Ovarian cancer is a serious disease that often starts in the fallopian tubes or on the surface of the ovary. Studies show that high-grade serous ovarian cancer (HGSOC) usually comes from the fallopian tube cells.
It’s important to know where cancer starts to find it early and treat it well. We need to find where cancer begins to help patients more.
Key Takeaways
- Ovarian cancer often begins in the epithelial cells of the fallopian tubes.
- The ovarian surface is another common site for the initiation of ovarian cancer.
- High-grade serous ovarian cancer (HGSOC) is frequently linked to the fallopian tube epithelium.
- Early detection is critical for improving outcomes in ovarian cancer patients.
- Understanding the origins of ovarian cancer can lead to more effective treatment strategies.
The Nature and Significance of Ovarian Cancer
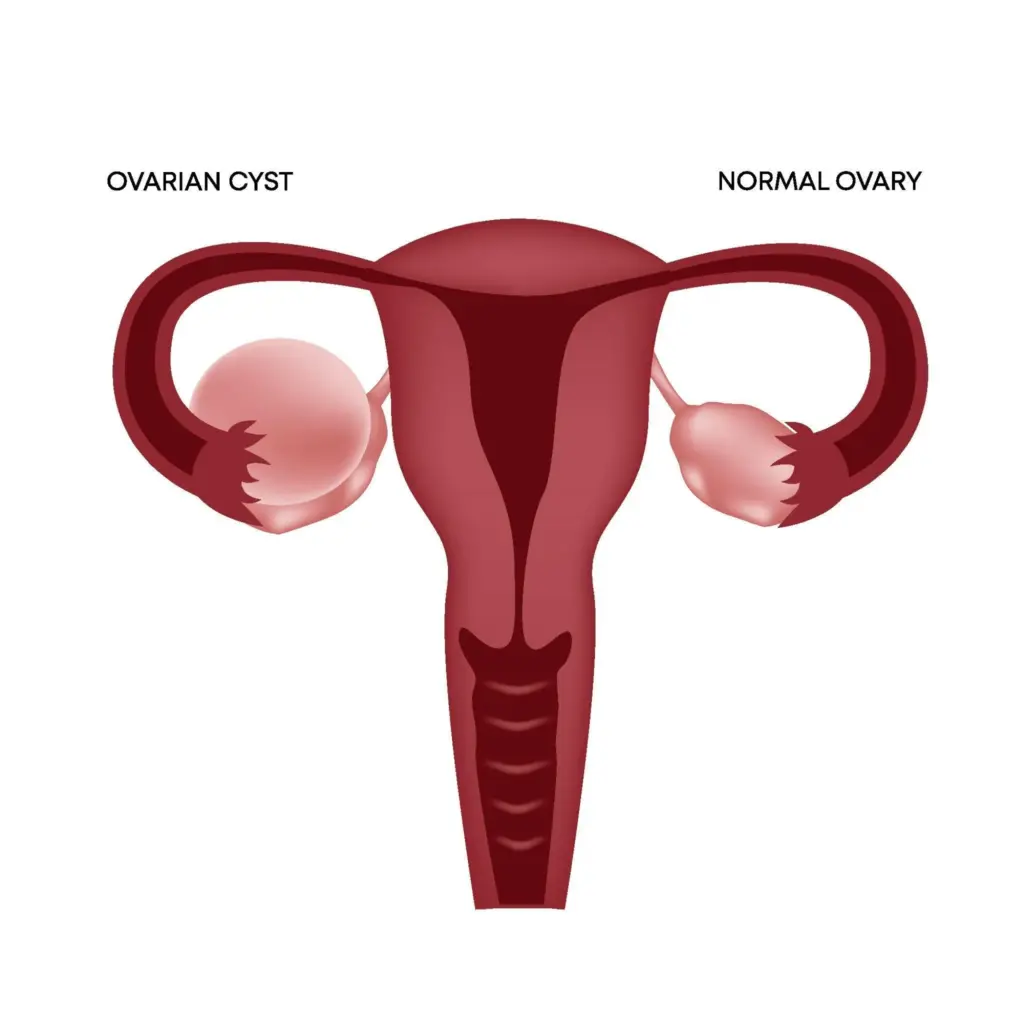
Learning about ovarian cancer is vital. It’s a cancer that affects the ovaries, key parts of the female body. The female reproductive anatomy includes the ovaries, fallopian tubes, uterus, cervix, and vagina. All these work together to keep reproductive health strong.
Definition and Female Reproductive Anatomy
Ovarian cancer starts in the ovaries, small organs by the uterus. Most ovarian cancers, over 90%, are epithelial ovarian cancer. They come from the outer layer of the ovary. Knowing about the ovarian cancer definition and its link to the female body is key to understanding how it grows and spreads.
The ovaries play several vital roles. They make eggs and hormones like estrogen and progesterone. These hormones are vital for the menstrual cycle and getting pregnant. The says epithelial ovarian cancer is the most common type. This shows why knowing about it is so important.
Why Understanding Cancer Origins Matters
Knowing where cancer comes from helps find better ways to diagnose and treat it. The start of ovarian cancer, mainly epithelial ovarian cancer, affects how well patients do. Studying where ovarian cancer comes from has led to new treatments and better survival rates.
“The more we understand about the origins and nature of ovarian cancer, the better equipped we are to combat this devastating disease.” It’s important to raise ovarian cancer awareness. This helps find cancer early and supports those dealing with it.
Evolution of Understanding: Historical vs. Current Knowledge

Ovarian cancer was once thought to start only in the ovaries. Now, we know it’s more complex. The old idea was that it came from the surface of the ovaries. But, our understanding has changed a lot over time.
Traditional Views on Ovarian Cancer Origins
People used to think ovarian cancer came from the surface of the ovaries or from cysts inside them. This idea came from looking at the ovaries and seeing cancerous spots.
The “incessant ovulation” hypothesis was also popular. It said that the constant ovulation caused damage to the ovarian surface. This damage could lead to cancer. But, it didn’t explain all types of ovarian cancer.
The Paradigm Shift in Scientific Understanding
New studies have changed how we see where ovarian cancer starts. Now, many believe that high-grade serous ovarian cancers (HGSOC) come from the fallopian tube epithelium, not the ovaries.
This change is based on several important findings:
- Scientists found precancerous lesions in the fallopian tubes, called serous tubal intraepithelial carcinomas (STICs).
- STICs and HGSOC share similar genes and molecular traits.
- Studies show that removing the fallopian tubes can lower ovarian cancer risk.
This new understanding is very important. It means we might be able to prevent some types of ovarian cancer by removing the fallopian tubes. It’s also leading to better ways to find cancer early and treat it more effectively.
|
Aspect |
Traditional View |
Current Understanding |
|---|---|---|
|
Primary Origin Site |
Ovarian Surface Epithelium |
Fallopian Tube Epithelium (for HGSOC) |
|
Cancer Development Theory |
Incessant Ovulation Hypothesis |
Multiple pathways, including STICs |
|
Preventive Measures |
Oophorectomy or Prophylactic Surgery |
Salpingectomy, Targeted Therapies |
Primary Sites Where Ovarian Cancer Develops
Recent studies have shed light on where ovarian cancer develops. Understanding these sites helps in comprehending the disease better and discovering new treatment options.
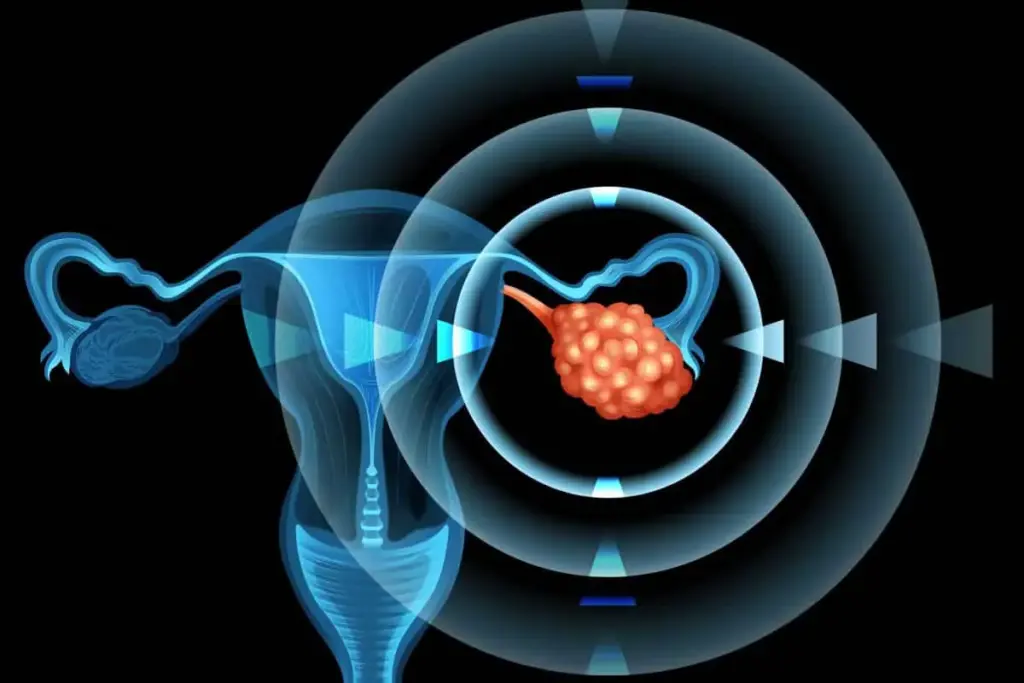
Fallopian Tube Epithelium as a Major Origin Site
The fallopian tube epithelium is a key place for ovarian cancer, mainly for high-grade serous ovarian cancer (HGSOC). Studies show that secretory cells in the fallopian tube can turn into serous tubal intraepithelial carcinomas (STICs). These are precursors to HGSOC.
Key findings about fallopian tube epithelium:
- Secretory cells are the primary cell type involved in STICs and HGSOC.
- The fallopian tube epithelium is a common site for early carcinogenic changes.
- Genetic mutations, such as TP53, are frequently observed in STICs and HGSOC.
Ovarian Surface Epithelium and Other Starting Points
While the fallopian tube epithelium is a major origin site, ovarian surface epithelium (OSE) and other structures within the ovary can also give rise to ovarian cancer. OSE is thought to be involved in the development of certain ovarian cancer subtypes, though its role is less clear than that of the fallopian tube epithelium.
Characteristics of ovarian surface epithelium:
|
Characteristics |
Description |
|---|---|
|
Cell Type |
Primarily composed of flat to cuboidal epithelial cells |
|
Function |
Covers the surface of the ovary, potentially involved in ovulation and repair processes |
|
Cancer Association |
Thought to be involved in the development of certain ovarian cancer subtypes |
Lesions in ovarian cancer can double in size approximately every 2.2 months, showing how aggressive this disease is. Knowing where ovarian cancer starts is key to finding early detection and treatment strategies.
Major Types of Ovarian Cancer
It’s important to know the different types of ovarian cancer for better treatment. Ovarian cancer is made up of various tumor types. Each type has its own cell of origin, look, and how it behaves.
Epithelial Ovarian Cancer (90% of Cases)
Epithelial ovarian cancer makes up about 90% of cases. It starts in the outer layer of the ovary or the fallopian tube. Epithelial ovarian cancer has several subtypes, like serous, mucinous, endometrioid, and clear cell carcinomas.
Serous carcinomas are the most common. They can be low-grade or high-grade. High-grade serous ovarian cancer is very aggressive and deadly.
Non-Epithelial Types: Germ Cell and Stromal Tumors
Non-epithelial ovarian cancers include germ cell tumors and sex cord-stromal tumors. Germ cell tumors come from egg-producing cells and are more common in young women. They can be benign or malignant, with types like dysgerminoma, yolk sac tumor, and teratoma.
Sex cord-stromal tumors come from the ovary’s stromal cells. These tumors can make hormones and have different symptoms. Granulosa cell tumors are a notable type, linked to estrogen production and endometrial hyperplasia.
Knowing about these ovarian cancer types is key for the right treatment. We’ll look into their characteristics and how they affect patients next.
High-Grade Serous Ovarian Cancer: The Deadliest Subtype
HGSOC is the most common and deadly subtype of ovarian cancer. It poses significant challenges in diagnosis and treatment. We will explore its characteristics, prevalence, and why it has a poor prognosis.
Characteristics and Prevalence of HGSOC
HGSOC is known for its aggressive behavior and late presentation. It causes about 70-80% of ovarian cancer deaths. Its aggressive nature comes from its fast growth and early spread.
Research shows HGSOC often starts in the fallopian tube. This highlights the need to understand where this disease comes from. A study in found that almost all HGSOC cases have a mutation in the TP53 gene.
|
Characteristics |
Description |
Implications |
|---|---|---|
|
Origin |
Often from fallopian tube epithelium |
Understanding origin can inform prevention and early detection strategies |
|
Molecular Features |
Mutations in TP53, BRCA1/2 |
Impacts prognosis and treatment options, including possible targeted therapies |
|
Growth Rate |
Rapid |
Contributes to late diagnosis and poor prognosis |
Why HGSOC Has Poor Prognosis
The poor prognosis of HGSOC comes from several factors. These include late diagnosis, fast progression, and resistance to treatments. We will look at these factors and research aimed at better outcomes for HGSOC patients.
One big challenge is the non-specific symptoms leading to late diagnosis. By the time HGSOC is found, it’s often too late. Also, the cancer’s resistance to chemotherapy makes treatment hard.
Researchers are working on new treatments, like targeted and immunotherapies. Understanding HGSOC’s molecular mechanisms is key to these new treatments.
How Ovarian Cancer Grows and Spreads
It’s important to know how ovarian cancer grows and spreads. This knowledge helps doctors find better ways to treat it. Ovarian cancer grows by a complex process. It invades nearby tissues and can spread to other parts of the body.
Tumor Doubling Time and Growth Patterns
Ovarian cancer grows fast, doubling in size every 2.2 months. This shows how aggressive the disease is. It usually takes about 13.1 months for the cancer to spread from one place to others.
Tumor doubling time is key to understanding how ovarian cancer grows. The rate of growth can differ from person to person. This depends on the type of tumor and how well the body’s immune system fights it.
Metastasis Timeline and Common Spread Patterns
Ovarian cancer often spreads within the peritoneal cavity. It usually goes to the omentum, bowel, and other pelvic areas. The metastasis timeline can vary, but it usually happens within a year after the tumor starts growing.
Here are some common ways ovarian cancer spreads:
- Direct extension to nearby organs
- Intraperitoneal dissemination
- Lymphatic spread to regional lymph nodes
- Hematogenous spread to distant organs, though this is less common
|
Pattern of Spread |
Description |
Frequency |
|---|---|---|
|
Direct Extension |
Spread to adjacent organs |
Common |
|
Intraperitoneal Dissemination |
Spread within the peritoneal cavity |
Very Common |
|
Lymphatic Spread |
Spread to regional lymph nodes |
Common |
|
Hematogenous Spread |
Spread to distant organs via bloodstream |
Less Common |
Knowing these patterns helps doctors create better treatment plans. This can improve how well patients do.
Ovarian Cancer Statistics and Epidemiology
Ovarian cancer’s spread and death rates give us key insights. Knowing these stats helps us see how it affects health and guides research.
Current Incidence and Mortality in the United States
The (SEER) show ovarian cancer is a big worry in the US. In 2023, about 19,680 women got ovarian cancer, and 12,740 died from it.
This shows how serious ovarian cancer is for women’s health. Its high death rate comes from being hard to catch early.
Projected Cases and Deaths for 2025
For 2025, ovarian cancer will keep affecting US healthcare. About 20,890 women will get it, and 12,730 will die. This calls for more research and better ways to find and treat it.
These numbers stress the need for ongoing research. By studying ovarian cancer, we can tackle its health challenges better.
Molecular and Genetic Mechanisms of Ovarian Cancer
Understanding ovarian cancer’s molecular and genetic roots is key to finding better treatments. Studies reveal that genetic changes and pathway disruptions are central to this disease’s start and growth.
Key Genetic Mutations
Genetic changes like BRCA1 and BRCA2 are major risk factors for ovarian cancer. These genes help fix DNA, and mutations in them cause DNA instability, a cancer trait.a top researcher, says, “BRCA1 and BRCA2 mutations greatly raise ovarian cancer risk, making genetic tests very important.”
“The presence of BRCA1 and BRCA2 mutations significantly increases the risk of developing ovarian cancer, highlighting the importance of genetic screening.”
TP53, a tumor suppressor gene, is often mutated in the most aggressive ovarian cancer type, HGSOC. These mutations disrupt cell cycle control, helping tumors grow and spread.
Molecular Pathways in Cancer Development
Ovarian cancer’s development involves complex molecular pathways. The PI3K/AKT signaling pathway is often disrupted in ovarian cancer. It’s vital for cell survival and growth, and its overactivation can help cancer spread.
- The PI3K/AKT pathway helps cells live longer by stopping cell death.
- When this pathway goes wrong, cells grow and tumors expand.
- Targeting the PI3K/AKT pathway is a promising treatment for ovarian cancer.
Other molecular mechanisms, like the MAPK/ERK signaling pathway and DNA repair changes, also play roles in ovarian cancer. Knowing these pathways is vital for creating targeted treatments.
We’re getting closer to understanding ovarian cancer’s genetic and molecular bases. This knowledge will help us develop better diagnostic and treatment options. More research is needed to lower ovarian cancer rates and deaths.
Risk Factors for Developing Ovarian Cancer
Ovarian cancer is influenced by genetics, environment, and lifestyle. Knowing these factors helps us spot who’s at higher risk. This knowledge is key for early detection.
Hereditary and Genetic Predispositions
Hereditary and genetic factors are big risks for ovarian cancer. Women with a family history of ovarian or breast cancer face higher risks. Mutations in BRCA1 and BRCA2 genes greatly increase ovarian cancer risk.
Women with a BRCA1 mutation face a 35-70% chance of ovarian cancer by age 80. Those with a BRCA2 mutation have a 10-30% chance.
“Genetic testing can spot BRCA1 and BRCA2 mutations,” saysa gynecologic oncology expert. “This allows for early intervention and risk management.”
Age and Reproductive History Factors
Age is a big risk factor, with ovarian cancer risk rising after 50. Reproductive history also matters. Women who’ve never been pregnant or had trouble getting pregnant are at higher risk. But, pregnancy and breastfeeding can lower this risk.
- Women who have never been pregnant are at a higher risk.
- Pregnancy and breastfeeding reduce the risk.
- Early menopause or late onset of menopause may also influence risk.
Environmental and Lifestyle Influences
Lifestyle and environment also affect ovarian cancer risk. Using talcum powder in the genital area may increase risk, though evidence is not solid. Obesity and a diet high in fat may also raise risk.
The American Cancer Society notes, “Genetic, environmental, and lifestyle factors all play a part in ovarian cancer risk.”
Understanding these factors helps us identify high-risk individuals. This promotes early detection and prevention strategies.
Protective Factors That May Reduce Ovarian Cancer Risk
Several protective factors have been found to lower the risk of ovarian cancer. Knowing about these can help us find ways to prevent it. This knowledge can help inform our lifestyle and medical decisions.
Oral Contraceptives and Hormone Therapy
Using oral contraceptives has been linked to a lower risk of ovarian cancer. The longer you use them, the more the risk drops. Oral contraceptives can cut the risk by up to 50% after five years.
Hormone therapy, like estrogen-progestin therapy, might also protect against ovarian cancer. While the evidence isn’t as strong, some studies hint at a possible risk reduction with certain hormone therapies.
|
Protective Factor |
Risk Reduction |
Duration of Use |
|---|---|---|
|
Oral Contraceptives |
Up to 50% |
5 years or more |
|
Hormone Therapy (Estrogen-Progestin) |
Variable |
Varies |
Pregnancy, Breastfeeding, and Surgical Procedures
Pregnancy is a protective factor against ovarian cancer. The risk goes down with each full-term pregnancy. Breastfeeding might also lower the risk, but the evidence is not as clear.
Certain surgeries, like tubal ligation and salpingectomy, can also reduce the risk. These surgeries are thought to stop cancer cells from spreading from the fallopian tubes to the ovaries.
- Pregnancy reduces ovarian cancer risk, with greater reduction with more full-term pregnancies.
- Breastfeeding may offer some protection, though evidence varies.
- Surgical procedures like tubal ligation and salpingectomy have been associated with reduced risk.
Understanding these protective factors helps us find ways to lower ovarian cancer risk. More research is needed to fully understand these effects and find more ways to prevent it.
Why Early Detection of Ovarian Cancer Remains Challenging
Finding ovarian cancer early is hard because it often doesn’t show symptoms at first. This makes it tough for both patients and doctors to catch it early.
The “Silent Killer” Phenomenon
Ovarian cancer is called a “silent killer” because it doesn’t show symptoms until it’s too late. This makes it hard to catch early, as it can grow a lot before being found. Many cases are only found when the cancer has spread, making treatment harder.
Studies have shown that early symptoms are often not specific. Symptoms like bloating and pain can mean many things, not just ovarian cancer. This makes it hard to know if it’s ovarian cancer early on.
Limitations of Current Screening Methods
Today’s screening tools for ovarian cancer have big limits. The main tools are transvaginal ultrasound (TVUS) and the CA-125 blood test. TVUS can spot ovarian masses, but it can’t say for sure if it’s cancer. The CA-125 test looks for a protein that’s often high in ovarian cancer, but it can also be high in other things, leading to false positives.
We know these tools help, but they’re not good enough for regular checks in women who don’t have symptoms. Research is ongoing to find better ways to screen, like new biomarkers and better imaging.
Creating better screening tools is key to finding ovarian cancer early. Until then, focusing on those at high risk and teaching them about symptoms is important. This is a big part of fighting this disease.
Diagnosis and Staging Process
Getting a correct diagnosis and staging is key for treating ovarian cancer well. We use a mix of clinical checks, imaging, and lab tests to see how far the disease has spread.
Diagnostic Procedures and Tests
Several tests help find ovarian cancer. Imaging tests like ultrasound, CT scans, and MRI help see the ovaries and find any problems. “Imaging has changed how we find ovarian cancer,” say experts.
“Imaging is very important in finding and knowing how far ovarian cancer has spread, helping spot the main tumor and any spread,”
— Expert Opinion
We also use serum tumor markers, like CA-125, to help diagnose and track the disease. A detailed physical examination and looking at the patient’s health history are also key.
The steps to diagnose include:
- Pelvic exam
- Imaging tests (ultrasound, CT, MRI)
- CA-125 blood test
- Looking at biopsy samples under a microscope
FIGO Staging System
The FIGO staging system is used a lot for ovarian cancer. It shows how far the disease has spread and helps decide treatment.
|
FIGO Stage |
Description |
|---|---|
|
I |
Limited to one or both ovaries |
|
II |
Involves one or both ovaries with pelvic extension |
|
III |
Tumor involves one or both ovaries with spread to the peritoneum outside the pelvis |
|
IV |
Distant metastasis excluding peritoneal metastasis |
Knowing about diagnosis and staging is very important for ovarian cancer patients. It affects how they are treated and their chances of getting better. Emphasizing a thorough diagnostic process is crucial for accurate staging and optimal patient care.
Modern Treatment Approaches for Ovarian Cancer
Ovarian cancer treatment has grown a lot, thanks to new research and tech. Now, we have many ways to treat it, each one fitting the needs of each patient.
Surgical Interventions and Cytoreduction
Surgery is key in fighting ovarian cancer. The goal is to remove as much tumor as possible. Cytoreductive surgery helps patients live longer and makes other treatments work better.
- Primary debulking surgery removes the tumor and affected tissues.
- Interval debulking surgery is done after chemotherapy to shrink the tumor more.
- Less invasive surgeries are used to help patients recover faster and do better.
Chemotherapy Protocols and Response Rates
Chemotherapy is a big part of treating ovarian cancer, often paired with surgery. Platinum-based chemotherapy is often the first choice. Paclitaxel and carboplatin are common drugs used.
- Neoadjuvant chemotherapy is given before surgery to make tumors smaller.
- Adjuvant chemotherapy is used after surgery to kill any cancer cells left.
- How well a patient responds can depend on the cancer’s stage and type, and the patient’s health.
Targeted Therapies and Immunotherapy Advances
Targeted therapies and immunotherapy are bringing new hope to ovarian cancer treatment. PARP inhibitors are showing great promise in treating BRCA1/2-mutated ovarian cancers.
- Bevacizumab is a targeted therapy that stops tumors from growing by blocking blood vessels.
- Immunotherapies, like checkpoint inhibitors, are being tested in clinical trials.
- Personalized medicine is being developed to match treatments to each patient’s genetic makeup.
Ovarian cancer treatment is changing fast, thanks to ongoing research and trials. As we learn more about the disease, our treatments are getting better, giving patients new hope.
Living with Ovarian Cancer: Patient Perspectives
<SEP-15553_image_4>
Living with ovarian cancer takes a lot of strength, support, and a full care plan. We must look at the patient’s view and the many things that shape their journey.
Quality of Life Considerations
Ovarian cancer and its treatment can really change a patient’s quality of life. Symptoms like pain, tiredness, and stomach problems can make everyday tasks hard. We need to tackle these issues with a care plan that includes managing symptoms and supportive therapies.
Patients often feel emotional and psychological pain, like anxiety and depression. Emotional support from doctors, family, and support groups is key. It helps patients deal with their diagnosis and treatment.
- Access to counseling and mental health services
- Support groups for patients and their families
- Palliative care to manage symptoms and improve quality of life
Support Resources and Survivorship
Support resources are key for patients with ovarian cancer. Patient advocacy groups and organizations offer important info, emotional support, and connections with others facing similar challenges.
Survivorship programs are also vital. They help patients deal with life after treatment. These programs cover concerns like recurrence, long-term side effects, and staying healthy.
“Survivorship care is not just about managing the physical aspects of cancer; it’s also about supporting the emotional and social needs of patients as they move forward.”
We understand the need for a complete care approach. We want to make sure patients have the resources they need to do well.
Conclusion: Future Directions in Ovarian Cancer Research and Care
As we learn more about ovarian cancer, new paths in research and care are emerging. At livhospital.com, we aim to offer top-notch healthcare. We also support international patients fully.
Research into ovarian cancer is leading to better treatments and outcomes. We’re looking at new screening methods, targeted therapies, and personalized medicine. These are key areas for future growth.
By focusing on ovarian cancer research and care, we can make a big difference. Our goal is to give patients and their families the best care. We stay up-to-date with the latest in cancer treatment and research.
FAQ
What is ovarian cancer and where does it usually start?
Ovarian cancer starts in the fallopian tubes or the surface of the ovaries. Knowing where it starts is key for early detection and treatment.
Is ovarian cancer genetic?
Yes, some ovarian cancers are linked to genetic mutations like BRCA1 and BRCA2. But not all cases are genetic.
What are the risk factors for developing ovarian cancer?
Risk factors include genetic predispositions, age, and reproductive history. Lifestyle and environmental factors also play a role.
Can birth control cause ovarian cancer?
No, birth control pills actually lower the risk of ovarian cancer. They are considered protective.
What are the symptoms of ovarian cancer?
Ovarian cancer is often silent in its early stages. Symptoms include bloating, pelvic pain, and trouble eating.
How is ovarian cancer diagnosed?
Diagnosis involves tests like imaging, blood tests, and biopsy. The FIGO staging system helps determine the disease’s extent.
What are the treatment options for ovarian cancer?
Treatment includes surgery, chemotherapy, targeted therapies, and immunotherapy. A team approach is best for treatment.
Can ovarian cancer be prevented?
While prevention is not guaranteed, some factors like birth control and pregnancy may lower risk. Certain surgeries also help.
What is the prognosis for high-grade serous ovarian cancer (HGSOC)?
HGSOC is a deadly form of ovarian cancer. It grows fast and is hard to treat, leading to a poor prognosis.
How does ovarian cancer grow and spread?
Ovarian cancer grows and spreads quickly. It can spread through the abdomen and lymph nodes.
What support resources are available for patients living with ovarian cancer?
Patients can find support through survivorship programs, counseling, and online communities. These help with physical, emotional, and social needs.
How can I reduce my risk of ovarian cancer?
Understanding risk factors and protective factors is important. Talk to your doctor about your risk and consider preventive steps.
Reference
National Cancer Institute (NCI). Ovarian Epithelial Treatment PDQ. https://www.cancer.gov/types/ovarian/hp/ovarian-epithelial-treatment-pdq






