Last Updated on October 21, 2025 by mcelik

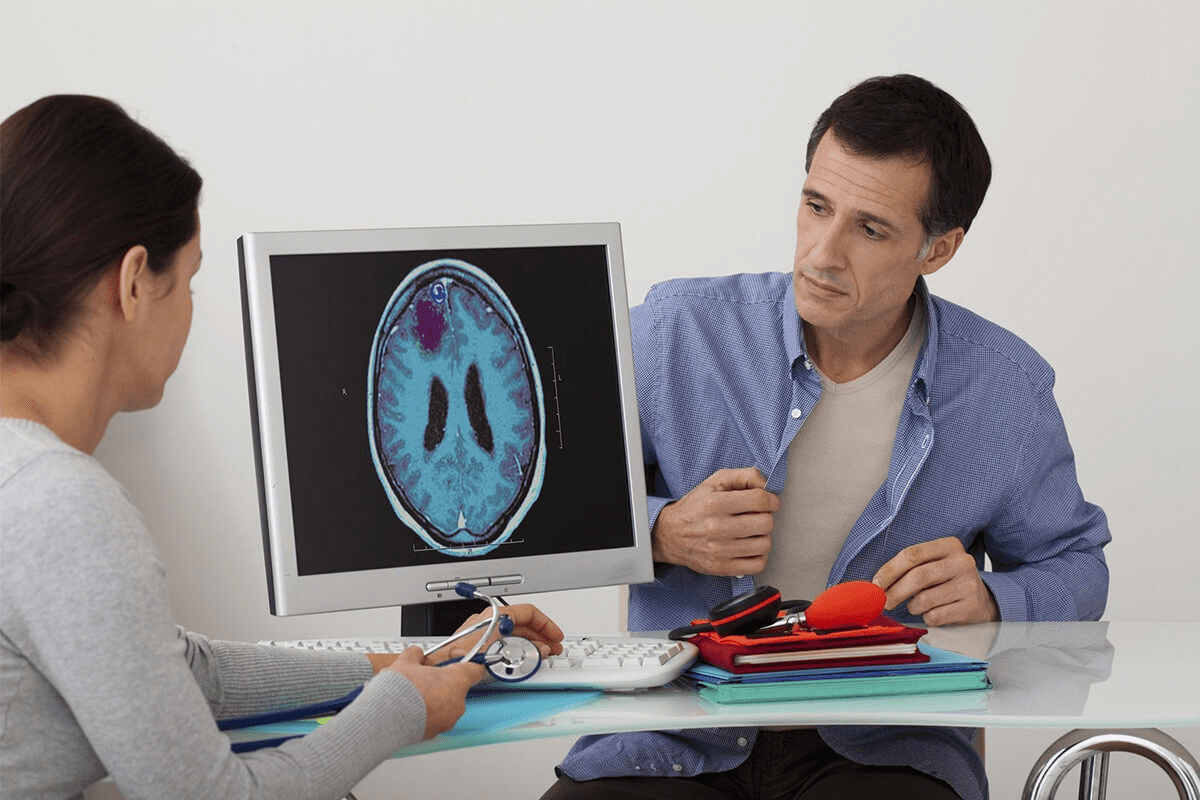
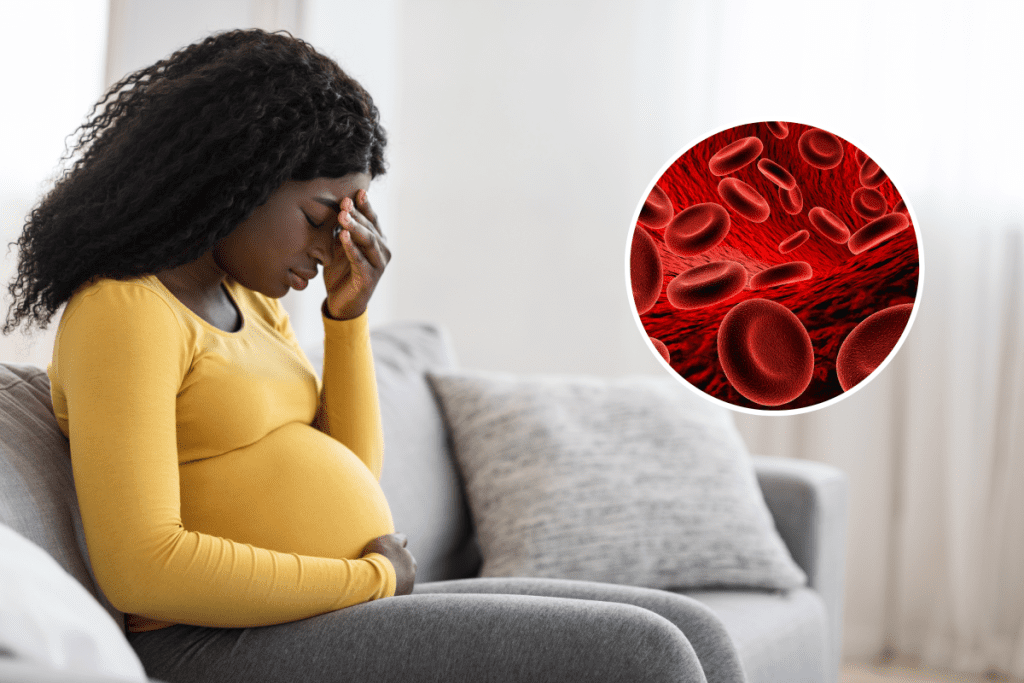
About 15-20% of pregnant women in the U.S. have iron deficiency anemia. Anemia lack of blood means they have low hemoglobin levels, which reduces the blood’s ability to carry oxygen to the body’s tissues. It’s key to know how to handle anemia during pregnancy because it can cause fatigue, weakness, and other complications that affect both the mother and baby. Proper diagnosis and treatment, including iron supplements and dietary changes, help manage anemia and promote healthy pregnancy outcomes.
.
Anemia can cause serious health issues for both mom and baby if not treated. It’s vital for pregnant women to know the iron deficiency symptoms and treatment choices.
This guide will help expectant mothers understand anemia’s causes, symptoms, and treatments. It aims to give them the tools to have a healthy pregnancy.
Key Takeaways
- Understanding the risks associated with anemia in pregnancy.
- Recognizing the symptoms of iron deficiency in pregnant women.
- Exploring treatment options for low hemoglobin during pregnancy.
- The importance of prenatal care in managing anemia.
- Nutritional advice to prevent and treat anemia.
Understanding Anemia During Pregnancy
It’s important for pregnant women to know about anemia. Pregnancy brings big changes in the body, including blood volume and composition. These changes can cause anemia.
Normal Blood Changes in Pregnancy
Pregnancy makes a woman’s blood volume grow a lot. This is to support the growing fetus and prepare for delivery. But, it can also lead to a type of anemia where red blood cells and hemoglobin levels drop. This is a normal change, but it can sometimes become a serious problem.
Definition of Anemia in Pregnancy
Anemia in pregnancy is when hemoglobin levels are too low. The World Health Organization says it’s less than 11 g/dL in the first and third trimesters. In the second trimester, it’s less than 10.5 g/dL. Hemoglobin is a key protein in red blood cells that carries oxygen.
Prevalence and Significance
Anemia is a big health issue, and pregnant women are at high risk. It’s thought that nearly a quarter of the world’s population is anemic, with pregnant women being most affected. Anemia can lead to serious problems for both the mother and the baby, including preterm labor and low birth weight.
| Trimester | Normal Hemoglobin Level (g/dL) | Anemia Threshold (g/dL) |
| First | >11 | |
| Second | >10.5 | |
| Third | >11 |
Anemia Lack of Blood: What It Means for Pregnant Women

The term ‘anemia lack of blood’ is often misunderstood. It’s not just about the amount of blood but its quality too. During pregnancy, the body changes a lot. These changes affect how well the blood carries oxygen.
The Role of Red Blood Cells and Hemoglobin
Red blood cells carry oxygen to the body’s parts. Hemoglobin is the protein in these cells that binds to oxygen. In pregnancy, the demand for oxygen increases for both the mother and the fetus. Low hemoglobin levels mean the body’s tissues and organs don’t get enough oxygen.
How Pregnancy Affects Blood Volume
Pregnancy increases blood volume by about 40-50%. This is needed to meet the oxygen and nutritional needs of the mother and fetus. It also prepares the mother’s body for blood loss during delivery. But, if red blood cell production doesn’t keep up, it can cause dilutional anemia. This is when the hemoglobin in the blood is lower than normal.
- Blood volume expansion supports the mother’s and fetus’s needs.
- Increased red blood cell production is necessary to avoid anemia.
- Dilutional anemia can occur if red blood cell production doesn’t match blood volume expansion.
Impact on Mother and Baby
Anemia during pregnancy can affect both the mother and the baby. For the mother, it can cause fatigue, shortness of breath, and a decreased ability to tolerate blood loss during delivery. For the baby, it can lead to preterm birth, low birth weight, and affect their iron stores after birth.
- Maternal anemia can cause fatigue and decreased tolerance to blood loss.
- It can lead to preterm birth and low birth weight in the baby.
- Affecting the baby’s iron stores and potentially their health after birth.
Understanding anemia during pregnancy is key. It shows why monitoring and managing this condition is so important. It ensures the best outcomes for both mother and baby.
Types of Anemia Commonly Seen in Pregnancy
Pregnant women face several types of anemia, which can affect their health. Anemia in pregnancy comes from nutritional deficiencies, health issues, or other factors.
Iron Deficiency Anemia
Iron deficiency anemia is the most common in pregnancy. It happens when the body lacks iron for hemoglobin, a key protein in red blood cells. Symptoms include fatigue, weakness, and shortness of breath. It can be due to not enough iron in the diet, increased iron needs during pregnancy, or chronic blood loss.
Folate Deficiency Anemia
Folate deficiency anemia is another common issue. Folate, or vitamin B9, is vital for making red blood cells. A lack of folate leads to anemia with large red blood cells. Folate supplements are often advised during pregnancy to prevent this, as folate also helps prevent neural tube defects in the fetus.
Vitamin B12 Deficiency Anemia
Vitamin B12 is key for making red blood cells and keeping the nervous system healthy. A B12 deficiency causes anemia with large red blood cells and neurological issues. Pregnant women on strict vegetarian or vegan diets are at higher risk due to missing animal products.
“Vitamin B12 deficiency is a significant concern in pregnancy, particular among women with dietary restrictions. Ensuring adequate intake through diet or supplementation is critical.”
Hemolytic Anemia
Hemolytic anemia happens when red blood cells are destroyed too quickly. It can be caused by infections, medications, or inherited conditions. During pregnancy, it poses risks to both mother and fetus, requiring careful management.
Knowing about the different anemias in pregnancy is key for diagnosis and treatment. Each type has its causes, symptoms, and health impacts on the mother and baby.
Risk Factors for Developing Anemia During Pregnancy
Several factors can increase the risk of developing anemia during pregnancy. It’s important to identify and manage these early. Anemia can be caused by pre-existing medical conditions, dietary factors, and pregnancy-related circumstances.
Pre-existing Conditions
Women with pre-existing medical conditions are at a higher risk of developing anemia during pregnancy. Conditions like sickle cell disease, thalassemia, and chronic diseases can increase this risk. Women who have experienced heavy menstrual bleeding before pregnancy are also more likely to develop anemia.
Dietary Factors
Diet plays a big role in the development of anemia during pregnancy. A diet lacking essential nutrients, like iron, folate, and vitamin B12, can significantly increase the risk. Vegetarians and vegans are at a higher risk because they get less iron and vitamin B12 from animal sources.
Multiple Pregnancies
Women carrying twins or multiple fetuses have a higher demand for iron and other nutrients. This increases their risk of developing anemia. The increased blood volume and nutrient demands can exacerbate the risk.
Age-Related Risks
Pregnant women under 20 years old or over 35 years old are at a higher risk of developing anemia. Teenage pregnancies have additional nutritional demands due to the mother’s own growth and development needs. Older pregnant women may have pre-existing conditions or decreased physiological reserve, contributing to the risk.
| Risk Factor | Description | Impact on Pregnancy |
| Pre-existing Conditions | Sickle cell disease, thalassemia, chronic diseases | Increased risk of anemia |
| Dietary Factors | Lack of iron, folate, vitamin B12 | Higher risk of anemia, specially in vegetarians/vegans |
| Multiple Pregnancies | Twins or multiple fetuses | Increased demand for iron and nutrients |
| Age-Related Risks | Under 20 or over 35 years old | Higher risk due to additional demands or decreased physiological reserve |
Signs and Symptoms of Anemia in Pregnancy
Anemia symptoms can be hard to spot, but catching them early is key for mom and baby’s health. Anemia in pregnancy shows up in different ways. So, it’s important for pregnant women to know the signs.
Common Physical Symptoms
Pregnant women with anemia might feel fatigue, weakness, and shortness of breath. This is because their bodies don’t get enough oxygen. This is due to not enough red blood cells or hemoglobin.
They might also feel dizzy, lightheaded, have cold hands and feet, or pale skin. Sometimes, anemia can cause a rapid heartbeat or palpitations.
Psychological Manifestations
Anemia can also affect a pregnant woman’s mind. The brain gets less oxygen, leading to irritability, anxiety, and depression. These feelings can be tough during pregnancy, when mood swings are common.
Distinguishing Anemia Symptoms from Normal Pregnancy Changes
It’s hard to tell if anemia symptoms are from pregnancy or anemia. Symptoms like fatigue and shortness of breath happen in pregnancy for other reasons too.
But, if these symptoms are severe or keep coming back, see a doctor. They can check if you have anemia and suggest treatment.
Diagnostic Tests for Anemia in Pregnancy
Diagnosing anemia in pregnancy involves several blood tests. These tests help doctors find and treat anemia accurately.
Complete Blood Count (CBC)
A Complete Blood Count (CBC) is key in diagnosing anemia. It checks the blood for red and white cells, hemoglobin, and platelets. This test shows how severe and what type of anemia a person has.
Key components of CBC relevant to anemia diagnosis:
- Red Blood Cell Count (RBC): Measures the number of red blood cells.
- Hemoglobin (Hb): Measures the amount of hemoglobin in the blood.
- Hematocrit (Hct): Measures the proportion of blood volume made up by red blood cells.
Hemoglobin and Hematocrit Levels
Hemoglobin and hematocrit levels are vital for diagnosing anemia. Low hemoglobin means less oxygen to tissues, showing anemia. Hematocrit shows the red blood cell percentage in the blood. These levels are watched closely during pregnancy to spot anemia.
| Parameter | Normal Range in Pregnancy | Indicative of Anemia |
| Hemoglobin (g/dL) | 11-16 g/dL (varies by trimester) | <11 g/dL |
| Hematocrit (%) | 33-44% (varies by trimester) | <33% |
The American College of Obstetricians and Gynecologists (ACOG) says anemia is diagnosed when hemoglobin is below the normal range for pregnancy.
Additional Blood Tests
Other blood tests are done to find anemia’s cause. These include:
- Iron studies: To check for iron deficiency.
- Folate and Vitamin B12 levels: To find deficiencies that cause anemia.
- Reticulocyte count: To see how well the bone marrow is working.
These tests are essential for finding anemia in pregnancy. They help doctors create the right treatment plans.
Iron Supplementation for Treating Anemia in Pregnancy
Iron supplements are key in treating anemia during pregnancy. Anemia lowers the red blood cell count or hemoglobin level. This can harm both the mother and the baby. Iron supplements boost iron levels, helping make more red blood cells.
Types of Iron Supplements
There are many iron supplements for pregnant women. The most common ones are:
- Ferrous Sulfate: It’s often prescribed because it’s effective and affordable.
- Ferrous Gluconate: It’s gentler on the stomach, making it a good choice for those with side effects.
- Ferrous Fumarate: It’s recommended for women with severe iron deficiency.
- Iron Complex Supplements: These combine iron with nutrients like folic acid and vitamin B12. They help with absorption and address other deficiencies.
Recommended Dosages
The right amount of iron varies based on anemia’s severity and individual needs. Usually:
- For mild anemia, 30-60 mg of elemental iron daily is recommended.
- For severe cases, a healthcare provider may prescribe higher doses.
It’s important to follow your healthcare provider’s advice. This ensures effective treatment and reduces side effects.
Managing Side Effects
Iron supplements are vital but can cause side effects like constipation, nausea, and stomach cramps. To handle these:
- Take supplements with food: This can lessen stomach side effects.
- Increase fluid and fiber intake: This helps with constipation.
- Consider alternative forms of iron: If side effects are bad, talk to your healthcare provider about switching to a different type.
Duration of Supplementation
How long you need iron supplements depends on anemia’s severity and how well you respond to treatment. Generally:
- Treatment goes on until hemoglobin levels get back to normal.
- Supplementation might continue for months after pregnancy to refill iron stores.
It’s vital to have regular check-ups with your healthcare provider. They will help figure out how long you need supplements.
Other Nutritional Supplements for Anemia Treatment
Iron supplements are not the only answer for anemia during pregnancy. Other supplements are key to treating anemia and keeping mom and baby healthy.
Folic Acid Supplements
Folic acid is vital for preventing and treating folate deficiency anemia in pregnancy. Folic acid supplements are recommended to prevent birth defects of the brain and spine.
The daily dose for pregnant women is 600 to 800 micrograms. Women with a history of anemia or other issues might need more, as advised by their doctor.
Vitamin B12 Supplements
Vitamin B12 is also essential for preventing anemia. Vitamin B12 deficiency can cause anemia, fatigue, and neurological problems. Pregnant women, and those on vegetarian or vegan diets, are at higher risk.
Vitamin B12 can be taken orally or by injection, depending on the deficiency and the patient’s health.
Vitamin C for Iron Absorption
Vitamin C helps iron absorption, making it great for pregnant women with anemia. Eating foods high in vitamin C (like citrus fruits, strawberries, and bell peppers) with iron-rich foods boosts iron supplement effectiveness.
| Vitamin C Rich Foods | Iron Rich Foods |
| Oranges | Red meat |
| Strawberries | Spinach |
| Bell Peppers | Legumes |
Supplement Interactions and Safety
While supplements are helpful, knowing about interactions and safety is key. Pregnant women should talk to their doctor before starting any new supplements. This is to avoid bad reactions with other medicines or worsening health conditions.
For example, calcium supplements can reduce iron absorption, so take them at different times. Some antibiotics can also cut down iron supplement effectiveness.
Dietary Approaches to Treating Anemia in Pregnancy
A well-balanced diet is key in treating anemia in pregnant women. Anemia means not enough healthy red blood cells to carry oxygen. Adding certain nutrients and foods can boost hemoglobin levels and health.
Iron-Rich Foods
Iron is vital for preventing and treating anemia. Pregnant women should eat foods rich in iron, such as:
- Red meat
- Poultry
- Fish
- Legumes (lentils, chickpeas, black beans)
- Leafy greens (spinach, kale)
- Nuts and seeds (pumpkin seeds, sesame seeds)
- Fortified cereals
Eating more of these foods can meet the iron needs during pregnancy. Cooking in cast-iron cookware also helps, as it increases iron intake, mainly with acidic foods like tomatoes.
Foods That Enhance Iron Absorption
Some foods can improve iron absorption, making diet more effective. These include:
- Foods high in vitamin C (citrus fruits, bell peppers, tomatoes)
- Foods containing heme iron (animal sources like meat, poultry, and fish)
Eating these foods with iron-rich foods can greatly improve iron absorption. For instance, orange juice with a meal can help absorb non-heme iron better.
Foods to Avoid When Anemic
Some foods can reduce iron absorption or make anemia worse. Pregnant women should limit or avoid:
- Caffeine (found in coffee, tea, and some soft drinks)
- Calcium-rich foods and supplements (dairy products, fortified plant-based milk)
- Foods high in phytates (whole grains, legumes, nuts)
Staying away from these foods or eating them apart from iron-rich foods can improve iron absorption. It’s wise to talk to a healthcare provider or dietitian for tailored advice.
By choosing the right foods, pregnant women can manage anemia well. This ensures better health for both mother and baby.
Medical Treatments for Severe Anemia in Pregnancy
Medical treatments are key in managing severe anemia in pregnancy. They help keep both the mother and the fetus safe. When anemia is severe, doctors often suggest several treatments to quickly improve the patient’s health.
Intravenous Iron Therapy
Intravenous iron therapy is a top choice for severe iron deficiency anemia. It gives iron straight into the blood, skipping the stomach. This is great for pregnant women who can’t take oral iron or haven’t seen results from it.
Benefits of intravenous iron therapy include:
- Rapid increase in iron levels
- Improved hemoglobin production
- Reduced need for blood transfusions
Blood Transfusions
When anemia is very severe or the fetus is in distress, blood transfusions might be needed. These transfusions add blood to the patient’s system. This quickly boosts red blood cells and helps oxygen reach the fetus.
While blood transfusions are generally safe, they are typically reserved for emergency situations or when other treatments have failed.
Erythropoietin Treatment
Erythropoietin is a hormone that helps make more red blood cells. For severe anemia, erythropoietin treatment might be considered, mainly when other options don’t work.
The use of erythropoietin during pregnancy is closely watched. There are risks and benefits that need careful consideration.
These treatments for severe anemia in pregnancy show how important quick and effective care is for expectant mothers. Healthcare providers can tailor treatments to each patient’s needs. This ensures the best outcomes for both mother and baby.
Cultural Considerations and Traditional Remedies
Treating anemia in pregnancy goes beyond just medicine. Cultural practices and traditional remedies are also key. They offer insights into caring for expectant mothers with anemia.
Diverse Approaches Across Cultures
Every culture has its own ways to fight anemia in pregnancy. Some use herbal teas and special diets to boost iron. Healthcare providers must respect these practices to care for patients fully.
In Asian cultures, foods like dark leafy greens, dates, and red meat are good for iron. African cultures might use herbal remedies for anemia.
Evidence-Based Traditional Remedies
It’s important to know which traditional remedies work. Some have been proven to help with anemia. For example, certain teas can improve iron absorption.
- Foods rich in folate, like those in many cultures, help prevent folate deficiency anemia.
- Vitamin C foods, eaten in many cultures, help iron absorption when paired with iron-rich foods.
Integrating Conventional and Traditional Care
Doctors are now mixing modern medicine with traditional remedies. This makes care more satisfying and effective. It makes treatment fit better with each patient’s culture.
Understanding cultural differences helps doctors create better treatment plans. They might add traditional diets or herbal remedies, if they’re safe and backed by science.
Managing Anemia Throughout Each Trimester
Managing anemia during pregnancy is a big job that needs focus in each trimester. As the pregnancy goes on, the body needs more iron and nutrients. It’s important to change how we manage anemia as needed.
First Trimester Considerations
In the first trimester, we need to lay the groundwork for managing anemia. This means:
- Starting with blood tests to see if there’s anemia
- Looking at what you eat and suggesting iron-rich foods
- Talking about if you need iron supplements
Early action is key to handling anemia well during pregnancy.
Second Trimester Adjustments
In the second trimester, the body needs more iron because of the growing red blood cells and the baby. Important steps include:
- Upgrading iron supplements if blood tests show you need more
- Watching for signs of anemia like tiredness and short breath
- Changing your diet to include foods that help your body absorb iron better, like vitamin C-rich foods
This trimester is also when we need to watch for other nutritional gaps that could make anemia worse.
Third Trimester Challenges
In the third trimester, anemia risks go up because of the increased need for iron and nutrients. Challenges include:
- Dealing with symptoms like dizziness and heart racing that can get worse with anemia
- Making sure you get enough iron from food and supplements
- Getting ready for possible medical help like IV iron or blood transfusions if anemia is severe
Preparing for Labor and Delivery
As the due date gets closer, it’s vital to keep anemia in check for a healthy birth. Things to think about include:
- Getting your hemoglobin levels up before labor to lower risks
- Talking with your healthcare team about managing anemia during and after labor
- Knowing the signs of anemia that might need quick medical help during and after delivery
Good management of anemia all through pregnancy, and getting ready for labor and delivery, is essential for a good birth outcome.
Potential Complications of Untreated Anemia in Pregnancy
Anemia can harm pregnant women and their babies if not treated. It’s important for expectant mothers to know these risks. This way, they can get the care they need.
Risks to the Mother
Untreated anemia can cause problems for the mother, including:
- Increased risk of preterm labor: Anemic women are more likely to have preterm labor. This can cause problems for both the mother and the baby.
- Higher risk of postpartum hemorrhage: Anemia can make severe bleeding after delivery more likely. This is a big cause of death for mothers worldwide.
- Cardiac complications: Severe anemia can cause heart problems. The heart works harder without enough red blood cells, which can lead to heart failure.
A study in a medical journal found that anemia in pregnancy increases the risk of problems for both the mother and the baby. It’s important to find and treat anemia early.
“Anemia is a big public health problem, mainly for pregnant women. Its effects can be serious if not managed well.”
Risks to the Baby
The baby also faces risks if the mother has untreated anemia:
- Low birth weight: Babies of anemic mothers are more likely to be underweight. This increases the risk of death and health problems later on.
- Preterm birth: Anemia also raises the risk of preterm birth. This can lead to health issues for the baby.
- Potential developmental issues: Some studies suggest that anemic mothers may have children with developmental delays or cognitive problems.
Long-term Health Implications
Untreated anemia during pregnancy can affect health long after the pregnancy:
- Persistent health issues: Women with anemia during pregnancy may face ongoing health problems after giving birth. This can include anemia or related conditions.
- Impact on future pregnancies: Having anemia during pregnancy can increase the risk of anemia in future pregnancies. This creates a cycle that needs to be broken.
In conclusion, untreated anemia in pregnancy is a serious issue for both the mother and the baby. It can lead to long-term health problems. Pregnant women need to be checked for anemia and treated to avoid these risks.
Preventing Anemia Before and During Pregnancy
Preventing anemia is a big job that starts before a woman gets pregnant and goes on during her pregnancy. It involves good nutrition before getting pregnant, taking the right supplements, and living a healthy lifestyle. These steps can greatly lower the chance of a woman getting anemia while she’s expecting.
Preconception Nutrition
Eating right before getting pregnant is key to avoiding anemia later. It’s important to eat foods high in iron, folate, and vitamin B12. Foods like red meat, beans, and fortified cereals are good sources of iron. Leafy greens, legumes, and citrus fruits are full of folate. And, vitamin B12 is found in animal products like meat, poultry, fish, and dairy.
Nutritional Tips:
- Eat more foods high in iron.
- Add folate-rich foods to your meals.
- Make sure to get enough vitamin B12 from animal products or supplements.
Preventive Supplementation
Along with a healthy diet, taking supplements can also help prevent anemia. Pregnant women often need iron supplements, and those at risk should definitely take them. Folic acid supplements are also important to stop folate deficiency anemia.
| Supplement | Recommended Dosage | Purpose |
| Iron | 30 mg per day | Prevent iron deficiency anemia |
| Folic Acid | 600-800 mcg per day | Prevent folate deficiency anemia |
| Vitamin B12 | 2.6 mcg per day | Prevent vitamin B12 deficiency anemia |
Lifestyle Factors
How you live your life also affects your risk of anemia. Drinking too much caffeine and tea can hurt iron absorption. But, cooking in cast-iron cookware can help increase iron intake, even more so if you cook acidic foods like tomatoes.
Additional Tips:
- Don’t drink tea or coffee with meals.
- Use cast-iron cookware.
- Keep a healthy diet and lifestyle.
When to Seek Medical Help for Anemia During Pregnancy
It’s important for pregnant women with anemia to get medical help on time. This ensures their health and the baby’s well-being. Anemia can cause problems for both the mother and the fetus if not treated right.
Warning Signs That Require Immediate Attention
Pregnant women need to know the warning signs that mean they should see a doctor right away. These include:
- Severe fatigue that makes it hard to do daily tasks
- Shortness of breath or trouble breathing
- Dizziness or feeling like you’re going to pass out
- Rapid heartbeat or feeling your heart beat fast
- Pale skin or jaundice
Spotting these signs early is important for managing anemia and avoiding complications.
Regular Monitoring Schedule
It’s key to keep an eye on anemia during pregnancy. Pregnant women should follow this schedule:
- Go to all prenatal check-ups as your healthcare provider tells you to
- Get blood tests to check your hemoglobin levels and other important things
- Tell your healthcare provider right away if you notice any new or getting worse symptoms
Questions to Ask Your Healthcare Provider
Pregnant women with anemia should ask their healthcare provider important questions. Some examples are:
- What’s the best way to handle anemia during pregnancy?
- Are there any food changes that can help my condition?
- What risks could anemia pose to my baby and me?
- How often should I have my blood tested?
Building Your Medical Support Team
It’s vital for pregnant women with anemia to have a strong medical support team. This team might include:
- Obstetricians or maternal-fetal medicine specialists
- Nutritionists or dietitians for food advice
- Other healthcare professionals as needed
Having a wide support team makes sure all care needs are met. This brings peace of mind and the best results.
Postpartum Anemia: Continued Care After Delivery
The time after having a baby is very important for new moms. They might face the risk of postpartum anemia. This is when there’s not enough red blood cells or hemoglobin, affecting their health and recovery.
Risk Factors for Postpartum Anemia
There are several things that can make a mom more likely to get postpartum anemia. These include:
- Excessive blood loss during delivery
- Pre-existing anemia during pregnancy
- Multiple pregnancies (twins, triplets, etc.)
- Poor nutrition and inadequate iron intake
Knowing these risk factors helps in catching and treating postpartum anemia early.
Treatment Approaches
Dealing with postpartum anemia usually means fixing the cause and adding iron. Here are some ways to do it:
- Iron Supplementation: Oral iron supplements are often prescribed to treat iron deficiency anemia.
- Dietary Changes: Eating more iron-rich foods and vitamin C can help iron absorption.
- Intravenous Iron Therapy: In severe cases, intravenous iron may be given.
Doctors might also suggest other nutritional supplements based on what each woman needs.
Recovery Timeline
How long it takes to get better from postpartum anemia depends on how bad it is and the treatment. Most women start feeling better in a few weeks. But, it can take months for iron levels to get back to normal.
It’s very important to keep seeing your healthcare provider. They can check how you’re doing and change your treatment if needed.
Conclusion
Treating anemia in pregnancy is key for the health of both mom and baby. It’s important for expectant mothers to know the causes, symptoms, and how to treat it. This knowledge helps them manage their condition well.
Anemia in pregnancy can come from iron, folate, or vitamin B12 deficiencies. To treat it, a mix of supplements, diet changes, and sometimes medical help is needed. This approach helps manage anemia effectively.
By being proactive about anemia, pregnant women can lower the risk of problems. Regular check-ups with healthcare providers are also essential. They help keep anemia under control.
In short, treating anemia in pregnancy needs a plan that includes education, nutrition advice, and medical care. Understanding and tackling anemia is a big step towards a healthy pregnancy and a happy baby.
FAQ
What is anemia in pregnancy?
Anemia in pregnancy means you have fewer red blood cells or less hemoglobin. This makes it hard for your body and your baby’s to get enough oxygen.
How common is anemia during pregnancy?
Anemia is quite common in pregnancy. It affects many women, mostly in low-income countries.
What are the symptoms of anemia in pregnancy?
Symptoms include feeling very tired, weak, and pale. You might also get short of breath, dizzy, or have headaches. These symptoms can be hard to tell apart from normal pregnancy feelings.
How is anemia diagnosed during pregnancy?
Doctors use a complete blood count (CBC) test to find anemia. This test checks your hemoglobin and hematocrit levels.
What are the risks of untreated anemia during pregnancy?
If anemia isn’t treated, it can lead to serious problems. These include preterm labor, low birth weight, and health issues for both mom and baby.
How is anemia treated during pregnancy?
Treatment usually includes iron supplements and eating more iron-rich foods. Sometimes, folic acid and vitamin B12 are also given.
Can anemia be prevented during pregnancy?
Yes, you can prevent or lower the risk of anemia. Eating iron-rich foods and taking supplements before getting pregnant helps. Avoid foods that block iron absorption too.
What are the signs that I should seek medical help for anemia during pregnancy?
Seek help if you’re extremely tired, dizzy, or have trouble breathing. Heavy bleeding is also a sign to see a doctor. Always follow your healthcare provider’s monitoring schedule.
Can anemia continue after pregnancy?
Yes, anemia can stick around after pregnancy, known as postpartum anemia. It needs ongoing care and treatment to avoid complications.
How is postpartum anemia treated?
Treatment for postpartum anemia includes iron supplements. In severe cases, blood transfusions might be needed.
What are the long-term implications of anemia during pregnancy?
Anemia during pregnancy can lead to ongoing health problems. These include infections, poor brain development in kids, and lasting fatigue in moms.
Are there any cultural or traditional remedies for anemia during pregnancy?
Yes, many cultures have their own remedies for anemia. Some might help, but always talk to a doctor before trying them.
Reference
- Pavord, S., Daru, J., Prasannan, N., Robinson, S., Stanworth, S., Girling, J., & BSH Committee. (2020). UK guidelines on the management of iron deficiency in pregnancy. British Journal of Haematology, 188(6), 819“830. https://pubmed.ncbi.nlm.nih.gov/31960965/