Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.

Diagnosing cancer for surgery involves carefully mapping out where the tumor is and understanding its biology. This step turns the idea of “cancer” into a clear plan for surgery. It is very important because the choice to operate, the type of surgery, and the order of treatments all depend on getting the diagnosis and staging right. Diagnosis shows what kind of tumor it is, while staging tells where it is, how big it is, and if it has spread.
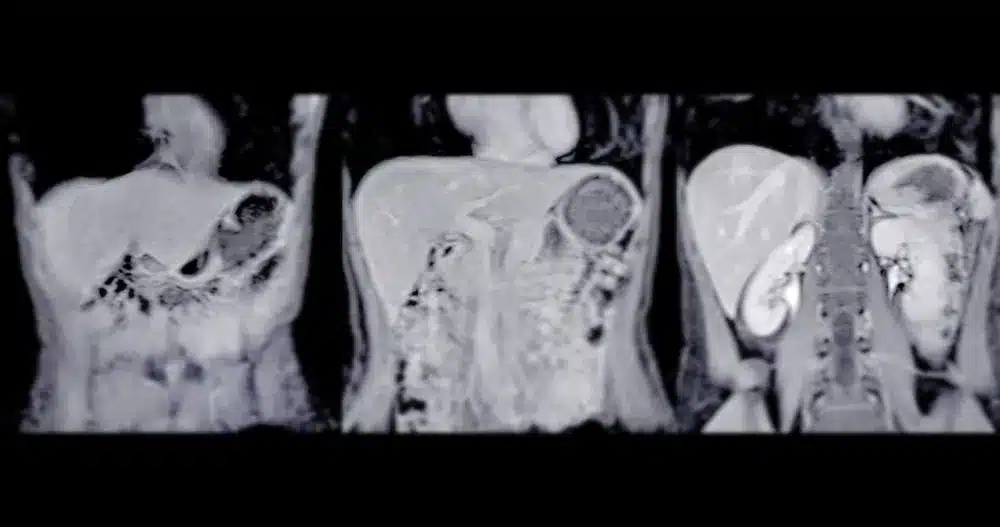
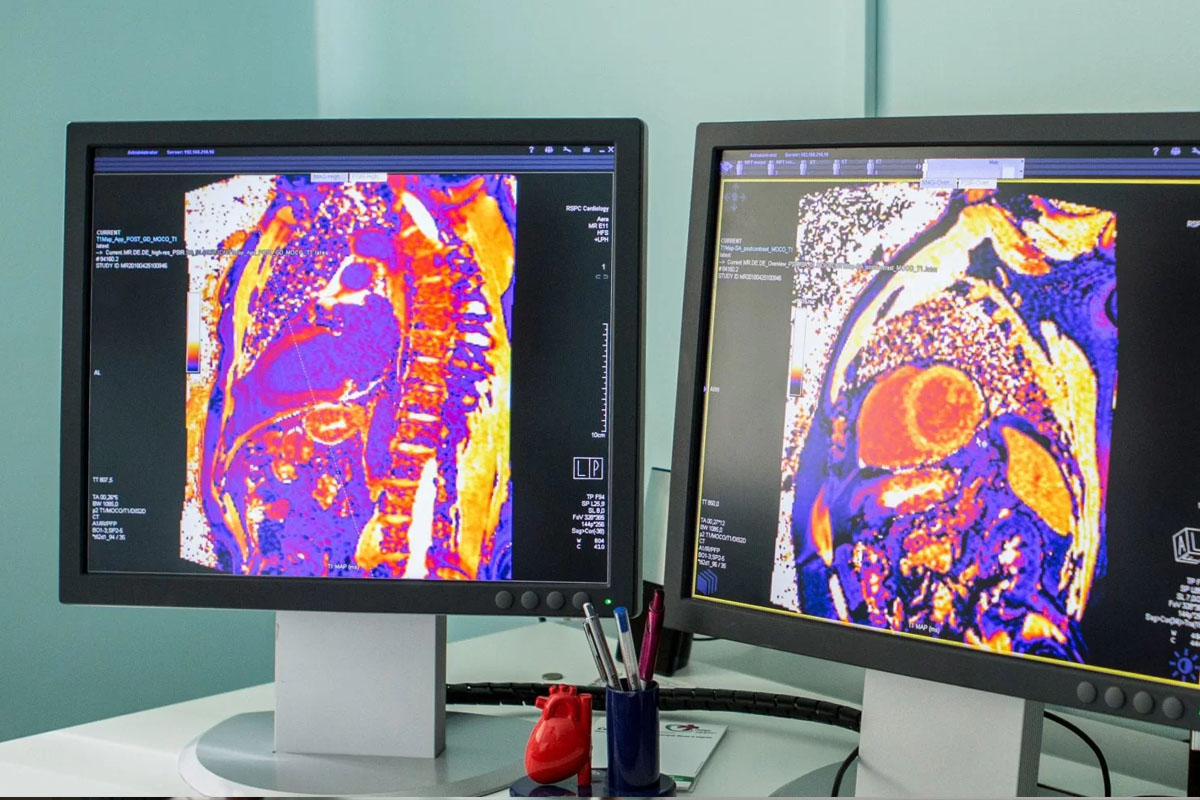
Modern diagnosis relies on a multimodal approach integrating advanced imaging, tissue sampling, and molecular profiling. The era of exploratory surgery, where a surgeon would open a patient to “look and see,” is largely obsolete. Today, the surgeon enters the operating room with a detailed 3D mental model of the tumor’s relationship to critical blood vessels and nerves, derived from high-resolution cross-sectional imaging. This preoperative visualization is essential for planning the resection margins and reconstruction strategy.

Computed Tomography (CT) remains the workhorse of oncologic staging, providing rapid, high-resolution images of the chest, abdomen, and pelvis. It is excellent for detecting lung and liver metastases and for defining the local extent of the primary tumor. However, Magnetic Resonance Imaging (MRI) offers superior soft tissue contrast, making it the modality of choice for brain tumors, sarcomas, rectal cancer, and pelvic malignancies. MRI allows the surgeon to visualize the interface between the tumor and the muscle or fascia, which is critical for limb-sparing or sphincter-sparing surgeries.
Positron Emission Tomography (PET) is a functional imaging modality. It uses a radiolabeled glucose analog (FDG) to identify cells with high metabolic activity. Since cancer cells consume glucose at a much higher rate than normal cells (the Warburg effect), they “light up” on the scan. PET/CT fusion images combine metabolic data with anatomical structure, allowing the surgeon to distinguish between active tumor and scar tissue and to detect small, distant metastases that might be missed on a standard CT scan. This metabolic staging is crucial for avoiding futile surgeries in patients who already have systemic disease.
The definitive diagnosis requires tissue. The biopsy technique is strategic; it must provide enough tissue for molecular testing without disrupting the tumor planes or seeding cancer cells along the needle track. Core needle biopsies are generally preferred over fine needle aspirations for this reason, as they preserve the tissue architecture. The pathologist then determines the tumor’s histological subtype and grade.
In the era of precision medicine, pathology reports include extensive molecular profiles. Testing for HER2 in breast and gastric cancer, KRAS in colorectal cancer, or BRAF in melanoma is standard. These biomarkers provide surgeons and oncologists with information about the tumor’s biological behavior. A highly aggressive, poorly differentiated tumor might be treated with chemotherapy first (neoadjuvant therapy) to shrink it and test its sensitivity. In contrast, a slow-growing, well-differentiated tumor might go straight to surgery.

Staging is codified using the TNM system: Tumor (size and extent), Node (lymph node involvement), and Metastasis (spread to distant organs). This standardized language allows surgeons worldwide to communicate the severity of disease. However, staging is evolving. We now have “Clinical Staging” based on scans and “Pathological Staging” based on what is actually found during surgery. The pathological stage is the most accurate predictor of prognosis.
Newer prognostic models integrate biological markers into the staging system. For example, a small breast cancer that is HER2 positive and hormone receptor negative is treated differently from a tumor of the same size with a different profile. The “Bio-staging” concept acknowledges that the genetic programming of the cell is as important as the tumor’s physical size. This helps the surgical oncologist determine whether surgery should be the first or last step in the treatment sequence.
Before major cancer surgery, the patient’s functional reserve must be evaluated. This is “physiological staging.” Cardiopulmonary exercise testing (CPET) measures the body’s ability to deliver oxygen to tissues under stress, mimicking the metabolic demand of surgery. A patient with poor functional capacity may not survive the recovery from a primary resection, even if the tumor is technically removable. In these cases, less invasive options or pre-habilitation (exercise and nutrition programs before surgery) are pursued to optimize the patient’s fitness.
Doctors also check the patient’s nutrition. Poor nutrition is common in cancer and can make it harder for wounds to heal and for the immune system to work. Blood tests and body measurements help decide if the patient needs extra nutrition before surgery. The aim is to make sure the patient has what they need to heal and recover from the stress of surgery.
Not every lump or mass is cancer. Doctors must rule out other conditions like certain infections, non-cancerous tumors, or inflammation that can look similar. They use advanced scans and special lab tests to tell the difference. Getting the diagnosis wrong can lead to unnecessary major surgery, so surgeons are careful to confirm cancer before doing any permanent procedures.

Send us all your questions or requests, and our expert team will assist you.
TNM stands for Tumor, Node, and Metastasis. “T” describes the size and extent of the primary tumor. “N” indicates whether the cancer has spread to nearby lymph nodes. “M” indicates if the cancer has spread to distant parts of the body. These scores are combined to assign an overall stage (0-IV), which guides treatment and prognosis.
PET scans detect high metabolic activity. While cancer cells are very active, so are cells involved in inflammation and infection. Therefore, an area of active healing, a localized infection, or even muscle strain can appear as a PET scan abnormality, mimicking cancer. Doctors use CT correlation and sometimes biopsy to distinguish between the two.
This is a procedure to identify the first lymph node(s) to which cancer cells are most likely to spread from a primary tumor. By injecting a tracer, the surgeon can find and remove only this “sentinel” node. If it is free of cancer, it is unlikely the cancer has spread further, allowing the patient to avoid the side effects of removing all the lymph nodes.
Neoadjuvant therapy is treatment given before the primary surgery. This usually involves chemotherapy or radiation. The goals are to shrink the tumor to make it easier to remove, to kill any microscopic cancer cells that may have spread, and to test how well the cancer responds to the drugs.
Resectability is determined by the tumor’s location and its relationship to vital structures. If a cancer encases major arteries that cannot be reconstructed or invades critical organs that cannot be spared, it may be deemed unresectable. The patient’s overall health and ability to survive the surgery and recovery are also significant factors in this decision.

Cancer metastasis is a complex process. It involves the spread of malignant tumors to other parts of the body. Knowing where cancer spreads first is
Lung cancer is a common cancer worldwide and has a high death rate, largely because it often metastasizes. Where lung cancer first spreads is key

Over 2 million PET scans are done every year in the U.S. to aid in tumor detection. These scans help find tumors and evaluate lung


Nearly 70 million ultrasound procedures happen every year in the United States. A big part of these are transvaginal ultrasounds for checking health. Many people
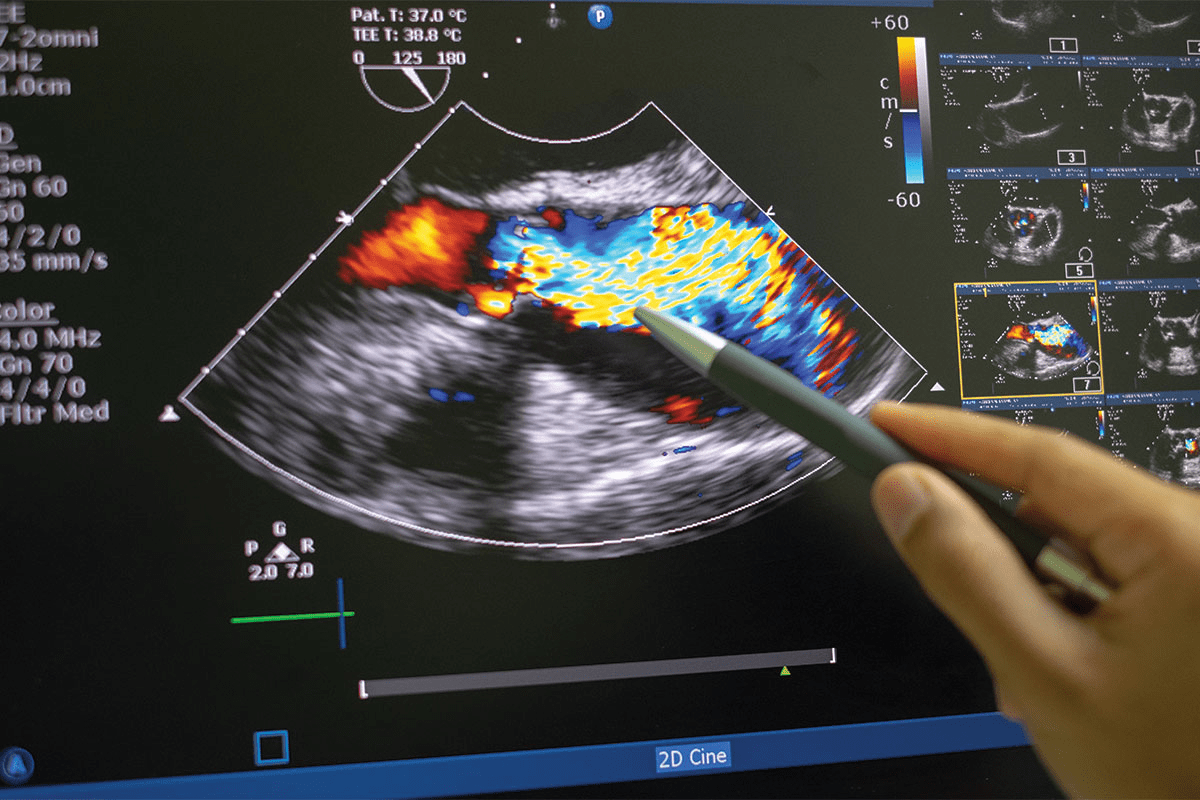
Ultrasound technology is key in finding cancers early. A recent study showed ultrasound can spot cancerous tumors very accurately. This change is big for cancer

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)