bone Marrow Biopsy | Assess bone marrow cellularity and structure | Presence of fibrosis, cellularity, and architecture |
| Bone Marrow Aspiration | Analyze bone marrow cells for abnormalities | Cytogenetic and molecular abnormalities, blast count |
Managing Treatment Side Effects
It’s important to manage MDS treatment side effects. Common issues include fatigue, infection risk, and blood problems.
Strategies for managing treatment side effects:
- Adjusting medication dosages or switching to alternative treatments
- Implementing supportive care measures such as transfusions or growth factors
- Monitoring for signs of infection and initiating prompt treatment when necessary
When to Consider Treatment Changes
Treatment plans for MDS should be flexible. Changes are needed if the disease worsens, side effects are severe, or treatment isn’t working.
By staying vigilant with monitoring and follow-up, healthcare providers can improve MDS treatment. This leads to better outcomes and quality of life for patients.
Latest Research and Clinical Trials
Ongoing clinical trials are key in the fight against Myelodysplastic Syndrome. They bring new hope and treatment options to patients.
Emerging Treatments
New treatments for Myelodysplastic Syndrome are being tested. These include drugs and new ways to treat the disease. They aim to boost blood cell production and prevent the disease from getting worse.
- Immunotherapy: Using the body’s immune system to fight MDS.
- Targeted Therapy: Drugs that target specific genetic mutations in MDS.
- Stem Cell Transplantation: New transplant techniques are improving outcomes for some patients.
Genetic Research Advances
Genetic research has greatly improved our understanding of Myelodysplastic Syndrome. It helps identify genetic mutations, leading to targeted treatments.
Some important areas of genetic research include:
- Identifying genetic markers to predict disease progression.
- Understanding how genetic mutations cause MDS.
- Creating genetic tests to help choose treatments.
Participating in Clinical Trials
Joining clinical trials can give patients access to new treatments. It also helps advance medical research and future treatments.
Patients should talk to their doctors about the benefits and risks of clinical trials. This helps them make a well-informed decision.
Conclusion
This highlights the significance of understanding this pre-cancerous blood condition.
Managing MDS involves different strategies. These include supportive care, disease-modifying medications, and stem cell transplantation. By keeping up with the latest research and clinical trials, those with MDS can find new treatment options. This helps them make informed decisions about their care.
As research advances, the outlook for MDS patients is getting better. With a team effort in care and a focus on the latest developments, patients can manage this challenging condition. This way, they can improve their overall well-being.
FAQ
What is Myelodysplastic Syndrome (MDS)?
Myelodysplastic Syndrome (MDS) is a serious condition. It affects how blood cells are made in the bone marrow.
What are the common symptoms of MDS?
Early signs of MDS include feeling very tired, weak, and short of breath. As it gets worse, symptoms can include infections, bleeding, and losing weight.
How is MDS diagnosed?
Doctors use blood tests, bone marrow biopsies, and genetic tests to diagnose MDS. These include a complete blood count (CBC) and bone marrow aspiration.
What are the different types of MDS?
MDS has different subtypes. These are based on the number of bone marrow blasts, genetic changes, and blood cell shortages.
What are the causes and risk factors of MDS?
The exact causes of MDS are not always known. But, certain chemicals, radiation, and genetic changes can increase the risk.
How is MDS treated?
Treatment for MDS depends on the type, how severe it is, and the patient’s health. It may include supportive care, medications, and stem cell transplants.
Can MDS progress to leukemia?
Yes, MDS can turn into acute myeloid leukemia (AML). Knowing the risk factors is important for managing MDS.
What is the prognosis for MDS?
The outlook for MDS varies. It depends on the type, severity, and overall health. Understanding these factors helps in making decisions.
How can patients manage MDS symptoms and improve quality of life?
Managing MDS symptoms is key to a better life. This includes managing fatigue, preventing infections, and getting emotional support.
What is the role of ongoing research and clinical trials in MDS?
Research and clinical trials are vital for MDS. They help find new treatments and improve patient outcomes.
References
Rafiq, M., et al. (2024). Predictive value of abnormal blood tests for detecting cancer in symptomatic patients: A cohort study in primary care. PLoS Medicine. Retrieved from
Virdee, P. S., et al. (2024). The association between blood test trends and undiagnosed cancer: A population-based study. BMC Medicine. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11083147/