Last Updated on October 21, 2025 by mcelik
Is anemia hereditary? About 1 in 5 women and 1 in 10 men will experience anemia at some point in their lives, making it a major global health issue.
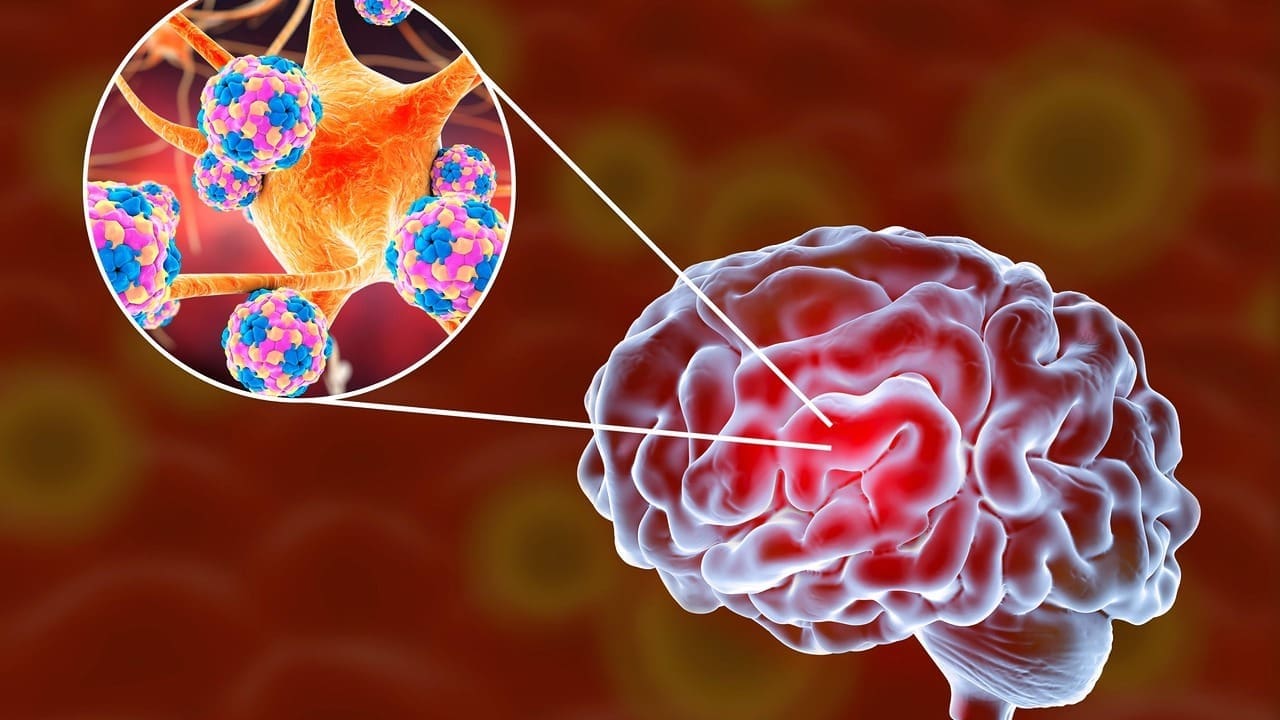
Anemia occurs when the body lacks enough healthy red blood cells to carry oxygen efficiently. Nutritional deficiencies and chronic illnesses are common causes, but genetic disorders also play a big role in certain anemia types.
Understanding the genetic link to anemia helps identify at-risk individuals and ensures proper treatment. Studies on hereditary anemia show that family history can significantly influence who develops the condition.
Key Takeaways
- Anemia affects a significant portion of the population worldwide.
- Genetic disorders can cause certain types of anemia.
- Understanding hereditary factors is key for targeted treatment.
- Research into genetic anemia has found important risk factors.
- Identifying at-risk individuals can prevent serious problems.
Understanding Anemia: The Basics

Anemia is when your body doesn’t have enough healthy red blood cells. These cells are key for carrying oxygen to your body’s tissues. It’s a serious issue that affects millions globally, leading to various health problems.
What Is Anemia?
Anemia happens when your body lacks red blood cells or they don’t have enough hemoglobin. Hemoglobin is a protein that carries oxygen. Without enough, your body’s tissues don’t get the oxygen they need. This can cause everything from mild fatigue to serious health issues.
Common Symptoms and Signs
The symptoms of anemia vary based on its severity and cause. Common signs include:
- Fatigue and weakness
- Shortness of breath
- Pale or yellowish skin
- Dizziness or lightheadedness
- Headaches
These symptoms happen because your body’s tissues aren’t getting enough oxygen. Oxygen is vital for their proper function.
Impact on Health and Quality of Life
Anemia can greatly affect your health and daily life. It can make you less productive, increase your risk of infections, and even lead to heart problems. Knowing the causes and symptoms of anemia is key to managing it well.
By spotting the signs of anemia and getting medical help, you can get the right treatment. This can greatly improve your quality of life.
The Science Behind Blood Cell Production
Blood cell production, or hematopoiesis, is a key process in our bodies. It happens in the bone marrow. Here, many cells and molecules work together to make different blood cells, like red and white blood cells, and platelets.
Normal Red Blood Cell Development
Red blood cells are made through a detailed process. It needs nutrients and growth factors. It starts with hematopoietic stem cells turning into erythroblasts.
These cells go through several stages to become reticulocytes. Then, they enter the bloodstream to become erythrocytes, or red blood cells.
The Role of Hemoglobin
Hemoglobin is a key protein in red blood cells. It carries oxygen from the lungs to our body’s tissues. It’s made of four polypeptide chains and four heme groups, which have iron.
The iron in hemoglobin binds to oxygen. This lets it be carried all over the body. Problems with hemoglobin, like in sickle cell anemia, can cause anemia and health issues.
Key Molecules Affected in Anemia
Many molecules are important for making and working of red blood cells. Problems with these molecules can cause anemia. Some key ones are:
- Globins: Proteins that make up hemoglobin.
- Heme: The part of hemoglobin with iron.
- Erythropoietin: A hormone that controls red blood cell production.
- Iron: Needed for making heme and hemoglobin.
| Molecule | Function | Effect of Deficiency |
| Globins | Component of hemoglobin | Abnormal hemoglobin structure (e.g., sickle cell anemia) |
| Heme | Oxygen binding | Reduced oxygen delivery (e.g., iron deficiency anemia) |
| Erythropoietin | Regulates red blood cell production | Reduced red blood cell production (e.g., anemia of chronic disease) |
| Iron | Essential for heme production | Iron deficiency anemia |
Understanding blood cell production and key molecules is key to knowing anemia. It helps healthcare providers diagnose and treat anemia better.
Is Anemia Hereditary? The Genetic Connection

Anemia is a complex condition that can be influenced by genetics. It happens when there’s not enough red blood cells or when they’re not working right. These cells are key for carrying oxygen to our bodies. Genetics play a big role in anemia, along with other factors like diet and health conditions.
Defining Hereditary Conditions
Hereditary conditions are passed down through genes from parents to kids. In anemia, these conditions affect how red blood cells are made or work. They can be inherited in different ways, like autosomal dominant or recessive.
Knowing if anemia is hereditary is key for treatment. It also helps with family planning and checking relatives for risk.
How Genes Influence Blood Disorders
Genes are vital for making and working of red blood cells. They carry instructions for proteins needed in these cells. Changes in genes can cause disorders, including anemia.
For example, genes can affect hemoglobin production. Hemoglobin is what carries oxygen in red blood cells. Sickle cell anemia and thalassemia are genetic disorders caused by these changes.
Genetic vs. Acquired Anemia
It’s important to know if anemia is genetic or not. Genetic anemia comes from inherited mutations. Acquired anemia is caused by outside factors like diet or disease.
Knowing the cause helps choose the right treatment. Genetic anemia might need special treatments like gene therapy. Acquired anemia can often be fixed by treating the cause.
Types of Anemia: Genetic and Non-Genetic Causes
Anemia can be divided into several types based on its causes. These include genetic and non-genetic factors. Knowing these types is key for accurate diagnosis and effective treatment.
Iron Deficiency Anemia
Iron deficiency anemia is the most common anemia worldwide. It happens when the body lacks enough iron to make hemoglobin. Common causes include not getting enough iron in the diet, chronic blood loss, and needing more iron during pregnancy.
Vitamin Deficiency Anemias
Vitamin deficiency anemias occur when the body lacks essential vitamins for making red blood cells. The most common deficiencies are vitamin B12 and folate. These can be due to not getting enough vitamins in the diet, not being able to absorb them well, or needing more because of certain conditions.
Anemia of Chronic Disease
Anemia of chronic disease is linked to long-term illnesses like infections, inflammatory conditions, and cancer. This anemia is complex. It involves inflammation that affects how the body uses iron and makes red blood cells.
Aplastic Anemia
Aplastic anemia is a rare and serious condition where the bone marrow can’t make blood cells. It can be caused by genetic factors, toxins, certain medications, and viral infections. Treatment often involves addressing the underlying cause and supportive care.
| Type of Anemia | Causes | Characteristics |
| Iron Deficiency Anemia | Inadequate iron intake, chronic blood loss | Low hemoglobin, fatigue, weakness |
| Vitamin Deficiency Anemias | Lack of vitamin B12 or folate | Megaloblastic anemia, neurological symptoms |
| Anemia of Chronic Disease | Chronic infections, inflammation, cancer | Normocytic or microcytic anemia, inflammation |
| Aplastic Anemia | Genetic factors, toxins, medications, viral infections | Bone marrow failure, pancytopenia |
In conclusion, anemia is a complex condition with many types. Each type has its own causes and characteristics. Understanding these differences is vital for proper diagnosis and treatment.
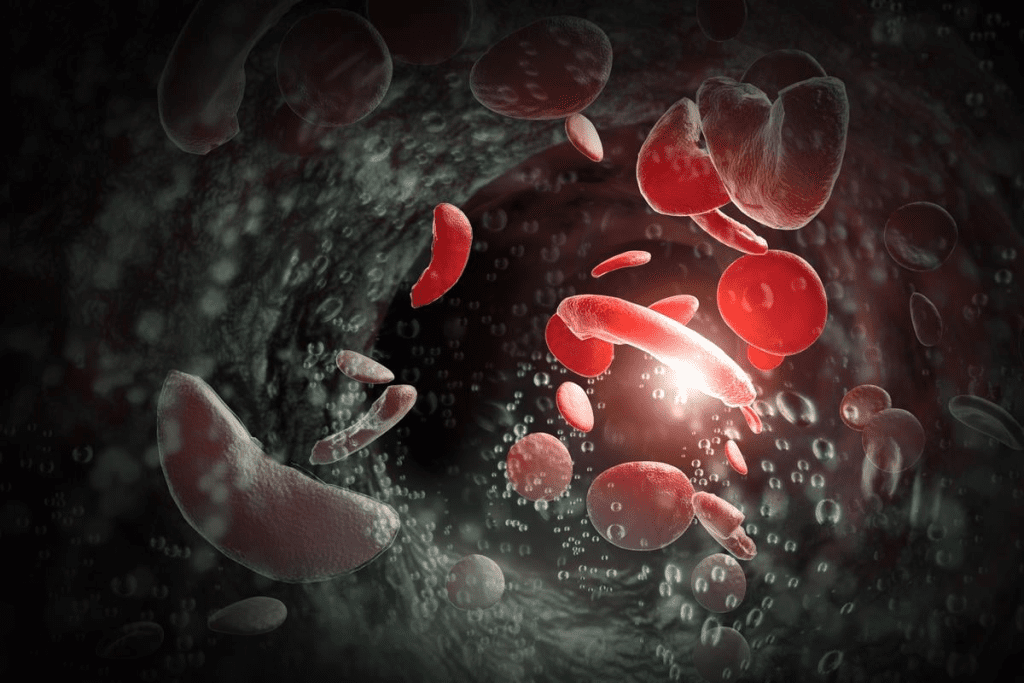
Sickle Cell Anemia: A Classic Genetic Blood Disorder
Sickle cell anemia is caused by a specific mutation in the hemoglobin gene. This mutation leads to the production of abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
This mutation causes red blood cells to be shaped like a crescent or sickle. They can’t move through blood vessels smoothly. The genetic mutation is a point mutation in the HBB gene that codes for the beta-globin subunit of hemoglobin.
The Genetic Mutation Behind Sickle Cell
The genetic mutation behind sickle cell anemia is a change in the DNA sequence of the HBB gene. Glutamic acid is replaced with valine at the sixth position due to a single nucleotide substitution. This change causes the hemoglobin to aggregate under low oxygen conditions, leading to the characteristic sickling of red blood cells.
The mutation is inherited in an autosomal recessive manner. This means an individual must inherit two copies of the mutated gene (one from each parent) to express the condition.
Inheritance Patterns
Sickle cell anemia is inherited when an individual receives two abnormal HBB genes, one from each parent. Carriers, who have one normal and one mutated gene, typically do not display the full symptoms of the disease. They can pass the mutated gene to their offspring.
- If both parents are carriers, there’s a 25% chance each child will have the disease.
- There’s a 50% chance each child will be a carrier like the parents.
- And a 25% chance each child will neither have the disease nor be a carrier.
Global Distribution and Prevalence
Sickle cell anemia is found worldwide but is more prevalent in certain regions. These include parts of Africa, the Mediterranean, the Middle East, and India. It is also found in populations that have migrated from these areas.
In the United States, sickle cell anemia affects approximately 1 in 500 African Americans. About 1 in 12 African Americans carries the sickle cell trait.
Understanding the global distribution and prevalence of sickle cell anemia is key. It’s important for public health efforts aimed at managing and treating the condition.
Thalassemias: Inherited Blood Disorders
Thalassemia is a group of genetic conditions. They affect how the body makes hemoglobin, a key part of blood.
There are mainly two types: alpha thalassemia and beta thalassemia. Knowing about these helps us understand their impact on hemoglobin.
Alpha Thalassemia
Alpha thalassemia happens when genes for alpha-globin chains are changed or missing. The severity depends on how many genes are affected.
Symptoms can vary. Mild cases might not show symptoms, while severe cases can cause serious anemia and health problems.
Beta Thalassemia
Beta thalassemia is caused by changes in genes for beta-globin chains. It can range from beta thalassemia minor to beta thalassemia major.
Beta thalassemia major is more severe. It often needs regular blood transfusions and other treatments.
Genetic Mutations and Inheritance
Thalassemias are inherited in a specific way. A person needs two defective genes to have the condition.
Carriers have one normal and one mutated gene. They might have mild symptoms or none at all. But they can pass the mutated gene to their kids.
Knowing about the genetic mutations and how they are passed down is key. It helps with diagnosis, treatment, and planning families.
Hereditary Spherocytosis and Other Membrane Defects
Red blood cell membrane defects, like hereditary spherocytosis, are genetic disorders that cause anemia. These conditions come from mutations in genes that are key for the structure and function of red blood cell membranes.
Genetic Basis of Membrane Disorders
Hereditary spherocytosis is mainly caused by mutations in genes like ANKS1, SLC4A1, and EPB42. These genes help keep the red blood cell membrane strong. The mutations lead to the creation of abnormal proteins in the membrane.
This makes red blood cells lose their biconcave disk shape and turn spherical. The spherical shape makes them more likely to break down early, a process called hemolysis. This leads to anemia because the body can’t keep a healthy number of red blood cells.
Clinical Manifestations
The symptoms of hereditary spherocytosis can vary a lot. Common signs include anemia, jaundice, and a big spleen. The severity of these symptoms can range from mild to severe and may need medical treatment, like blood transfusions or removing the spleen.
Diagnosis is made by a doctor’s evaluation, lab tests (like blood smears and osmotic fragility tests), and genetic testing to find the mutation.
Inheritance Patterns
Hereditary spherocytosis usually follows an autosomal dominant pattern. This means just one copy of the mutated gene causes the condition. But, some cases might be autosomal recessive, needing two copies of the mutated gene (one from each parent).
Knowing the inheritance pattern is key for genetic counseling. It helps figure out the risk of passing the condition to future generations.
Enzyme Deficiencies: G6PD and Pyruvate Kinase Deficiency
Certain enzyme deficiencies, like G6PD and pyruvate kinase deficiency, can cause anemia. This is because red blood cells don’t work right. These conditions are genetic and affect how red blood cells are made and work.
Genetic Mutations Affecting Enzymes
Genetic mutations cause G6PD and pyruvate kinase deficiency. G6PD deficiency comes from mutations in the G6PD gene. This gene makes the enzyme glucose-6-phosphate dehydrogenase, which protects red blood cells.
Mutations in the G6PD gene mean red blood cells break down easily. This is because they lack the enzyme to protect them.
Pyruvate kinase deficiency is caused by mutations in the PKLR gene. This affects the pyruvate kinase enzyme, which is key for energy in red blood cells. Without enough of this enzyme, red blood cells don’t last long.
Triggers and Symptoms
People with G6PD deficiency might have hemolytic crises. This can be triggered by infections, certain medicines, or eating fava beans. Symptoms include jaundice, feeling tired, and shortness of breath.
Pyruvate kinase deficiency can cause anemia, jaundice, and a big spleen. The symptoms can vary from mild to severe.
Inheritance and Risk Factors
G6PD and pyruvate kinase deficiency are inherited. G6PD is usually passed down in an X-linked recessive pattern. This means men are more likely to get it than women.
Pyruvate kinase deficiency is passed down in an autosomal recessive pattern. This means you need two copies of the bad gene to have the condition. Carriers have one good and one bad gene and usually don’t show symptoms but can pass the bad gene to their kids.
Fanconi Anemia and Other Rare Genetic Anemias
It’s important to know the genetic causes of rare anemias like Fanconi anemia. These conditions have unique genetic roots and symptoms. This makes diagnosis and treatment tricky.
The Genetic Basis of Fanconi Anemia
Fanconi anemia is a rare genetic disorder caused by DNA repair gene mutations. It leads to bone marrow failure, birth defects, and a higher cancer risk. The mutations stop the body from fixing DNA damage, causing genetic instability.
Key Features of Fanconi Anemia:
- Bone marrow failure leading to anemia, neutropenia, and thrombocytopenia
- Congenital abnormalities, such as skeletal defects and developmental delays
- Increased susceptibility to malignancies, such as acute myeloid leukemia
Diamond-Blackfan Anemia
Diamond-Blackfan anemia is a rare genetic disorder that affects red blood cell production. It usually starts in infancy or early childhood. It’s caused by mutations in genes that make ribosomal proteins.
Clinical Features:
- Severe anemia requiring lifelong transfusions
- Congenital anomalies, such as craniofacial abnormalities and thumb anomalies
- Increased risk of certain malignancies
Other Rare Inherited Anemias
There are other rare genetic anemias, each with its own genetic and clinical traits. These include:
- Congenital dyserythropoietic anemias, characterized by ineffective erythropoiesis
- Pearson syndrome, a mitochondrial DNA deletion disorder affecting hematopoiesis
Knowing the genetic basis of these rare anemias is key for accurate diagnosis and treatment. Genetic testing is vital for finding the underlying mutations and making treatment decisions.
Is Iron Deficiency Anemia Genetic?
Iron deficiency anemia can be caused by not enough iron in the diet or losing too much blood. But, research shows that genes might also play a big role.
Genetic Factors Influencing Iron Absorption
Iron absorption is complex and influenced by genes. The body needs to absorb iron from food to make healthy red blood cells. Genetic variations can make iron absorption less efficient, even with enough iron in the diet.
For example, genes like HFE, TMPRSS6, and TFR2 are important for iron absorption. Changes in these genes can make it harder for the body to take in iron, leading to anemia.
Hereditary Hemochromatosis and Iron Overload
Hereditary hemochromatosis is a genetic disorder that causes too much iron absorption, leading to iron overload. It’s linked to mutations in the HFE gene. This condition is different from iron deficiency anemia but studying it helps us understand iron metabolism better.
| Gene | Function | Effect of Mutation |
| HFE | Regulation of iron absorption | Increased iron absorption |
| TMPRSS6 | Inhibition of hepcidin | Decreased iron absorption if mutated |
| TFR2 | Regulation of hepcidin | Altered iron metabolism |
Family Patterns in Iron Deficiency
Looking at family patterns can give us hints about the genetic side of iron deficiency anemia. Studies have found that people with a family history of iron deficiency are more likely to get it. This suggests a genetic link.
More research into the genetics of iron deficiency anemia could help find people at risk. It could also lead to more tailored treatments.
Genetic Testing for Anemia: What to Expect
Genetic testing can offer insights into anemia’s genetic roots. This knowledge is key for diagnosing anemia types, guiding treatments, and planning families.
Types of Genetic Tests Available
There are many genetic tests for anemia, each with its own role. These include:
- Diagnostic testing: Confirms anemia in those showing symptoms.
- Carrier testing: Finds people who might pass on genetic mutations to their kids.
- Predictive testing: Shows the chance of getting anemia based on genes.
- Preimplantation genetic diagnosis (PGD): Picks embryos without certain genetic issues for IVF.
These tests differ in how they look at genes, from specific ones to the whole genome.
When Genetic Testing Is Recommended
Genetic testing is advised for those with anemia in their family history. It’s also for those with certain anemia types, like sickle cell and thalassemia. It’s suggested for unusual anemia cases or suspected genetic disorders.
Interpreting Test Results
Understanding genetic testing results for anemia needs expertise. The findings can be complex. They might show:
- A genetic mutation linked to anemia, confirming a diagnosis.
- Being a carrier of a genetic mutation, affecting family planning.
- A negative result, which might exclude a genetic cause but doesn’t rule out anemia.
Grasping the results and their meanings is vital for making smart choices about treatment and family planning.
Does Anemia Run in Families? Understanding Inheritance Patterns
Anemia can run in families through different genetic pathways. The pattern of inheritance depends on the specific cause of anemia. Conditions can follow autosomal dominant, autosomal recessive, X-linked, or multifactorial patterns.
Autosomal Dominant Inheritance
Autosomal dominant inheritance means one mutated gene can cause the condition. Hereditary spherocytosis is an example. A parent with the condition has a 50% chance of passing it to each child.
Autosomal Recessive Inheritance
Autosomal recessive conditions require two mutated genes to develop. Sickle cell anemia and beta-thalassemia are examples. Carriers, with one normal and one mutated gene, usually don’t show symptoms but can pass the mutated gene to their children.
X-Linked Inheritance
X-linked inheritance involves genes on the X chromosome. G6PD deficiency is an example, affecting males more often. Females can be carriers and pass the condition to their sons.
Multifactorial Inheritance
Some anemias result from both genetic and environmental factors. Understanding this can help manage and prevent the condition.
| Inheritance Pattern | Description | Examples of Anemia |
| Autosomal Dominant | One mutated gene copy causes the condition | Hereditary Spherocytosis |
| Autosomal Recessive | Two mutated gene copies required | Sickle Cell Anemia, Beta-Thalassemia |
| X-Linked | Genes on the X chromosome | G6PD Deficiency |
| Multifactorial | Both genetic and environmental factors | Some forms of Iron Deficiency Anemia |
Knowing the inheritance patterns of anemia is key for genetic counseling. It helps assess the risk for family members. Healthcare providers can then offer more precise guidance on passing the condition to future generations.
Managing Hereditary Anemia: Treatment Approaches
Managing hereditary anemia requires a variety of methods. This includes traditional treatments and new research. It also involves making lifestyle changes. Each approach is tailored to the person’s needs.
Medical Interventions
Medical treatments are key in managing hereditary anemia. They include blood transfusions to boost healthy red blood cells. Medications help reduce iron overload and, in some cases, bone marrow transplantation.
Key medical interventions include:
- Blood transfusions to improve oxygen delivery to tissues
- Iron chelation therapy to manage iron overload
- Bone marrow transplantation in severe cases
- Medications to manage symptoms and complications
Lifestyle Modifications
Lifestyle changes are also vital. Patients should eat a diet rich in iron, vitamin B12, and folate. They should also avoid too much alcohol and manage chronic conditions.
Recommended lifestyle changes include:
- Eating a balanced diet that includes iron-rich foods
- Avoiding alcohol and smoking
- Staying hydrated and managing stress
- Regular check-ups with healthcare providers
Emerging Therapies and Research
New treatments for hereditary anemia are being developed. Gene therapy aims to fix the genetic issue causing the anemia. Other research focuses on new medications and ways to manage iron overload.
Emerging therapies include:
- Gene therapy to correct genetic mutations
- New drugs to manage symptoms and complications
- Advanced iron chelation therapies
- Stem cell transplantation techniques
As research improves, the future for those with hereditary anemia looks brighter. There’s hope for a better quality of life and longer life expectancy.
Genetic Counseling for Families with Hereditary Anemia
Genetic counseling is key for families dealing with hereditary anemia. It offers support and guidance. This helps families grasp the condition, its effects, and how to manage it.
The Role of Genetic Counselors
Genetic counselors are experts in genetic disorders. They help families understand hereditary anemia. They share details on the condition’s genetics, how it’s passed down, and the chances of it affecting future generations.
Family Planning Considerations
Genetic counseling is vital for family planning. It helps parents understand risks to their children. Counselors discuss reproductive options and technologies.
- Preimplantation genetic diagnosis (PGD)
- Prenatal testing
- Family planning strategies
Support Resources for Families
Genetic counselors also connect families with support. This includes groups, educational materials, and services. These help families deal with the emotional and practical sides of hereditary anemia.
Support groups offer a sense of community. Educational materials provide ongoing guidance.
By using these resources, families can better handle hereditary anemia. This improves their overall quality of life.
Future Directions: Gene Therapy and Advanced Treatments
The field of treating genetic anemia is on the verge of a big change. Thanks to gene therapy and new treatments, patients and doctors now have better options. These options aim to make life better for those with genetic anemia.
Current Research in Gene Therapy
Gene therapy is a new way to treat genetic anemia by fixing the genetic problem. Current research is working on making this method safe and effective. It uses special tools to get healthy genes into cells.
Studies have shown great results in treating beta-thalassemia and sickle cell disease with gene therapy. These are two common types of genetic anemia.
CRISPR and Genetic Editing
CRISPR-Cas9 is a big deal in genetic editing. CRISPR lets scientists edit genes precisely. This means they can fix the genes that cause anemia.
Research is looking into how safe and effective CRISPR is for treating genetic anemia. It’s a promising technology for fixing genetic problems.
Promising Clinical Trials
Many clinical trials are testing gene therapy and genetic editing for genetic anemia. These trials are key to understanding and improving these treatments. They help bring new hope to patients.
For example, trials on sickle cell disease and beta-thalassemia have shown good results. Some patients have seen big improvements in their health.
As these treatments get better, they offer hope for those with genetic anemia. The future of treating anemia looks bright, thanks to gene therapy, genetic editing, and other new methods.
Conclusion: Understanding the Genetic Landscape of Anemia
Understanding anemia’s genetic landscape is key for those affected and healthcare workers. Anemia is complex, with many causes, including genetics. This leads to genetic anemia.
Genetic tests can find specific mutations. This helps in treating sickle cell anemia and thalassemias. Knowing about anemia helps in planning families and improves diagnosis.
New treatments, like gene therapy, are hopeful for managing hereditary anemia. Studying anemia’s genetics further will lead to better diagnosis, treatment, and support. This will greatly improve life for those affected.
FAQ
Is anemia genetic?
Anemia can be genetic, depending on the type. Some anemias, like sickle cell anemia and thalassemia, come from genetic mutations. But, not all anemias are genetic. Some are caused by lack of nutrients, chronic diseases, or other factors.
What are the genetic causes of anemia?
Genetic causes of anemia include mutations that affect red blood cells. This is seen in sickle cell anemia, thalassemia, and hereditary spherocytosis. These mutations are passed down from parents.
Can anemia be inherited?
Yes, some anemias can be inherited. For example, sickle cell anemia and thalassemia are caused by genetic mutations. The chance of inheriting these conditions depends on the parents’ genetic status.
Is iron deficiency anemia genetic?
Iron deficiency anemia is usually caused by lack of nutrients or other non-genetic factors. But, there can be genetic influences on iron absorption and metabolism. For instance, hereditary hemochromatosis is a genetic condition that affects iron absorption.
What is the role of genetic testing in diagnosing anemia?
Genetic testing can diagnose certain anemias, like sickle cell anemia and thalassemia. It identifies the genetic mutations behind them. It also shows the risk of passing these conditions to future generations.
How is hereditary anemia managed?
Managing hereditary anemia involves medical treatments, lifestyle changes, and new therapies like gene therapy. The treatment depends on the type and severity of the anemia.
What is the significance of genetic counseling for families with hereditary anemia?
Genetic counseling is key for families with hereditary anemia. It gives information on the risk of passing the condition, its implications for family planning, and support resources. Genetic counselors help families understand and deal with genetic anemia.
Are there new treatments on the horizon for genetic anemia?
Yes, new treatments and research are underway for genetic anemia. This includes gene therapy, CRISPR, and clinical trials for new therapies. These advancements offer hope for better outcomes for those with genetic anemia.
Can anemia run in families?
Yes, certain anemias, mainly those with a genetic basis, can run in families. Knowing the inheritance pattern of a specific anemia can help predict the risk for family members.
What are the different inheritance patterns for anemia?
Anemia can be inherited in different ways. This includes autosomal dominant, autosomal recessive, X-linked, and multifactorial inheritance. The specific pattern depends on the genetic cause of the anemia.
Reference
- Weatherall, D. J. (2010). The inherited diseases of hemoglobin are an emerging global health burden. Blood, 115(22), 4331“4336. https://pubmed.ncbi.nlm.nih.gov/20233970