Last Updated on October 21, 2025 by mcelik
Did you know that blood clotting saves millions of lives every year? It stops too much bleeding when a blood vessel gets hurt.
But, if clotting goes wrong, it can cause big health problems. We’ll look into what coagulation is, why it’s important, and what happens when it doesn’t work right.
Coagulation, or clotting and coagulation, is key to our health. Understanding how coagulation works assists healthcare professionals in identifying and addressing issues effectively. We’ll see why coagulation matters for our well-being.
Key Takeaways
- Dysregulation of coagulation can lead to serious health issues.
- Understanding coagulation is critical for diagnosing and treating related disorders.
- Coagulation disorders can have significant consequences on overall health.
- Proper diagnosis and treatment of coagulation disorders are essential.
The Fundamentals of Blood Coagulation

Blood coagulation is a defense against too much blood loss. It’s a complex process. Many cells and proteins work together to keep blood vessels strong.
Coagulation, or clotting, turns blood from liquid to gel. This is key to stop bleeding when a blood vessel is hurt. Platelets stick together and fibrin, a protein, forms the clot.
The coagulation cascade is a series of chemical reactions. It leads to clot formation. Clotting factors, proteins in blood plasma, are involved. They are labeled with Roman numerals (I to XIII) and work in a specific order.
The Physiological Purpose of Blood Clotting
The main goal of blood clotting is to stop too much blood loss after a vessel is injured. It seals off the damaged area. This keeps blood pressure stable and ensures the affected area gets enough blood.
Blood clotting also helps in healing. The clot supports cell growth and repair. As healing happens, the clot is broken down by fibrinolysis. This process helps blood flow return to normal.
| Clotting Factor | Name | |
| I | Fibrinogen | Forms fibrin clot |
| II | Prothrombin | Precursor to thrombin |
| III | Tissue Factor |
Understanding how coagulation works assists healthcare professionals in identifying and addressing issues effectively.
The Coagulation Cascade: How Blood Clots Form
When a blood vessel gets hurt, the body starts the coagulation cascade to stop too much bleeding. This complex process has many steps that end in a blood clot. It’s key for keeping blood inside our bodies and stopping bleeding too much.
Primary Hemostasis: Platelet Activation
The first step is primary hemostasis, where platelets get activated. When a blood vessel is damaged, platelets stick to the injury and clump together. This is helped by von Willebrand factor and collagen. The platelet plug seals the injured vessel.
Platelet activation is very important. Activated platelets release chemicals that bring more platelets to the injury. This makes a strong platelet plug that seals the blood vessel.
Secondary Hemostasis: Fibrin Formation
The coagulation cascade involves many clotting factors, proteins in our blood. These factors, named with Roman numerals, work together to make fibrin. The last step is when fibrinogen turns into fibrin by thrombin.
| Clotting Factor | Common Name | |
| Factor I | Fibrinogen | Precursor to fibrin |
| Factor II | Prothrombin | Precursor to thrombin |
| Factor IIa | Thrombin | Converts fibrinogen to fibrin |
Understanding how coagulation works assists healthcare professionals in identifying and addressing issues effectively.
Normal vs. Abnormal Clotting and Coagulation
It’s important to know the difference between normal and abnormal clotting. This helps us understand coagulation disorders better. We’ll look at how healthy people keep their clotting in check and what happens when it goes wrong.
Balanced Hemostasis in Healthy Individuals
In healthy people, clotting is a finely tuned process. It stops bleeding without causing too many clots. This balance comes from pro-coagulant and anti-coagulant factors working together.
When Coagulation Goes Wrong
When this balance is upset, it can cause coagulation disorders. These can make it hard to stop bleeding or lead to too many clots (thrombosis).
| Condition | Description | Potential Complications |
| Normal Hemostasis | Balanced clotting and bleeding prevention | None under normal conditions |
| Hypercoagulable State | Increased tendency to form clots | Deep Vein Thrombosis, Pulmonary Embolism |
| Coagulopathy | Increased tendency to bleed | Hemorrhage, Easy Bruising |
The effects of coagulation disorders can be serious. They range from deep vein thrombosis and pulmonary embolism to bleeding and easy bruising. Knowing about these conditions is key to managing and treating them.
Hypercoagulation: When Blood Clots Too Easily
Hypercoagulation is when blood clots too quickly. This can harm your health a lot. It happens when your blood clots too fast, causing blockages in blood flow.
Defining Hypercoagulable States
A hypercoagulable state means your blood clots too easily. Thrombophilia is another name for this. It’s when you’re more likely to get blood clots because of your genes or other health issues.
“Having a hypercoagulable state raises your risk of serious blood clots,” says a top expert in hematology.
Risk Factors for Hypercoagulation
Many things can make you more likely to have hypercoagulation. Genetic factors include certain gene mutations, like Factor V Leiden.
- Having conditions like cancer or hormonal changes can also raise your risk.
- Other health issues, like kidney problems or certain blood cancers, can make you more prone to clotting.
- Things like not moving much, smoking, or being overweight can also increase your risk.
Knowing about these risk factors helps doctors catch hypercoagulation early. They can then take steps to prevent serious blood clots.
Common Causes of Blood Thickening
Blood clotting too much is called hypercoagulability. It comes from genes and things we get from outside. Knowing why it happens helps us treat it better.
Hypercoagulability is caused by many things. Genes and health conditions both play a big part. They affect how blood clots.
Genetic Factors in Blood Coagulability
Genes can change how blood clots. Some genes make clotting factors work differently. This can increase the risk of blood clots.
- Factor V Leiden: A mutation that makes factor V resistant to inactivation by activated protein C, leading to an increased risk of clot formation.
- Prothrombin Gene Mutation: This mutation can lead to elevated levels of prothrombin, increasing the risk of thrombosis.
- Antithrombin Deficiency: A condition where the body lacks sufficient antithrombin, a protein that helps regulate clotting.
These genetic factors can be passed down. People with a family history of blood clots might have them.
Acquired Causes of Thick Blood
Many things can make blood clot more. Medical conditions, lifestyle, and medicines are some. Here are a few examples:
- Cancer: Some cancers make blood clot more because they produce substances that help clots form.
- Immobility: Being stuck in one place for a long time, like on a long flight, can cause blood to clot.
- Hormonal Changes: Hormone changes, like during pregnancy or after having a baby, can also make blood clot more.
Other conditions like antiphospholipid syndrome and myeloproliferative neoplasms can also make blood clot more.
Recognizing the Symptoms of Coagulation Disorders
Knowing the symptoms of coagulation disorders can save lives. Disorders like hypercoagulation can cause serious health problems if not treated quickly.
Warning Signs of Hypercoagulation
Hypercoagulation shows itself in different ways. Some common signs include:
- Pain or swelling in the limbs
- Redness or warmth in the affected area
- Unexplained swelling or tenderness
When to Seek Medical Attention
If you notice any of these symptoms, get medical help right away:
- Severe pain or swelling in one limb
- Chest pain or trouble breathing
- Neurological symptoms like confusion or weakness
Quick medical check-ups can stop serious problems like deep vein thrombosis (DVT) or pulmonary embolism (PE). A study shows that early action can cut the risk of lasting damage by half.
We stress the need to know the symptoms of coagulation disorders and when to get medical help. This knowledge can greatly improve health outcomes and lower the risk of complications.
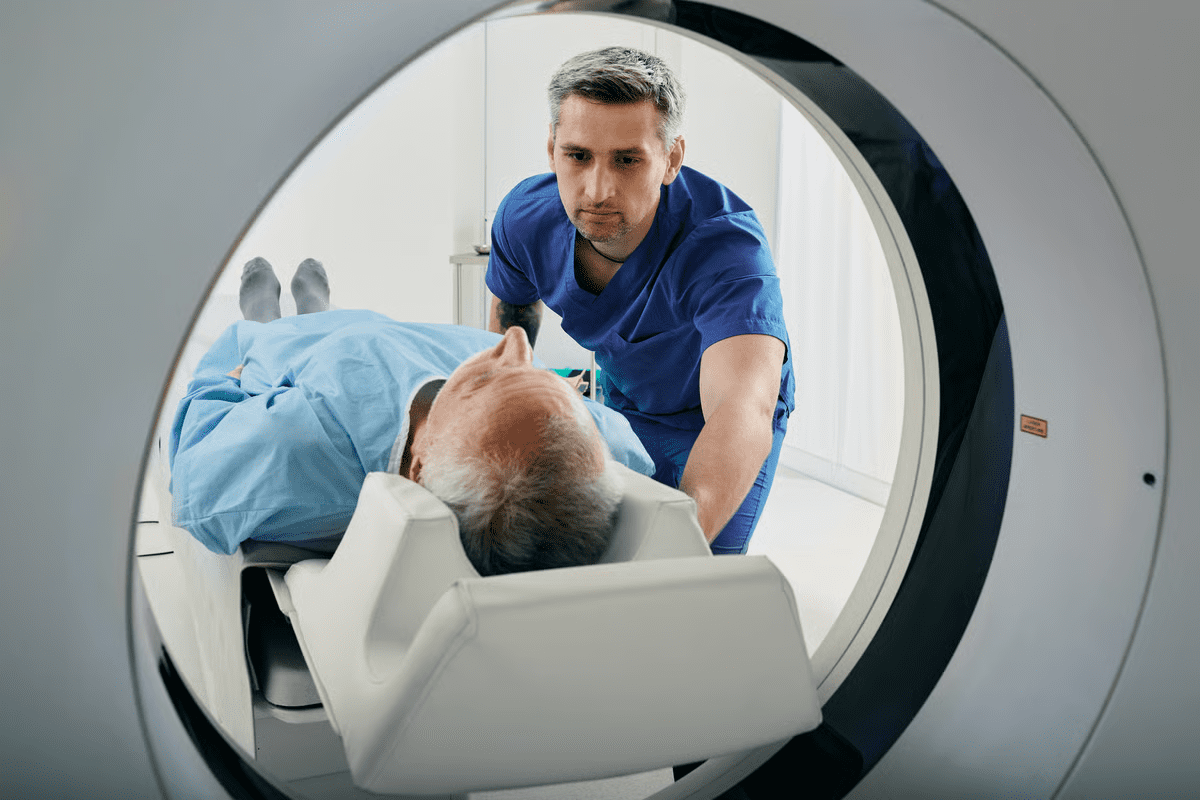
Diagnosing Coagulation Abnormalities
Diagnosing coagulation problems involves lab tests and imaging studies. These tools help find clotting issues and guide treatment.
Laboratory tests are key in checking blood clotting. We use different assays to measure the coagulation cascade’s parts.
Laboratory Tests for Blood Clotting Assessment
Laboratory tests are vital for spotting coagulation problems. These include:
- Clotting time assays, like prothrombin time (PT) and activated partial thromboplastin time (aPTT), which show how long it takes for blood to clot.
- Clotting factor analyses, which check the levels and activity of clotting factors in the blood.
- Fibrinogen level tests, which measure fibrinogen, a key protein in clotting.
These tests help us find the cause of coagulation disorders and see if treatment is working.
Imaging Studies for Clot Detection
Imaging studies also help find and check blood clots. Common ones are:
- Ultrasound, often used for deep vein thrombosis (DVT).
- Computed Tomography (CT) scans, which spot clots in places like the lungs and brain.
- Magnetic Resonance Imaging (MRI), which gives detailed views of blood vessels and clots.
By using lab tests and imaging, we can accurately find coagulation problems. Then, we can make good treatment plans.
Thrombophilia: Understanding Blood Clotting Disorders
Thrombophilia is a condition where blood clots more easily. It’s a serious health issue that can be managed with the right care. It can be passed down in families or caused by other factors.
Inherited Thrombophilias
Inherited thrombophilias are genetic conditions that affect blood clotting. They are passed down through families. These conditions raise the risk of blood clots.
People with a family history of blood clots or who have had them before might need tests. Knowing the genetic causes helps in managing the condition.
Acquired Thrombophilic Conditions
Acquired thrombophilic conditions are not inherited. They develop over time due to various reasons. Medical conditions, infections, and lifestyle choices can cause them.
For example, being immobile for a long time, surgery, and some medications can increase the risk. Knowing these risks helps prevent blood clots.
Managing thrombophilia requires a complete approach. This includes medical treatments and lifestyle changes. Understanding the causes helps in creating a treatment plan tailored to each person.
Serious Complications of Abnormal Coagulation
It’s important to know the risks of abnormal coagulation to avoid serious health problems. This issue can cause life-threatening heart and blood vessel problems.
Abnormal coagulation means the body either makes too many or too few blood clots. Too many clots can block blood flow, while too few can cause too much bleeding.
Deep Vein Thrombosis and Pulmonary Embolism
One big risk is deep vein thrombosis (DVT). DVT happens when a blood clot forms in deep veins, often in the legs. If not treated, it can turn into a deadly pulmonary embolism (PE), where the clot goes to the lungs.
Symptoms of DVT include swelling, pain, and redness in the affected limb. PE can cause shortness of breath, chest pain, and even sudden death.
Stroke and Heart Attack Risk
Abnormal coagulation also raises the risk of stroke and heart attack. Blood clots in brain or heart arteries can block them, causing damage or death.
The risk factors for these conditions include genetics, lifestyle, and health conditions. Knowing these risks helps prevent and treat them early.
The following table summarizes the serious complications associated with abnormal coagulation:
| Complication | Description | Symptoms |
| Deep Vein Thrombosis (DVT) | Blood clot in deep veins, usually in the legs | Swelling, pain, redness in the affected limb |
| Pulmonary Embolism (PE) | Clot breaks loose and travels to the lungs | Shortness of breath, chest pain, sudden death |
| Stroke | Blockage in arteries supplying the brain | Slurred speech, weakness, vision loss |
| Heart Attack | Blockage in arteries supplying the heart | Chest pain, shortness of breath, fatigue |
Treatment Approaches for Coagulation Disorders
Treating coagulation disorders involves both medicine and surgery. It’s important to know all the options for managing these conditions.
Anticoagulant Medications
Anticoagulant drugs are key in treating coagulation disorders. They stop new blood clots from forming and prevent existing ones from growing. We use these drugs for people at risk of blood clots or those who have already had one.
Medicines like warfarin, apixaban, rivaroxaban, and dabigatran are common choices. Each has its own use, benefits, and side effects.
Choosing the right anticoagulant depends on the patient’s health history and the cause of their disorder. We also consider any other health issues they might have. Regular checks are needed to make sure these treatments work well and are safe.
Surgical Interventions for Blood Clots
Sometimes, surgery is needed to treat coagulation disorders. Procedures like thrombectomy, which removes blood clots, are used in emergencies. We also consider IVC filters for patients who can’t take anticoagulants or have clots despite treatment.
Surgery is usually for severe cases or when other treatments don’t work. We decide on surgery based on the patient’s health and their specific disorder.
Knowing all the treatment options helps doctors create plans that meet each patient’s needs. This way, we can better manage coagulation disorders.
Lifestyle Modifications to Manage Coagulation Issues
Living a healthy lifestyle is key for those with coagulation issues. It helps lower the risk of blood clots. Making smart choices about what you eat and how you exercise can greatly improve your blood vessel health.
Dietary Considerations for Healthy Blood Flow
Eating right is vital for keeping blood flowing well and preventing clots. Drinking plenty of water is essential. It keeps blood vessels flexible and blood flowing smoothly.
Some foods are better than others for blood clotting. Foods rich in omega-3 fatty acids, like salmon and flaxseeds, reduce inflammation and improve blood vessel function. Foods high in antioxidants, such as berries and leafy greens, protect against oxidative stress that may lead to clotting.
| Food Group | Beneficial Foods | Effect on Blood Flow |
| Fatty Fish | Salmon, Sardines | Reduces inflammation, improves vessel function |
| Nuts and Seeds | Flaxseeds, Chia Seeds | Rich in omega-3 fatty acids, anti-inflammatory |
| Fruits and Vegetables | Berries, Leafy Greens | High in antioxidants, protects against oxidative stress |
Exercise and Activity Recommendations
Regular exercise is also vital for managing coagulation issues. It boosts blood circulation, lowers clot risk, and improves heart health. Aim for at least 30 minutes of moderate-intensity exercise most days.
Brisk walking, cycling, or swimming are great options. Avoid sitting for long periods, as it can increase clot risk. For those with mobility issues, simple leg exercises or stretching can help.
By adding these lifestyle changes to your daily life, you can manage your coagulation issues better. This reduces the chance of serious problems.
Preventing Dangerous Blood Clots
Keeping our blood vessels healthy is key to avoiding dangerous blood clots. We can lower the risk of clots by following good health habits. It’s also important to know how to protect those at higher risk.
Risk Reduction Strategies
Living a healthy lifestyle is the first step in preventing blood clots. This means staying active, eating well, and not sitting for too long. Drinking plenty of water is also important because dehydration can make blood more likely to clot.
People at risk or with clotting history should see their doctor often. Doctors may check blood tests to see how well treatments are working.
| Risk Factor | Prevention Strategy |
| Prolonged Immobility | Regular movement, compression stockings |
| Family History of Clots | Genetic testing, anticoagulant therapy |
| Obesity | Weight loss, regular exercise |
Special Considerations for High-Risk Individuals
Those with clotting history or certain health issues are at higher risk. For them, anticoagulant medications might be needed to stop clots. It’s important to follow the treatment plan and keep doctor’s appointments.
High-risk people should watch for clot signs like swelling, pain, or color changes in limbs. If these symptoms show up, they should get medical help right away.
Living with Coagulation Disorders: Long-term Management
Managing coagulation disorders long-term is key to a good life. People with these conditions face a tough healthcare world. They must avoid problems and stay healthy.
Monitoring and Follow-up Care
Keeping an eye on things is vital. This means regular blood tests to check clotting factors. Doctors might also use imaging studies to watch for clots or other issues.
Follow-up care is just as important. It lets doctors see if treatments are working. Patients should talk about any changes or worries during these visits.
| Monitoring Activity | Frequency | Purpose |
| Blood Tests | Every 1-3 months | Assess clotting factors and adjust anticoagulant medication |
| Imaging Studies | As recommended by healthcare provider | Monitor for clots or other complications |
| Follow-up Appointments | Every 3-6 months | Assess treatment effectiveness and address patient concerns |
Quality of Life Considerations
Making lifestyle changes is important. This includes dietary changes and regular exercise. It’s also wise to avoid risky activities.
Staying informed about your condition is also key. Knowing your treatment options helps you make better choices. This improves your life quality.
By focusing on long-term care and smart lifestyle choices, people with coagulation disorders can live well. Our healthcare team is here to support you. We offer full care and advice to enhance your life quality.
Conclusion: The Importance of Understanding Coagulation Health
Understanding how coagulation works assists healthcare professionals in identifying and addressing issues effectively.
Coagulation disorders can lead to serious issues like deep vein thrombosis and heart attacks. It’s important to know the risks and symptoms. This way, people can get medical help on time.
Managing coagulation disorders needs a full plan. This includes changing lifestyle habits, taking medicines, and sometimes surgery. Working with doctors helps create a treatment plan that fits each person’s needs.
Teaching people about coagulation health is vital for better health. We urge readers to learn about their coagulation health. If they notice any symptoms or concerns, they should see a doctor.
FAQ
What is coagulation, and why is it important?
Coagulation, or blood clotting, stops bleeding when a blood vessel is hurt. It’s key for healing and keeping blood inside our bodies.
How do blood clots form?
Blood clots form through primary and secondary hemostasis. First, platelets stick together. Then, the coagulation cascade makes fibrin, forming a clot.
What is hypercoagulation, and what are its risk factors?
Hypercoagulation makes blood clot too easily, raising the risk of blood clots. Genetic and medical conditions, plus lifestyle, can cause it.
What are the symptoms of coagulation disorders?
Symptoms include pain, swelling, and redness in limbs. Seeing a doctor is important if you notice these signs.
How are coagulation abnormalities diagnosed?
Tests like clotting time assays and imaging studies like ultrasound help diagnose. They check for clots and their size.
What is thrombophilia, and how is it managed?
Thrombophilia increases the risk of blood clots. Treatment includes medicines, lifestyle changes, and regular check-ups.
What are the complications of abnormal coagulation?
Abnormal coagulation can cause serious problems. These include deep vein thrombosis, pulmonary embolism, stroke, and heart attack.
How can coagulation disorders be treated?
Treatment includes medicines to stop clots and surgery to remove them. This helps manage the condition.
What lifestyle modifications can help manage coagulation issues?
Drinking water and eating foods that prevent clotting help. Regular exercise also lowers the risk of blood clots.
How can dangerous blood clots be prevented?
Prevention includes lifestyle changes and monitoring for those at high risk. This can include special care and measures.
What is involved in the long-term management of coagulation disorders?
Long-term care includes regular check-ups and managing quality of life. This helps people with clotting disorders live well.
References
Hematology Review – Physiology of Coagulation via NCBI