Last Updated on October 21, 2025 by mcelik

Sickle cell disease affects millions worldwide. 1 in 500 African Americans are born with it.Learn what causes the anemia in sickle cell disease, how it is inherited, and which parent passes the sickle cell gene to their child.
This disease is a genetic disorder. It changes how red blood cells make hemoglobin.
Key Takeaways
- Sickle cell disease is a genetic disorder affecting hemoglobin production.
- The condition is inherited from both parents.
- Understanding the inheritance pattern is key for affected families.
- Genetic testing can identify disease carriers.
- Family planning options are available for carriers.
The Nature of Sickle Cell Disease
To understand sickle cell disease, we need to know its definition and how it works. It’s a group of genetic disorders that affect hemoglobin. Hemoglobin is a protein in red blood cells that carries oxygen.
Definition and Basic Mechanism
Sickle cell disease is caused by abnormal hemoglobin, called sickle hemoglobin or hemoglobin S. This abnormal hemoglobin makes red blood cells bend into a sickle shape when oxygen levels are low. This bending leads to early destruction of red blood cells and can block blood flow in small vessels.
The disease works by changing red blood cells into sickle shapes. This happens because of hypoxia, acidosis, and dehydration. These sickled cells are destroyed faster and can block blood flow, causing vaso-occlusive crises and other problems.
Sickle Cell Trait vs. Sickle Cell Disease
It’s important to know the difference between sickle cell trait and sickle cell disease. Sickle cell trait happens when someone has one normal and one sickle hemoglobin gene. They usually don’t show symptoms but can pass the sickle gene to their kids.
Sickle cell disease happens when someone has two sickle hemoglobin genes. This leads to full symptoms, including anemia, pain crises, and a higher risk of infections.
- Sickle Cell Trait: Usually doesn’t cause symptoms, but can be a problem in extreme cases.
- Sickle Cell Disease: Can cause serious health problems, like chronic anemia, pain episodes, and a higher risk of infections.
Knowing the difference between sickle cell trait and disease is key for genetic counseling and managing health.
The Genetic Mutation Behind Sickle Cell Disease
A single mutation in the HBB gene causes sickle cell disease. This mutation changes how the beta-globin subunit of hemoglobin is made. It leads to the creation of abnormal hemoglobin, known as sickle hemoglobin or HbS.
The HBB Gene and Its Function
The HBB gene tells our bodies how to make the beta-globin subunit of hemoglobin. Hemoglobin is a protein in red blood cells that carries oxygen. The HBB gene is on chromosome 11, and a mutation can change its function.
Normally, the HBB gene makes a beta-globin protein important for adult hemoglobin (HbA). But, in sickle cell disease, a mutation changes the beta-globin chain. This results in sickle hemoglobin (HbS).
How a Single Mutation Changes Everything
The HBB gene mutation changes the hemoglobin structure and red blood cells. Red blood cells with HbS can become sickle-shaped. This leads to their early destruction and complications of sickle cell disease.
The table below shows the main differences between normal hemoglobin (HbA) and sickle hemoglobin (HbS):
| Characteristics | Normal Hemoglobin (HbA) | Sickle Hemoglobin (HbS) |
| Genetic Basis | Normal HBB gene | Mutated HBB gene |
| Hemoglobin Structure | Normal beta-globin | Abnormal beta-globin with valine substitution |
| Red Blood Cell Shape | Normal, disk-shaped | Sickle-shaped under certain conditions |
Knowing the genetic cause of sickle cell disease is key for finding tests and treatments. Genetic counseling helps families with a history of the disease. It gives them information on the risk of passing it to their children.
Inheritance Pattern: Is Sickle Cell Anemia Recessive or Dominant?
Sickle cell anemia is caused by an autosomal recessive inheritance pattern. This means a person needs two copies of the HBB gene defect, one from each parent, to have the disease. Knowing this helps families with sickle cell history understand their risk of passing it to their kids.
Autosomal Recessive Inheritance Explained
The disease-causing gene is on one of the 22 non-sex chromosomes. A person must have two copies of the mutated gene to have the disease. Those with one normal and one mutated gene are carriers and usually don’t show symptoms but can pass the gene to their kids.
Carrier Status: Carriers of the sickle cell gene are usually healthy but can pass the gene to their children. If both parents are carriers, there’s a 25% chance their child will have sickle cell anemia, a 50% chance they’ll be a carrier, and a 25% chance they won’t have the disease or be a carrier.
Probability Charts for Parents with Different Genotypes
Let’s look at a probability chart for parents with different genotypes regarding the sickle cell gene:
| Parent 1 Genotype | Parent 2 Genotype | Chance of Child Having Sickle Cell Anemia | Chance of Child Being a Carrier |
| Carrier (HbAS) | Carrier (HbAS) | 25% | 50% |
| Carrier (HbAS) | Normal (HbAA) | 0% | 50% |
| Affected (HbSS) | Carrier (HbAS) | 50% | 50% |
| Affected (HbSS) | Affected (HbSS) | 100% | 0% |
The risk of a child getting sickle cell anemia changes a lot based on the parents’ genotypes. Genetic counseling helps families understand their risks and plan for the future.
Which Parent Contributes to Sickle Cell Disease?
Sickle cell disease is a genetic disorder passed down from both parents. It’s important for parents-to-be, with a family history of the disease, to understand this.
The Role of Both Parents in Disease Transmission
Sickle cell disease is an autosomal recessive disorder. This means a person needs two defective hemoglobin genes, one from each parent, to have the disease. If someone has only one defective gene, they are a carrier but don’t show symptoms.
When both parents are carriers, there’s a 25% chance their child will have sickle cell disease. There’s also a 50% chance the child will be a carrier like the parents. And a 25% chance the child will have two normal genes, not affected or a carrier.
Common Misconceptions About Maternal vs. Paternal Inheritance
Many think sickle cell disease comes from one parent more than the other. But, it’s not biased towards the maternal or paternal line. It depends on the genes from both parents.
Here’s a simple table to show the possible genotypes of offspring when both parents are carriers:
| Mother’s Gene | Father’s Gene | Child’s Genotype | Probability |
| Normal | Normal | Normal | 25% |
| Normal | Sickle Cell Trait | Carrier | 50% (combined) |
| Sickle Cell Trait | Normal | Carrier | |
| Sickle Cell Trait | Sickle Cell Trait | Sickle Cell Disease | 25% |
The table shows the chance of a child getting sickle cell disease is the same, no matter the parent. This proves both parents play an equal role in the risk.
Knowing the genetic risks and talking to a healthcare provider or genetic counselor is key. It helps parents-to-be make informed choices about starting a family.
What Causes the Anemia in Sickle Cell Disease
In sickle cell disease, anemia comes from hemolysis, impaired erythropoiesis, and vaso-occlusive events. These factors greatly affect a patient’s life quality.
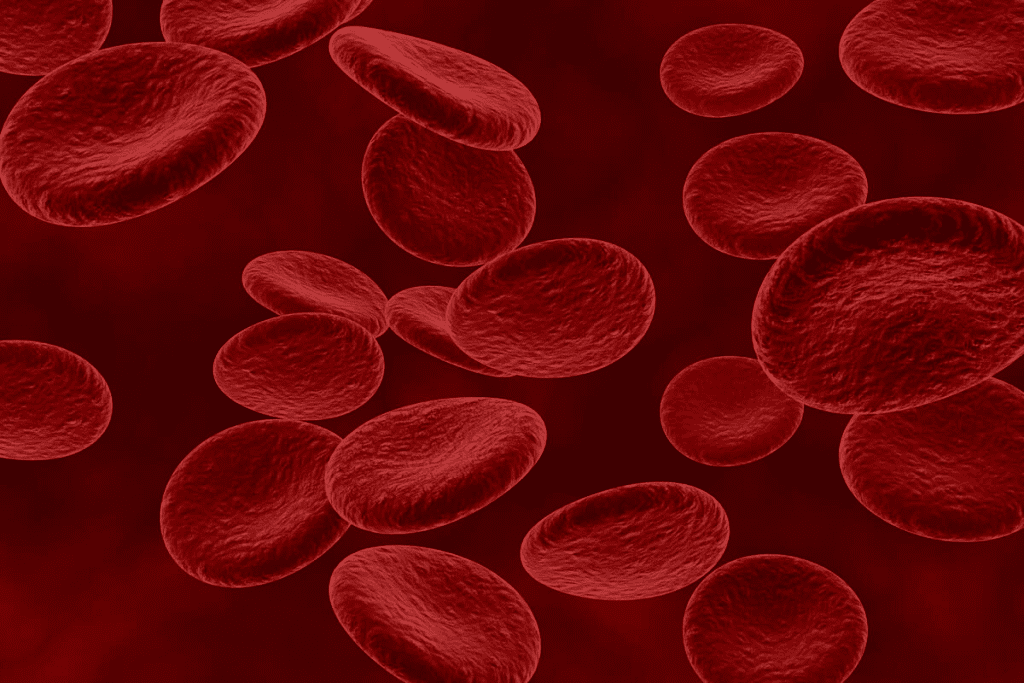
Hemolysis: Premature Destruction of Red Blood Cells
Hemolysis is when red blood cells die early. This is a key part of sickle cell disease. The abnormal hemoglobin makes red blood cells stiff and sickle-shaped, leading to their early death.
As a result, red blood cells last only 10-20 days, much less than the normal 120 days. This early death of red blood cells is a major reason for anemia in sickle cell disease.
“The premature destruction of red blood cells is a critical factor in the development of anemia in sickle cell disease,” as noted by experts in the field. This hemolysis not only reduces the number of red blood cells but also releases hemoglobin into the bloodstream, potentially causing further complications.
Impaired Erythropoiesis in Bone Marrow
Impaired erythropoiesis means the bone marrow can’t make new red blood cells well. In sickle cell disease, the bone marrow works hard to replace lost red blood cells. But, it’s stressed by inflammation and oxidative stress, making it harder to produce new cells.
Chronic inflammation in sickle cell disease also affects erythropoiesis. This inflammation lowers the production of erythropoietin, a hormone needed for making red blood cells. This makes anemia worse.
Vaso-occlusive Events and Organ Damage
Vaso-occlusive events happen when sickled red blood cells block small blood vessels. This causes tissue ischemia and organ damage. These events lead to acute pain crises and chronic organ dysfunction over time.
The damage to organs makes it harder for the body to make red blood cells and stay healthy. This creates a cycle that makes anemia worse in sickle cell disease. Knowing how these mechanisms work is key to finding better treatments.
The Sickling Process and Triggering Factors
The sickling process is a key part of sickle cell disease. It happens when certain environmental and physiological factors are present. This process changes normal red blood cells into sickle-shaped ones, leading to health issues.
How Normal Cells Transform into Sickle Cells
Normal red blood cells are flexible and move well through blood vessels. But, in sickle cell disease, these cells have abnormal hemoglobin, called sickle hemoglobin or HbS. When they release oxygen, the HbS polymerizes, making the cells rigid and sickle-shaped.
This change isn’t quick; it happens under specific conditions. Factors like the amount of HbS in the cell, other abnormal hemoglobins, and oxygen levels play a role. Low oxygen levels and dehydration can also trigger this change.
Environmental and Physiological Triggers
Many factors can start the sickling process. Environmental triggers include extreme temperatures, high altitudes, and intense physical activity. Physiological triggers include infections, dehydration, and stress. Knowing these triggers helps manage sickle cell disease better.
For example, high altitudes can lower oxygen levels, triggering sickling. Intense physical activity can cause dehydration, increasing HbS concentration. Infections can also trigger a crisis by causing inflammation and changing the body’s state.
“Managing environmental and physiological triggers is key to preventing sickle cell crises and improving the quality of life for individuals with sickle cell disease.”
To understand these triggers better, let’s look at a summary table:
| Trigger Type | Examples | Effect on Sickling |
| Environmental | High altitude, extreme temperatures | Increases risk of sickling due to low oxygen or temperature stress |
| Physiological | Infections, dehydration, stress | Promotes sickling through dehydration, inflammation, or physiological stress |
| Physical | Intense physical activity | Can cause dehydration and increase HbS concentration, promoting sickling |
Understanding the sickling process and its triggers helps those with sickle cell disease manage their condition. This can reduce the risk of complications.
Who Can Get Sickle Cell Disease?
Understanding who gets sickle cell disease involves looking at ethnic and geographic groups. It’s a genetic disorder that affects red blood cells, making them sickle-shaped. This happens because of a problem with hemoglobin production.
The disease isn’t limited to any ethnic or geographic group. But, its occurrence varies a lot. We’ll look at where sickle cell disease is common and why.
Ethnic and Geographic Distribution
Sickle cell disease is more common where malaria used to be a big problem. This includes parts of Africa, the Mediterranean, the Middle East, and India. In the U.S., about 1 in 500 African Americans has it.
In other places like the Mediterranean, the Middle East, and India, it’s found too. But not as often. The disease’s spread is tied to malaria’s history. The sickle cell gene helps protect against malaria.
Evolutionary Advantage: Malaria Protection
The sickle cell disease is common in malaria areas because it offers protection. People with the sickle cell gene are less likely to get severe malaria. This is thanks to Plasmodium falciparum.
This protection is why the sickle cell gene is common in malaria areas. It doesn’t make people immune to malaria. But, it makes the disease less severe, helping people survive.
To sum up, sickle cell disease is found worldwide but more in certain groups. Its spread is tied to malaria’s history. The sickle cell trait protects against malaria, keeping the disease in these areas.
Diagnosing Sickle Cell Disease
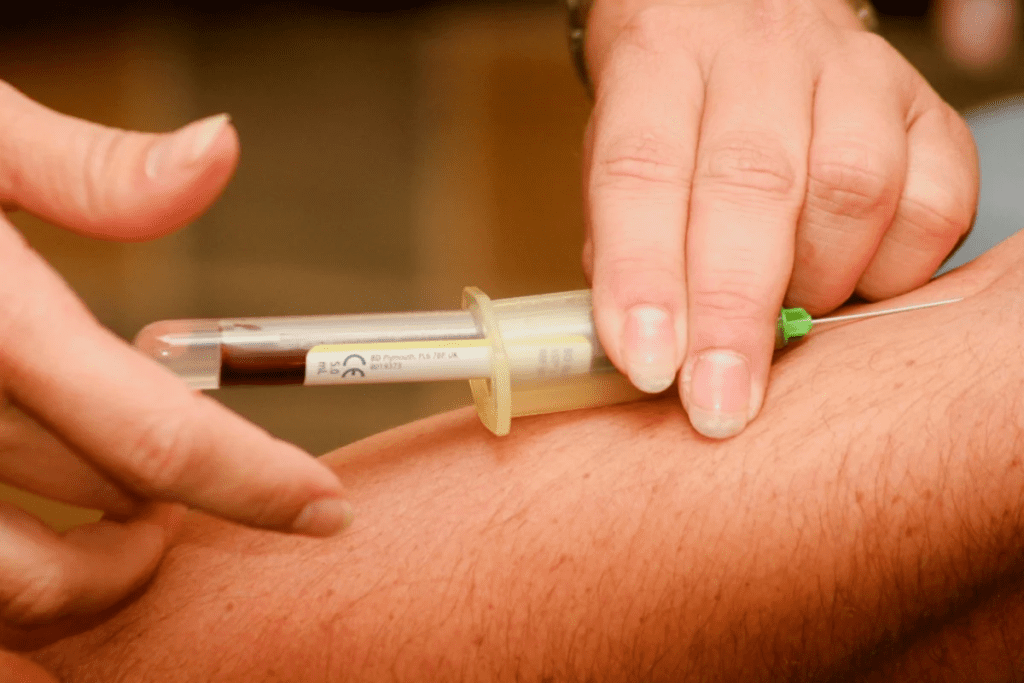
Diagnosing sickle cell disease takes a few steps. These include newborn screening, genetic testing, and prenatal diagnosis. These steps are key for catching the disease early and managing it well.
Newborn Screening Programs
Newborn screening is a big help in finding sickle cell disease early. It’s a simple blood test done in the first few days of life. It checks for abnormal hemoglobin.
Benefits of Newborn Screening:
- Early detection means quick medical help.
- Parents learn about their child’s health, helping them make choices.
- Early treatment can stop serious problems.
Genetic Testing Methods
Genetic testing is also important for diagnosing sickle cell disease. It looks at the HBB gene to find the disease-causing mutation.
| Testing Method | Description | Application |
| PCR (Polymerase Chain Reaction) | Amplifies DNA sequences to detect the sickle cell mutation. | Used for diagnosing sickle cell disease and trait. |
| HPLC (High-Performance Liquid Chromatography) | Separates and quantifies different hemoglobin types. | Used to diagnose and monitor sickle cell disease. |
Prenatal Diagnosis Options
Prenatal diagnosis lets parents know if their unborn baby has sickle cell disease. It’s done through:
- Chorionic Villus Sampling (CVS): Removes a small sample of cells from the placenta.
- Amniocentesis: Involves withdrawing a sample of amniotic fluid.
“Prenatal diagnosis gives expectant parents vital info about their baby’s health. It helps them prepare for the future or make informed choices about their pregnancy.”
These diagnostic methods have changed how we manage sickle cell disease. They allow for early treatment and better patient outcomes.
Symptoms and Complications of Sickle Cell Anemia
It’s important to know the symptoms and complications of sickle cell anemia. This disease has many acute and chronic issues. These can really affect a person’s life quality.
Acute Pain Crises and Management
Acute pain crises, or vaso-occlusive crises, are common in sickle cell anemia. They happen when sickled red blood cells block blood vessels. This causes pain and tissue damage.
To manage these crises, doctors use hydration and pain relief. Sometimes, people need to stay in the hospital.
Here are some ways to handle acute pain crises:
- Start treatment early when pain starts
- Drink plenty of water to avoid dehydration
- Take pain medicines, like opioids for severe cases
- Watch for signs of serious problems, like acute chest syndrome
Chronic Complications by Body System
Sickle cell anemia can cause long-term problems in different parts of the body. These include:
| Body System | Complications |
| Cardiovascular | Cardiac enlargement, heart failure |
| Respiratory | Acute chest syndrome, pulmonary hypertension |
| Neurological | Stroke, cognitive impairment |
Regular check-ups and care can help prevent these problems.
Impact on Growth and Development in Children
Sickle cell anemia can slow down growth and development in kids. This is because of chronic anemia and other issues. It’s key for kids to see their doctors often.
“Children with sickle cell disease need full care to manage their condition. This helps them grow and develop normally.”
Treatment Approaches for Sickle Cell Disease
Managing sickle cell disease requires a mix of treatments, cures, and preventive care. We’ll look at these methods to see how they help patients live better lives.
Standard Medical Interventions
Standard treatments for sickle cell disease are key to managing symptoms and preventing problems. These treatments include:
- Hydroxyurea: A drug that lowers the number of pain crises and may cut down on blood transfusions.
- Blood Transfusions: Regular transfusions can lower the risk of complications by reducing sickled red blood cells.
- Pain Management: It’s important to manage pain well. This might involve non-narcotic and narcotic drugs, based on the pain’s severity.
Curative Options: Stem Cell Transplantation and Gene Therapy
For some, there are curative options. These include:
- Stem Cell Transplantation: Also called bone marrow transplantation, it replaces the patient’s marrow with healthy donor marrow. It’s the only cure for sickle cell disease now.
- Gene Therapy: A new field that aims to fix the genetic issue causing sickle cell disease. Gene therapy is experimental but shows great promise for the future.
Preventive Care and Maintenance
Preventive care is essential for managing sickle cell disease. This includes:
- Regular Check-Ups: Ongoing medical care to watch the disease and tackle complications early.
- Vaccinations: Keeping up with recommended vaccines to prevent infections.
- Lifestyle Modifications: Making healthy choices, like drinking plenty of water, avoiding extreme weather, and managing stress.
By using these treatments together, we can greatly improve sickle cell disease management. This helps patients live better lives.
Genetic Counseling for Families with Sickle Cell History
For families with sickle cell disease history, genetic counseling is key. It helps understand and manage the risk of passing on the condition. We offer full support to families dealing with this genetic disorder.
Understanding Genetic Risk
Genetic counseling explains the risks of sickle cell disease. We guide families on the genetic basis and the chance of passing it to their kids. Important points include:
- Explaining the autosomal recessive inheritance pattern of sickle cell disease
- Discussing the probability of having a child with sickle cell disease or trait based on the parents’ genotypes
- Reviewing family history to identify carriers and affected individuals
Knowing these risks helps families make smart reproductive choices. We stress the value of genetic testing to find out carrier status and talk about what the results mean.
Family Planning Options
Families with sickle cell disease have many family planning choices. We share info on:
- Prenatal testing, including chorionic villus sampling (CVS) and amniocentesis
- Preimplantation genetic diagnosis (PGD) for families undergoing in vitro fertilization (IVF)
- Adoption as an alternative family building option
We aim to support families in making choices that fit their needs. Our goal is to offer comprehensive and compassionate care to those facing sickle cell disease challenges.
Living with Sickle Cell Disease: Management Strategies
Living with sickle cell disease can be tough, but the right strategies can help. It’s about medical care, lifestyle changes, and support. These steps can make life better.
Lifestyle Modifications to Prevent Crises
Changing your lifestyle can help avoid sickle cell crises. Staying hydrated is key, as dehydration can cause sickling. Also, avoid extreme temperatures and eat a balanced diet.
- Drink plenty of water all day.
- Stay away from hard work, when it’s hot.
- Manage stress with meditation or deep breathing.
Navigating Healthcare Systems
Finding your way through healthcare can be hard with sickle cell disease. It’s vital to find a knowledgeable healthcare provider. Regular visits and care can help manage symptoms and prevent problems.
| Healthcare Aspect | Description | Benefit |
| Regular Check-ups | Frequent visits to healthcare providers | Early detection of complications |
| Preventive Care | Measures to prevent infections and crises | Less frequent sickle cell crises |
| Specialist Care | Access to specialists knowledgeable about sickle cell disease | Personalized treatment plans |
Support Resources and Community
Having support resources and a community can make a big difference. Support groups, online or in-person, offer a place to share and learn from others.
By using these strategies, people with sickle cell disease can face challenges head-on. They can live more fulfilling lives.
Conclusion
Understanding sickle cell disease’s genetic basis is key to managing it well. This disease is caused by a mutation in the HBB gene. It leads to abnormal hemoglobin and sickle-shaped red blood cells, causing health problems.
Managing sickle cell anemia needs a mix of lifestyle changes, medical care, and preventive steps. Knowing the genetic cause helps families deal with the condition better. Genetic counseling is vital for those with sickle cell history, helping with planning and managing the disease.
We need more research and support for sickle cell disease. By learning more about its genetics and improving care, we can improve life for those with it. Managing sickle cell anemia requires a full approach, covering physical, emotional, and social needs.
FAQ
What is sickle cell disease?
Sickle cell disease is a genetic disorder. It affects the hemoglobin in red blood cells. This makes them misshapen and break down, leading to anemia and other issues.
What causes sickle cell disease?
It’s caused by a mutation in the HBB gene. This gene codes for the beta-globin subunit of hemoglobin. The mutation leads to the production of abnormal hemoglobin, known as sickle hemoglobin or hemoglobin S.
Is sickle cell disease inherited?
Yes, it is inherited in an autosomal recessive pattern. This means a person must inherit two copies of the mutated HBB gene, one from each parent, to develop the disease.
Can I get sickle cell disease from one parent?
No, you can’t get sickle cell disease from just one parent. You need two copies of the mutated gene, one from each parent, to develop the disease. If you inherit only one copy, you have sickle cell trait.
What is the difference between sickle cell trait and sickle cell disease?
Sickle cell trait happens when a person has one normal and one mutated HBB gene. Sickle cell disease occurs when a person has two mutated HBB genes. People with sickle cell trait usually don’t show symptoms, while those with sickle cell disease face many complications.
How is sickle cell disease diagnosed?
It’s diagnosed through newborn screening, genetic testing, or prenatal diagnosis. Newborn screening uses a blood test to detect abnormal hemoglobin. Genetic testing can find the mutated HBB gene.
What are the symptoms of sickle cell disease?
Symptoms include acute pain crises, anemia, infections, and chronic complications like organ damage and stroke. Children may also experience delayed growth and development.
How is sickle cell disease treated?
Treatment includes pain management, blood transfusions, and antibiotics. Curative options like stem cell transplantation and gene therapy are also available. Preventive care and lifestyle changes help manage the disease.
Can sickle cell disease be prevented?
While it can’t be prevented, genetic counseling and family planning help families understand their risk. This way, they can make informed decisions about having children.
Who is at risk for sickle cell disease?
People of African, Caribbean, and Middle Eastern descent are more likely to have it. Those with a family history of the disease are also at higher risk.
Is sickle cell disease contagious?
No, it’s not contagious. It’s a genetic disorder passed down from parents.
How can I manage sickle cell disease?
Managing it involves lifestyle changes like staying hydrated and avoiding extreme temperatures. It also means navigating healthcare systems and finding support resources.
What is the role of genetic counseling in sickle cell disease?
Genetic counseling helps families understand their risk of having a child with sickle cell disease. It provides guidance on family planning options.
References
- National Heart, Lung, and Blood Institute. (2024, March 15). Sickle cell disease. Retrieved from https://www.nhlbi.nih.gov/health/sickle-cell-disease