
Inherited bleeding disorders affect thousands worldwide. Hemophilia and von Willebrand disease are the most common. Hemophilia makes it hard for blood to clot, leading to long bleeding times. Von Willebrand disease happens when there’s not enough or a faulty von Willebrand factor, a key clotting protein.
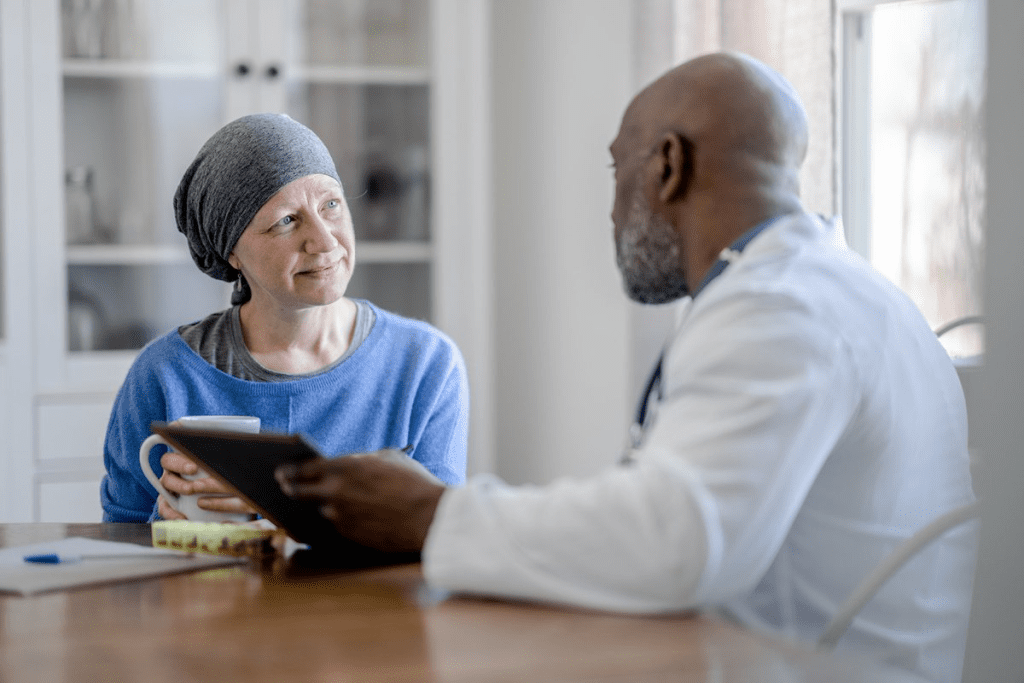
These conditions significantly impact the daily lives of those affected. They also put a big strain on healthcare systems. It’s important to understand inherited bleeding disorders to find better treatments and improve care.
Key Takeaways
- Hemophilia and von Willebrand disease are the most common inherited bleeding disorders.
- These conditions result from defects in blood clotting mechanisms.
- Effective management requires a thorough understanding of the disorders.
- Research and awareness are key to better treatment options.
- Healthcare systems face big challenges in managing these conditions.
Understanding the Mechanisms of Blood Clotting
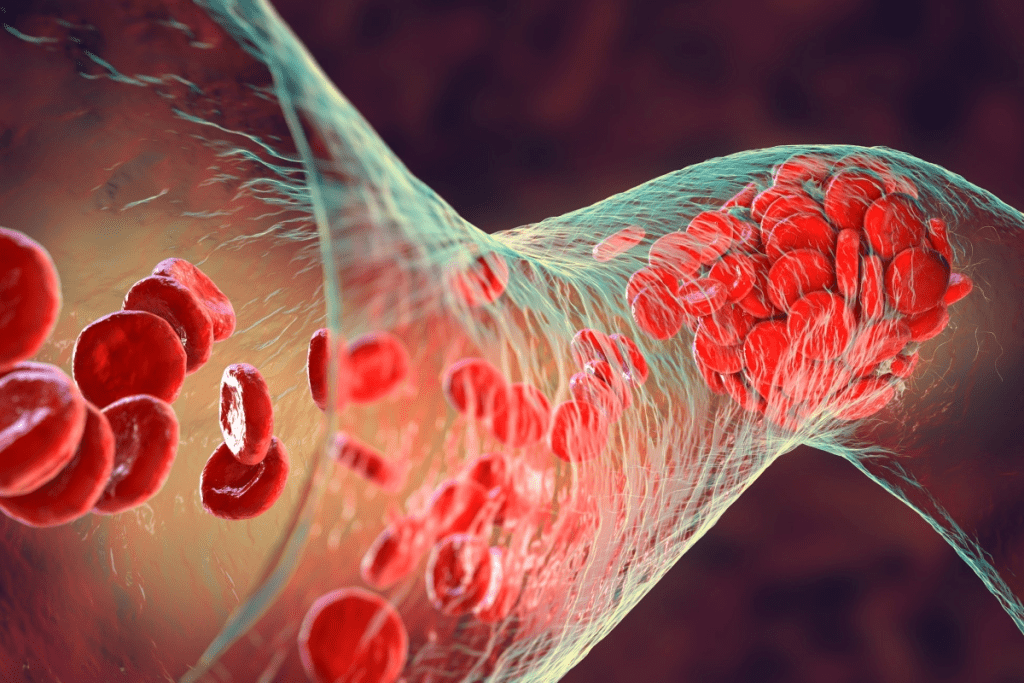
Hemostasis is how our body stops bleeding. It’s a balance between clotting and dissolving clots. This balance is key to prevent too much blood loss when a blood vessel gets hurt.
Normal Hemostasis Process
The normal process of stopping bleeding has several steps. First, vascular spasm happens. This is when the blood vessel walls contract to cut off blood flow to the injured area.
Then, platelet plug formation occurs. Platelets stick to the injury and to each other, creating a temporary seal. After that, the coagulation phase starts.
In this phase, chemical reactions create a fibrin clot. This clot strengthens the platelet plug. Clotting factors are proteins that help this process.
Role of Clotting Factors
Clotting factors are vital in the coagulation cascade. Each factor has its own role. Without them, bleeding disorders can occur.
Hemophilia A and B are caused by a lack of factor VIII and factor IX. These are key for the coagulation process.
- Factor VIII: Essential for the intrinsic pathway of coagulation.
- Factor IX: Also critical for the intrinsic pathway.
- Fibrinogen (Factor I): Converted into fibrin to form the clot.
What Happens When Clotting Is Impaired
Impaired clotting can cause bleeding disorders. These can stem from clotting factor deficiencies, platelet issues, or blood vessel problems. Knowing how blood clots work is key to diagnosing and treating these conditions.
Classification of Inherited Bleeding Disorders
Bleeding disorders that are inherited can be grouped into different types. This grouping is based on the parts of the blood clotting system they affect. Knowing these categories is key for diagnosing and treating these conditions.
Factor Deficiencies
Factor deficiencies happen when there’s not enough or when clotting factors don’t work right. Hemophilia A and B are examples. They are caused by a lack of factor VIII and IX, respectively.
Platelet Disorders
Platelet disorders involve problems with platelets. This can be a lack of platelets or when they don’t work well. Conditions like Bernard-Soulier syndrome and Glanzmann thrombasthenia show this.
Vascular Abnormalities
Vascular abnormalities are defects in blood vessels that can cause bleeding. Hereditary hemorrhagic telangiectasia (HHT) is a condition where blood vessels form abnormally.
| Category | Examples | Description |
| Factor Deficiencies | Hemophilia A, Hemophilia B | Lack or malfunction of clotting factors |
| Platelet Disorders | Bernard-Soulier syndrome, Glanzmann thrombasthenia | Abnormalities in platelet number or function |
| Vascular Abnormalities | Hereditary hemorrhagic telangiectasia (HHT) | Defects in blood vessel structure |
Hemophilia: The First Common Inherited Bleeding Disorder
Hemophilia is a group of bleeding disorders. They happen when certain clotting factors in the blood are missing. This makes it hard for blood to clot, leading to long and frequent bleeding.
Definition and Types of Hemophilia
Hemophilia is mainly split into two types: Hemophilia A and Hemophilia B. Hemophilia A is caused by a lack of factor VIII. Hemophilia B is due to a lack of factor IX. Both are genetic and affect blood clotting.
The World Federation of Hemophilia says Hemophilia A is more common. It affects about 1 in 5,000 to 1 in 10,000 males worldwide. Hemophilia B is rarer, happening in about 1 in 20,000 to 1 in 30,000 males.
Historical Perspective
Hemophilia has been known for centuries. Ancient civilizations mentioned it. The Talmud from the 2nd century talks about males who couldn’t be circumcised because of bleeding.
Prevalence and Demographics
Hemophilia mostly hits males because of its X-linked recessive pattern. Females can carry the mutated gene. They might show mild symptoms if they have two copies of the gene.
| Type of Hemophilia | Cause | Prevalence |
| Hemophilia A | Deficiency in Factor VIII | 1 in 5,000 to 1 in 10,000 males |
| Hemophilia B | Deficiency in Factor IX | 1 in 20,000 to 1 in 30,000 males |
Knowing about hemophilia helps manage it better. New medical treatments and genetic research offer hope. They improve life for those with hemophilia.
Genetic Basis of Hemophilia
Understanding the genetic roots of hemophilia is key to managing it well. Hemophilia is linked to the X chromosome.
X-Linked Inheritance Pattern
Hemophilia is X-linked recessive, meaning it’s on the X chromosome. This mainly affects males, who have one X and one Y chromosome. Females, with two X chromosomes, are usually carriers unless they get a bad gene from both parents, which is rare.
Mutations in Factor VIII and Factor IX Genes
The genes for clotting factor VIII and clotting factor IX are mutated in hemophilia A and B. These mutations cause the clotting factors to not work right. This leads to the bleeding problems seen in hemophilia.
Carrier Status and Testing
Female carriers have a 50% chance of passing the mutated gene to their sons, who will be affected, and daughters, who will likely become carriers. Genetic testing can spot carriers and those affected. This helps with family planning and managing the condition.
Knowing the genetic basis of hemophilia helps families and doctors manage it better.
Clinical Manifestations of Hemophilia
Hemophilia shows different symptoms, from mild to severe. This depends on how much clotting factor is missing. This makes it hard to diagnose and manage.
Symptoms Based on Severity
The severity of hemophilia is based on clotting factor levels. People with mild hemophilia might bleed after surgery or big injuries. Those with moderate hemophilia might bleed sometimes on their own.
But, those with severe hemophilia often bleed into joints and muscles a lot. This can happen without any injury.
Joint Bleeding and Hemarthrosis
Joint bleeding, or hemarthrosis, is a big problem for people with hemophilia. It can cause long-term pain, swelling, and make it hard to move. The knees, elbows, and ankles are most affected.
Chronic joint disease from too much bleeding can really hurt someone’s life. It makes simple tasks hard to do.
Muscle Bleeding and Other Complications
People with hemophilia can also bleed into muscles. Muscle hemorrhages are very painful. They can lead to serious problems like compartment syndrome, where muscle pressure hurts blood flow and nerves.
Other serious issues can happen too, like bleeding in the brain, stomach, or bladder. Quick and good treatment is key to avoid lasting harm and improve health.
Diagnosis and Screening for Hemophilia
Getting a correct diagnosis of hemophilia is key for managing it well. It involves different tests in labs and genetics. First, doctors look at your medical history and do a physical check to see if you bleed or bruise easily.
Laboratory Tests
Labs are important for finding out if you have hemophilia. They start with a blood count and tests like prothrombin time (PT) and activated partial thromboplastin time (aPTT). If aPTT is long, it might mean you lack a clotting factor.
Then, they do more tests to see how much of factor VIII and IX you have. These are key for diagnosing hemophilia A and B.
Genetic Testing
Genetic tests are also key in diagnosing hemophilia. They help find the exact genetic changes that cause it. This not only confirms the diagnosis but also helps find carriers in families.
Genetic tests are very useful for women who might carry the gene. They help with family planning and prepare for any affected children early on.
Prenatal Diagnosis
For families with a history of hemophilia, prenatal tests are available. Tests like chorionic villus sampling (CVS) or amniocentesis can check if the fetus has it. This gives important info for managing the pregnancy and preparing for the baby’s care.
In short, diagnosing hemophilia takes a few steps. It includes looking at your health, doing lab tests, and genetic testing. Early and right diagnosis is vital for managing hemophilia well. It helps improve life quality for those with this condition.
Treatment Options for Hemophilia
Managing hemophilia well means knowing all the treatment options. Over time, treatments for hemophilia have improved a lot. Now, there are many ways to handle the condition effectively.
Factor Replacement Therapy
Factor replacement therapy is key in treating hemophilia. It adds the missing clotting factor to the blood. This can be done with plasma-derived or recombinant factor concentrates. Recombinant factor products are safer because they have a lower risk of disease transmission.
“The introduction of recombinant factor VIII and IX has changed how we treat hemophilia A and B,” says a top hematologist. This method has greatly improved life for those with hemophilia.
Prophylactic vs. On-Demand Treatment
Treatment can be given regularly or as needed. Prophylactic treatment involves regular infusions to prevent bleeding. On-demand treatment stops bleeding when it happens.
- Prophylactic treatment lowers bleeding frequency and prevents joint damage.
- On-demand treatment is for acute bleeding episodes.
Novel Therapies and Gene Therapy
New treatments, like gene therapy, are showing great promise. Gene therapy tries to fix the problem by adding a working gene to the cells. Early trials have shown good results, with some patients getting normal factor levels.
As research goes on, the future of treating hemophilia looks bright. We might see even better and easier treatments soon.
Von Willebrand Disease: The Second Common Inherited Bleeding Disorder
Von Willebrand disease affects millions globally, making it the second most common inherited bleeding disorder. It occurs when there’s not enough or not enough of the right kind of von Willebrand factor (VWF). VWF is key for blood clotting.
Definition and Types
Von Willebrand disease has different types based on how much VWF is missing or not working right. Type 1 has a partial lack of VWF. Type 2 has a problem with how VWF works, and Type 3 has no VWF at all.
Historical Background
A doctor discovered this disease in 1926. He found it in a Finnish family from the Ã…land Islands. It was caused by a lack of VWF.
Epidemiology and Prevalence
About 1% of people have von Willebrand disease, but it might be more common because it’s often missed. It affects both men and women. Some studies say women might be more likely to be diagnosed, possibly because of childbirth or menstruation.
| Type | Description | Prevalence |
| Type 1 | Partial deficiency of VWF | Most common |
| Type 2 | Qualitative defect in VWF | Less common |
| Type 3 | Complete deficiency of VWF | Rare |
Genetic and Molecular Basis of Von Willebrand Disease
Understanding the molecular genetics of Von Willebrand disease is key to diagnosing and managing it. This condition is caused by a lack or malfunction of Von Willebrand factor (VWF). VWF is a vital protein for blood clotting.
Autosomal Inheritance Pattern
Von Willebrand disease follows an autosomal inheritance pattern. This means it can affect both males and females. It often follows an autosomal dominant pattern, but some cases may be recessive. This pattern affects how likely it is to pass the condition to children.
Von Willebrand Factor Structure and Function
The Von Willebrand factor is a large, multimeric glycoprotein. It’s essential for blood clotting. It helps platelets stick to injured blood vessels and protects factor VIII from breaking down too soon. The size of VWF matters for its effectiveness in platelet adhesion.
Genetic Mutations and Their Effects
Genetic mutations in the VWF gene can cause Von Willebrand disease. These mutations can lead to problems with VWF’s production, processing, or function. The type and location of the mutation can change how severe the disease is.
In summary, Von Willebrand disease is complex. It involves genetics, the structure and function of Von Willebrand factor, and the impact of genetic mutations. Knowing these details is vital for diagnosing and treating the disease.
Clinical Presentation of Von Willebrand Disease
Von Willebrand disease is the most common inherited bleeding disorder. It causes mucocutaneous bleeding and menorrhagia. These symptoms can greatly affect a person’s life quality.
Mucocutaneous Bleeding
Mucocutaneous bleeding is a key symptom of Von Willebrand disease. It shows as easy bruising, nosebleeds (epistaxis), and bleeding from the gums. How often and how severe these episodes are can differ a lot.
Menorrhagia in Women
Women with Von Willebrand disease often experience heavy menstrual bleeding, or menorrhagia. This can cause iron deficiency anemia and affect daily life. Menorrhagia is a common and early symptom for many women.
Severity Classification and Symptoms
The severity of Von Willebrand disease is based on Von Willebrand factor (VWF) activity and antigen levels. Symptoms can be mild, moderate, or severe. They include:
| Severity | VWF Activity Level | Common Symptoms |
| Mild | 30-50% | Occasional bruising, nosebleeds |
| Moderate | 10-30% | Frequent bruising, heavy menstrual bleeding |
| Severe | Frequent and severe bleeding episodes, including joint and muscle bleeding |
Knowing how Von Willebrand disease presents is key for diagnosis and treatment. Recognizing symptoms and their severity helps doctors create better treatment plans for each patient.
Diagnosing Von Willebrand Disease
Diagnosing Von Willebrand disease is a detailed process. It starts with initial screening and goes to laboratory evaluation and sometimes genetic testing. This thorough method is needed because the disease can show up differently in people.
Laboratory Evaluation
Laboratory tests are key in diagnosing Von Willebrand disease. The first step often includes a complete blood count (CBC) and bleeding time tests. More detailed tests are:
- VWF antigen (VWF:Ag) to measure the level of Von Willebrand factor
- VWF activity (VWF:Act) to assess the function of Von Willebrand factor
- Factor VIII activity to evaluate the level of factor VIII
These tests help understand how severe and what type of Von Willebrand disease someone has.
Challenges in Diagnosis
Diagnosing Von Willebrand disease can be tricky. This is because of several reasons, including:
- Variability in symptoms among affected individuals
- Overlap with other bleeding disorders
- Limited sensitivity and specificity of some laboratory tests
A detailed medical history and physical examination are key in guiding the diagnostic process.
Specialized Testing Methods
In some cases, specialized tests are needed to confirm the diagnosis or to tell the difference between types of Von Willebrand disease. These include:
| Test | Purpose |
| VWF multimer analysis | To assess the structure of Von Willebrand factor |
| Genetic testing | To identify mutations in the VWF gene |
| Ristocetin-induced platelet aggregation (RIPA) | To evaluate the function of Von Willebrand factor |
These specialized tests give important information. They help guide treatment decisions and manage the condition well.
Treatment Approaches for Von Willebrand Disease
Treatment for von Willebrand disease varies based on the individual’s needs and how severe their condition is. It often involves a mix of therapies to reduce bleeding risks and manage symptoms.
Desmopressin (DDAVP) Therapy
Desmopressin, or DDAVP, is a synthetic hormone for mild to moderate von Willebrand disease. It boosts the levels of von Willebrand factor and factor VIII in the blood. This helps fix the clotting factor shortage. DDAVP is best for those with type 1 von Willebrand disease.
Benefits of DDAVP Therapy:
- Works well for mild to moderate cases
- Easy to administer (intranasal or intravenous)
- Starts working quickly
Von Willebrand Factor Concentrates
For those not helped by DDAVP or with severe von Willebrand disease, concentrates are used. These products have both von Willebrand factor and factor VIII. They directly replace the missing clotting factors. They’re great for stopping bleeding quickly or before surgery.
| Therapy Type | Indications | Benefits |
| DDAVP Therapy | Mild to moderate von Willebrand disease | Rapid correction of clotting factors, non-invasive |
| Von Willebrand Factor Concentrates | Severe von Willebrand disease, acute bleeding, surgical prophylaxis | Direct replacement of deficient factors, effective for severe cases |
Adjunctive Therapies
Along with main treatments, other therapies support managing von Willebrand disease. These include antifibrinolytic agents to keep clots stable and hormonal treatments for heavy menstrual bleeding in women.
Choosing the right treatment for von Willebrand disease depends on several factors. These include how severe the condition is, how well the patient responds to treatments, and other personal factors. A doctor who specializes in bleeding disorders can help find the best treatment plan.
Managing Bleeding Disorders Across the Lifespan
Managing bleeding disorders at different life stages is key. It involves understanding and addressing unique needs. From diagnosing infants to caring for the elderly, a personalized approach is essential.
Pediatric Considerations
In children, diagnosing and managing bleeding disorders need extra care. Early diagnosis is vital to avoid complications. It also helps parents learn how to manage their child’s condition.
- Recognizing symptoms early
- Implementing appropriate treatment plans
- Educating caregivers and family members
Adolescence and Transition to Adult Care
As children with bleeding disorders grow up, their care must change. They need to start seeing adult healthcare providers. They also need to take more responsibility for their condition.
Pregnancy and Childbirth
Women with bleeding disorders face special challenges during pregnancy and childbirth. Close work between hematologists and obstetricians is key to reduce risks.
- Pre-pregnancy counseling
- Careful monitoring during pregnancy
- Planning for delivery
Aging with a Bleeding Disorder
As people with bleeding disorders get older, they may face more health issues. This includes joint damage or other health problems. A detailed and team-based approach is needed to manage these challenges.
Managing bleeding disorders at every stage of life is complex. Healthcare providers must adapt their care to meet each stage’s unique needs. This way, they can offer better care.
Emergency Management of Bleeding Disorders
Emergency situations with bleeding disorders need quick action to avoid serious problems. Conditions like hemophilia and von Willebrand disease can cause severe bleeding. This requires immediate care.
Recognizing Life-Threatening Bleeds
It’s key to spot life-threatening bleeds fast. These include severe bleeding from injuries, stomach bleeding, or bleeding in the brain. Catching these signs early can greatly improve results.
First Aid Measures
First aid for bleeding disorders includes pressing on the wound, keeping it stable, and raising it if you can. This helps cut down on blood loss until help comes.
When to Seek Medical Attention
People with bleeding disorders should get medical attention right away for severe bleeding. If stopping the bleed is hard or if there’s internal bleeding, seek help fast. Quick medical care is vital.
Hospital Treatment Protocols
Hospital treatment protocols for bleeding disorders often include clotting factor treatments. Doctors follow set rules to manage bleeding well.
Living with Inherited Bleeding Disorders
Living with inherited bleeding disorders can be tough, but it’s possible to lead an active life. The key is a mix of medical care, lifestyle changes, and mental support.
Lifestyle Adjustments
People with these disorders often have to change their lifestyle to avoid bleeding. They should stay away from sports and activities that could hurt them. Regular exercise, like swimming or cycling, is good because it keeps you healthy without too much risk.
Physical Activity Recommendations
Some activities are safer than others for those with bleeding disorders. Low-impact activities like yoga and walking are great. They help keep you flexible and strong without hurting your joints too much.
| Activity | Risk Level | Recommendation |
| Swimming | Low | Recommended |
| Cycling | Moderate | Recommended with safety gear |
| Contact Sports | High | Not Recommended |
Psychological Impact and Support
The mental side of having an inherited bleeding disorder is important. Anxiety and depression can be big issues. Support groups and counseling offer emotional help and ways to deal with the condition.
Educational and Vocational Considerations
When choosing education and jobs, people with bleeding disorders need to think about their condition. Jobs that involve a lot of physical work or are risky might not be right. Career counseling can help find better job paths.
Conclusion
Inherited bleeding disorders like hemophilia and von Willebrand disease are big health challenges. It’s important to know about them to manage them well. This helps improve life quality for those affected.
Hemophilia is caused by a lack of factor VIII or IX. Von Willebrand disease comes from a problem with von Willebrand factor. We’ve talked about how these conditions show up, how to diagnose them, and how to treat them.
New ways to test genes, replace factors, and find new treatments have changed how we handle bleeding disorders. More research and awareness are needed to better care for patients.
This article has covered the main points about hemophilia and von Willebrand disease. It aims to give a full picture. This helps us understand these disorders better and their effects on families.
FAQ
What are inherited bleeding disorders?
Inherited bleeding disorders are passed down through families. They affect how blood clots, causing too much bleeding. Hemophilia and von Willebrand disease are the most common types.
What is hemophilia?
Hemophilia is a genetic disorder that makes blood clotting hard. It happens because of a lack of clotting factors VIII or IX. People with hemophilia often bleed a lot in joints and muscles.
What is von Willebrand disease?
Von Willebrand disease is the most common bleeding disorder. It’s caused by a lack or problem with von Willebrand factor. This protein is key for blood clotting and platelet adhesion. It leads to bleeding in mucous membranes and other issues.
How are bleeding disorders diagnosed?
Doctors use lab tests to check clotting factor levels and function. They also do genetic tests to find specific mutations. Sometimes, they test before a baby is born if there’s a family history.
What are the treatment options for hemophilia?
Hemophilia treatment includes replacing missing clotting factors. This can be done regularly to prevent bleeds or on demand for sudden ones. New treatments like gene therapy are also being explored.
How is von Willebrand disease treated?
Treatment for von Willebrand disease includes desmopressin to release von Willebrand factor. They also use concentrates to replace the protein. Antifibrinolytics are used as additional treatments.
Can people with bleeding disorders lead normal lives?
Yes, with the right treatment and care, people with bleeding disorders can live active lives. Making lifestyle changes and getting regular medical check-ups helps manage the condition.
What are the challenges in managing bleeding disorders across different life stages?
Managing bleeding disorders changes as people grow older. It involves pediatric care, transitioning to adult care, and managing pregnancy and childbirth. Older individuals also have unique needs.
How are life-threatening bleeds managed in individuals with bleeding disorders?
For life-threatening bleeds, it’s important to recognize the signs early. First aid and quick medical help are key. In the hospital, doctors give clotting factor concentrates and supportive care.
What lifestyle adjustments are recommended for individuals with bleeding disorders?
People with bleeding disorders should avoid contact sports and keep a healthy weight. Good oral hygiene and knowing the signs of bleeding are also important. This helps ensure quick treatment.
References
Khudhair, A. A., Salih, A. A. M., & Kadhum, A. J. (2020). Congenital factor VII deficiency in Iraqi children: Single centre experience. Pakistan Journal of Medical Sciences,
Napolitano, M., et al. (2017). Factor VII deficiency: Clinical phenotype, genotype and therapy. Haemophilia,



































