
Scleroderma, also known as systemic sclerosis, is a chronic autoimmune disease. It affects the skin and internal organs. It is often linked to other autoimmune diseases like primary biliary cirrhosis and Sjögren’s syndrome.
It’s important to understand these connections for better patient care. Patients with scleroderma might also get secondary Sjögren’s syndrome. Or they might have antibodies linked to mixed connective tissue disease. This makes diagnosing and treating them harder.
Key Takeaways
- Scleroderma is linked to several autoimmune diseases, including primary biliary cirrhosis and Sjögren’s syndrome.
- Patients may experience secondary Sjögren’s syndrome or have antibodies associated with mixed connective tissue disease.
- Comprehensive care requires understanding these complex associations.
- Diagnosis and treatment can be challenging due to the complexity of the disease.
- Systemic sclerosis is another term for scleroderma, highlighting its impact on the skin and internal organs.
Understanding Scleroderma: An Overview
Scleroderma is a complex autoimmune disorder that affects both the skin and internal organs. It’s hard to diagnose and treat because it shows up in many ways. This condition makes the skin and organs hard by adding too much collagen. It can really change someone’s life, so knowing about it and how to manage it is key.
Definition and Classification of Scleroderma
Scleroderma is split into two main types based on how much of the body is affected. Localized scleroderma only affects the skin and sometimes the tissues under it. On the other hand, systemic scleroderma or systemic sclerosis hits the skin and many organs inside the body.
The term scleroderma covers a range of symptoms, from mild skin issues to widespread disease. Knowing what sclerosis definition means in medicine is important. It’s about tissues getting hard because of too much collagen. Systemic sclerosis shows that the disease affects the whole body.
Localized vs. Systemic Scleroderma
Telling localized from systemic scleroderma is important for treatment and outlook. Localized scleroderma mainly affects the skin and sometimes the tissues under it. But it doesn’t touch the organs inside. Systemic scleroderma, though, is more serious and can harm important organs.
|
Characteristics |
Localized Scleroderma |
Systemic Scleroderma/Systemic Sclerosis |
|---|---|---|
|
Skin Involvement |
Limited to specific areas |
Widespread, including face and hands |
|
Organ Involvement |
None |
Potential involvement of lungs, heart, kidneys, and gastrointestinal tract |
|
Autoantibodies |
Less commonly associated with specific autoantibodies |
Often associated with specific autoantibodies like anti-Scl-70 and anti-centromere |
|
Prognosis |
Generally better, with less risk of internal organ damage |
Varies based on the extent of organ involvement |
It’s critical for doctors to know the difference between localized and systemic scleroderma. This helps them give the right care. It also helps patients understand their condition and what it means for their life.
The Autoimmune Nature of Scleroderma
Scleroderma is an autoimmune disease. It happens when the immune system attacks the body’s own tissues. This leads to inflammation and fibrosis, causing the disease’s symptoms.
How Scleroderma Functions as an Autoimmune Disease
Scleroderma works like an autoimmune disease. It triggers an immune response that attacks the body’s cells and tissues. T cells and B cells are key players in this process.
These immune cells activate and produce autoantibodies and cytokines. These substances cause inflammation and fibrosis.
Key immune components involved in scleroderma include:
- T cells: Play a central role in cell-mediated immunity and are implicated in the disease’s pathogenesis.
- B cells: Produce autoantibodies that contribute to the disease’s progression.
- Cytokines: Signaling molecules that promote inflammation and fibrosis.
The Role of the Immune System in Scleroderma
The immune system is vital in scleroderma. It’s the immune system’s abnormal response that drives the disease. This response causes inflammation and fibrosis in tissues.
|
Immune Component |
Role in Scleroderma |
|---|---|
|
T cells |
Contribute to cell-mediated immunity and disease pathogenesis |
|
B cells |
Produce autoantibodies that exacerbate the disease |
|
Cytokines |
Promote inflammation and fibrosis |
Understanding the immune system’s role in scleroderma is key. It helps us find effective treatments. By focusing on specific immune responses, we can lessen the disease’s effects on patients.
Primary Biliary Cirrhosis and Scleroderma
Primary biliary cirrhosis is a chronic liver disease often linked to scleroderma, mainly in those with limited systemic sclerosis. This connection shows how autoimmune diseases can interact and require a detailed management plan.
The Liver-Skin Connection
The bond between primary biliary cirrhosis and scleroderma shows that scleroderma is more than skin-deep. It affects internal organs, like the liver. Research points to autoimmune processes in scleroderma contributing to primary biliary cirrhosis.
Studies indicate that primary biliary cirrhosis in scleroderma patients is not just a coincidence. It suggests a common underlying issue. This means scleroderma patients need their liver function closely monitored.
Prevalence and Risk Factors
Primary biliary cirrhosis is more common in scleroderma patients than in the general public. Risk factors include limited systemic sclerosis and certain autoantibodies.
- Limited systemic sclerosis is a big risk factor for primary biliary cirrhosis in scleroderma patients.
- Certain autoantibodies can signal a higher risk of primary biliary cirrhosis.
- Having a family history of autoimmune diseases may also increase the risk in scleroderma patients.
Knowing these risk factors is key to catching primary biliary cirrhosis early in scleroderma patients. We suggest regular check-ups and a team-based care approach.
Sjögren’s Syndrome as a Common Scleroderma Comorbidity
Exploring scleroderma’s complexities, we see how Sjögren’s syndrome affects patients. This autoimmune disorder causes dry eyes and mouth. When it happens with scleroderma, it’s called secondary Sjögren’s syndrome.
Secondary Sjögren’s Syndrome in Scleroderma Patients
Up to 20% of scleroderma patients get secondary Sjögren’s syndrome. This makes their lives harder. Both conditions need a detailed treatment plan.
Secondary Sjögren’s in scleroderma patients shows in different ways. This includes:
- Persistent dryness of the eyes and mouth
- Fatigue and musculoskeletal pain
- Dental caries and oral infections
- Eye discomfort and vision problems
Clinical Manifestations and Symptoms
The symptoms of secondary Sjögren’s in scleroderma patients vary. Some common ones are:
|
Symptom |
Frequency |
Impact on Quality of Life |
|---|---|---|
|
Dry eyes |
Common |
Significant discomfort, vision problems |
|
Dry mouth |
Very Common |
Difficulty swallowing, dental issues |
|
Fatigue |
Common |
Reduced productivity, decreased quality of life |
Knowing these symptoms helps manage the condition better. We stress the need for a team effort in treating scleroderma patients with secondary Sjögren’s. The goal is to ease symptoms and enhance their life quality.
Mixed Connective Tissue Disease and Scleroderma
Mixed connective tissue disease (MCTD) is a complex autoimmune disorder. It often overlaps with scleroderma, making diagnosis and treatment tricky. MCTD shares symptoms with scleroderma, lupus, and myositis, making it a key area of study in autoimmune diseases.
The Overlap Between MCTD and Scleroderma
MCTD and scleroderma share common symptoms like skin thickening, joint pain, and muscle weakness. Patients with MCTD often have a mix of symptoms that make diagnosis hard. Each patient’s case can be different, requiring a detailed diagnostic approach.
The diagnosis of MCTD is confirmed by anti-U1-RNP antibodies. These antibodies are found in most MCTD patients. They are key for telling MCTD apart from other autoimmune diseases.
Anti-U1-RNP Antibodies
Anti-U1-RNP antibodies are vital in diagnosing MCTD. Their presence is linked to a specific set of symptoms that overlap with scleroderma, lupus, and myositis. Finding these antibodies is critical for diagnosing and treating MCTD correctly.
Some MCTD patients also show signs of CREST syndrome. CREST is a variant of limited systemic scleroderma. It includes symptoms like calcinosis, Raynaud’s phenomenon, and telangiectasia. This shows how different autoimmune conditions can interact in MCTD patients.
Inflammatory Myopathies Associated with Scleroderma

Inflammatory myopathies are muscle diseases that can happen with scleroderma. These diseases cause muscle inflammation and weakness. This makes life harder for those affected.
Scleroderma is a complex autoimmune disease. It can also be with other diseases like inflammatory myopathies. We need a detailed plan to manage these diseases together.
Polymyositis in Scleroderma Patients
Polymyositis is an inflammatory myopathy that can happen with scleroderma. It causes muscle inflammation and weakness, mainly in the muscles closest to the body. To diagnose it, we do muscle tests, electromyography, and muscle biopsies.
Polymyositis symptoms in scleroderma patients include muscle weakness, fatigue, and pain. We look at these symptoms to make a correct diagnosis and treatment plan.
Dermatomyositis and Scleroderma Overlap
Dermatomyositis is another inflammatory myopathy that can happen with scleroderma. It has skin symptoms like a rash, along with muscle inflammation and weakness. This mix makes diagnosis and treatment tricky.
Managing dermatomyositis in scleroderma patients needs a team effort. We use immunosuppressive treatments and supportive care. Early treatment is key to avoid lasting damage and improve outcomes.
Systemic Lupus Erythematosus and Scleroderma Overlap
Systemic lupus erythematosus and scleroderma can overlap, creating a unique set of challenges. This overlap combines features of both diseases, making diagnosis and treatment complex.
Distinguishing Features of Lupus-Scleroderma Overlap
The symptoms of lupus-scleroderma overlap vary among patients. Common signs include skin thickening seen in scleroderma and malar rash and joint pain typical of lupus.
To diagnose this overlap, a detailed medical history, physical exam, and specific lab tests are needed. These tests help identify key autoantibodies.
Antibody Profiles in Overlapping Conditions
Identifying specific autoantibodies is key in diagnosing and treating lupus-scleroderma overlap. Anti-U1-RNP antibodies are common in patients with these overlapping diseases.
Knowing the antibody profiles helps doctors create personalized treatment plans. For example, certain autoantibodies may signal a higher risk of organ damage. This guides the use of targeted therapies.
Managing lupus-scleroderma overlap requires a team effort. Rheumatologists, immunologists, and other specialists work together to provide the best care.
Autoantibodies as Diagnostic Markers in Scleroderma
Diagnosing scleroderma often involves finding specific autoantibodies. These autoantibodies are key for diagnosing the disease. They also help predict how the disease might progress and what symptoms might appear.
Anti-Centromere Antibodies and Limited Cutaneous Scleroderma
Anti-centromere antibodies (ACAs) are common in limited cutaneous scleroderma (lcSSc). This type of scleroderma affects the skin on the hands, face, and sometimes forearms. ACAs are often linked to a better prognosis than other scleroderma types.
A study in a rheumatology journal found that ACAs are a sign of limited systemic scleroderma. It shows a lower risk of severe organ problems.
“The detection of ACAs can guide clinicians in predicting disease outcomes and tailoring management strategies.”
Anti-Scl-70 and Diffuse Cutaneous Scleroderma
Anti-Scl-70 antibodies, also known as anti-topoisomerase I antibodies, are linked to diffuse cutaneous scleroderma (dcSSc). This severe form affects the skin widely and often harms internal organs. The presence of these antibodies increases the risk of lung problems and other serious issues.
|
Antibody |
Associated Disease Subtype |
Clinical Implications |
|---|---|---|
|
Anti-Centromere |
Limited Cutaneous Scleroderma |
Favorable prognosis, lower risk of severe organ involvement |
|
Anti-Scl-70 |
Diffuse Cutaneous Scleroderma |
Higher risk of pulmonary fibrosis and severe organ involvement |
|
Anti-RNA Polymerase III |
Diffuse Cutaneous Scleroderma |
Associated with scleroderma renal crisis, rapid disease progression |
Anti-RNA Polymerase III Antibodies
Anti-RNA polymerase III antibodies are significant in scleroderma, mainly in diffuse cutaneous scleroderma. They signal a higher risk of kidney crisis, a serious condition. These antibodies are also linked to quick disease onset and progression.
Knowing the autoantibody profiles helps in managing scleroderma better. Healthcare providers can then tailor treatments more effectively.
Rheumatoid Arthritis and Scleroderma Coexistence

Rheumatoid arthritis and scleroderma can happen together, making diagnosis and treatment tricky. We will look into how this affects diagnosis and treatment.
Joint Manifestations in Scleroderma vs. Rheumatoid Arthritis
Rheumatoid arthritis and scleroderma affect joints differently. Rheumatoid arthritis causes both sides of the body to be inflamed. Scleroderma leads to stiffness and fibrosis in joints.
Key differences in joint manifestations include:
- Symmetry: Rheumatoid arthritis affects joints symmetrically, while scleroderma causes localized issues.
- Inflammation: Rheumatoid arthritis has significant inflammation, but scleroderma causes stiffness and fibrosis.
- Progression: Rheumatoid arthritis can destroy joints faster than scleroderma.
Diagnostic Challenges and Treatment Approaches
Diagnosing rheumatoid arthritis and scleroderma together is hard because symptoms overlap. We need to carefully look at symptoms and use tests to accurately diagnose and treat.
Diagnostic challenges include:
- Distinguishing between rheumatoid arthritis and scleroderma joint symptoms.
- Finding other autoimmune conditions that might be causing symptoms.
- Tracking disease activity and progression in patients with multiple conditions.
Experts say managing patients with these conditions needs a detailed and team-based approach. This approach treats symptoms and the immune system issues that cause these conditions.
This approach involves not only treating the symptoms but also addressing the underlying immune dysregulation that contributes to the coexistence of these conditions.
We will keep looking into the best treatments for patients with rheumatoid arthritis and scleroderma. We will focus on tailoring treatments to meet each patient’s unique needs.
Raynaud’s Phenomenon in Scleroderma and Other Autoimmune Diseases
Raynaud’s phenomenon is common in people with scleroderma. It shows how autoimmune diseases affect blood vessels. This condition causes blood flow to the hands and feet to drop when it’s cold or when someone is stressed.
Primary vs. Secondary Raynaud’s Phenomenon
There are two types of Raynaud’s phenomenon. Primary Raynaud’s phenomenon happens without any other disease. Secondary Raynaud’s phenomenon is linked to diseases like scleroderma. Knowing the difference is key to treating it right.
- Primary Raynaud’s is usually milder and doesn’t have other symptoms.
- Secondary Raynaud’s, found in scleroderma patients, is more serious and has other symptoms too.
Management Strategies for Raynaud’s in Scleroderma
Dealing with Raynaud’s in scleroderma needs a few steps. Here’s what we suggest:
- Stay away from cold and wear warm clothes to stop blood vessels from narrowing.
- Try to relax with meditation or deep breathing to handle stress.
- Don’t smoke or drink caffeine, as they can make blood vessels constrict.
- Use medicines like calcium channel blockers to help blood flow better.
By following these tips, people with scleroderma and Raynaud’s can manage their symptoms better. This can greatly improve their life quality.
CREST Syndrome: A Variant of Scleroderma
CREST syndrome is a specific type of limited cutaneous systemic sclerosis. It has its own set of symptoms. The acronym CREST stands for calcinosis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia.
Components of CREST Syndrome
The parts of CREST syndrome help doctors diagnose and understand the condition. Let’s look at each part:
- Calcinosis: Calcium deposits in the skin and under the skin, causing pain.
- Raynaud’s Phenomenon: A condition that affects blood flow to the fingers and toes, and sometimes the ears, nose, and lips, in response to cold or stress.
- Esophageal Dysmotility: This refers to the abnormal movement of food through the esophagus, which can lead to difficulty swallowing.
- Sclerodactyly: The thickening and tightening of the skin on the fingers, leading to a claw-like appearance.
- Telangiectasia: The visible dilation of small blood vessels near the surface of the skin, often appearing as red spots.
|
Component |
Description |
|---|---|
|
Calcinosis |
Calcium deposits in the skin |
|
Raynaud’s Phenomenon |
Blood flow reduction in response to cold or stress |
|
Esophageal Dysmotility |
Abnormal esophageal movement |
|
Sclerodactyly |
Skin thickening on fingers |
|
Telangiectasia |
Visible dilation of small blood vessels |
Relationship to Limited Cutaneous Systemic Sclerosis
CREST syndrome is closely related to limited cutaneous systemic sclerosis (lcSSc). Both have similar symptoms. CREST is often seen as a subtype of lcSSc. They both often have anti-centromere antibodies, linking them together.
It’s important to understand the connection between CREST syndrome and limited cutaneous systemic sclerosis. This knowledge helps in giving the right care and management to patients.
Epidemiology of Scleroderma and Associated Autoimmune Conditions
The study of scleroderma shows interesting differences in gender and race. This autoimmune disease affects people in different ways. It helps us understand the disease better and what might cause it.
Gender Disparities in Scleroderma
Women are more likely to get scleroderma than men. This is true for many autoimmune diseases. The ratio of women to men with scleroderma can be as high as 14:1.
It’s not clear why this happens. Hormones, genes, and maybe the environment might play a role. Knowing this could help find new treatments.
Racial and Ethnic Variations in Prevalence
Scleroderma affects different races and ethnicities in different ways. For example, limited cutaneous systemic sclerosis is more common in Europeans. Diffuse cutaneous systemic sclerosis is seen more in African Americans.
- Native Americans and African Americans get scleroderma more often than others.
- The disease is more common in certain places.
- This shows that genes and the environment are important in scleroderma.
By looking at these patterns, researchers can learn more about scleroderma. They can then create treatments that work better for different groups.
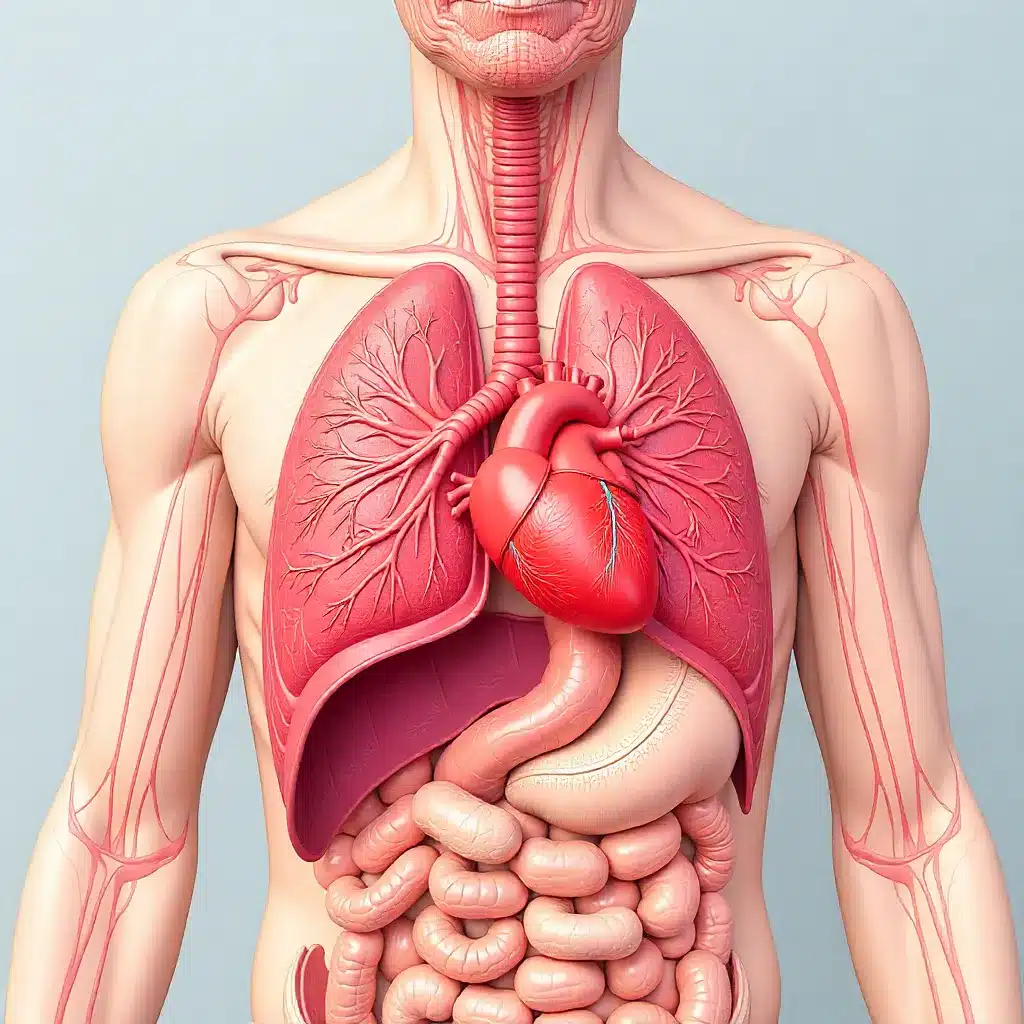
Impact of Scleroderma on Internal Organs
Scleroderma affects more than just the skin. It impacts internal organs in complex ways. This chronic autoimmune disease causes fibrosis and vascular changes in the skin and organs. We’ll look at how it affects the lungs, heart, and stomach.
Pulmonary Involvement and Interstitial Lung Disease
Scleroderma can harm the lungs, causing interstitial lung disease (ILD). ILD leads to inflammation and fibrosis, making it hard to breathe. It’s important to watch for signs of lung problems in scleroderma patients.
Pulmonary Function Tests (PFTs) and High-Resolution Computed Tomography (HRCT) help diagnose and manage ILD. Early treatment can slow the disease’s progress.
|
Pulmonary Complication |
Characteristics |
Diagnostic Tools |
|---|---|---|
|
Interstitial Lung Disease (ILD) |
Inflammation and fibrosis of lung tissue |
PFTs, HRCT |
|
Pulmonary Hypertension |
High blood pressure in the pulmonary arteries |
Echocardiography, Right Heart Catheterization |
Cardiac Manifestations in Scleroderma
The heart can also be affected by scleroderma. This can lead to fibrosis, pericarditis, and arrhythmias. Heart problems can greatly affect a patient’s prognosis.
Regular heart checks, like echocardiography and electrocardiography, are recommended. Managing heart issues often requires a team effort from cardiologists and rheumatologists.
Gastrointestinal Complications
Gastrointestinal problems are common in scleroderma. They can affect the esophagus, stomach, small intestine, and colon. Symptoms range from difficulty swallowing to intestinal pseudo-obstruction.
It’s important for scleroderma patients to have regular GI checks. Treatment may include lifestyle changes, medications, and sometimes surgery.
|
GI Complication |
Symptoms |
Management Strategies |
|---|---|---|
|
Dysphagia |
Difficulty swallowing |
Dietary modifications, swallowing therapy |
|
GERD |
Acid reflux, heartburn |
Proton pump inhibitors, lifestyle changes |
|
Intestinal Pseudo-obstruction |
Abdominal pain, nausea, vomiting |
Bowel rest, nutritional support, medications |
In conclusion, scleroderma’s impact on internal organs is a key part of the disease. Understanding these complications helps us provide better care for patients.
Treatment Approaches for Scleroderma with Overlapping Autoimmune Conditions
Treating scleroderma with other autoimmune conditions needs a mix of treatments. We understand that scleroderma needs a special plan. This plan must consider the other autoimmune diseases it comes with.
Immunosuppressive Therapies
Immunosuppressive therapies are key in treating scleroderma and other autoimmune diseases. These treatments aim to calm down the immune system. This helps ease symptoms and slow down the disease.
Common immunosuppressive agents include:
- Corticosteroids: They help reduce inflammation and slow down the immune system.
- Cyclophosphamide: Used for severe cases, like interstitial lung disease.
- Methotrexate: It’s used for its ability to calm the immune system and reduce inflammation.
Targeted Biological Treatments
Targeted biological treatments offer a more precise way to manage scleroderma and other autoimmune conditions. These treatments focus on specific parts of the immune system. This makes treatment more personalized.
Examples of targeted biological treatments include:
- Rituximab: It targets CD20-positive B cells, reducing inflammation and disease activity.
- Tocilizumab: An interleukin-6 receptor antagonist, used to reduce inflammation.
Organ-Specific Management Strategies
Scleroderma can affect many organs, so specific treatments are needed. We use different treatments for each organ involved.
|
Organ/System |
Common Manifestations |
Management Strategies |
|---|---|---|
|
Skin |
Skin thickening, ulcers |
Topical corticosteroids, wound care |
|
Lungs |
Interstitial lung disease |
Immunosuppressive therapy, pulmonary rehabilitation |
|
Gastrointestinal |
Dysphagia, GERD |
Proton pump inhibitors, dietary modifications |
By using immunosuppressive therapies, targeted biological treatments, and organ-specific strategies, we can offer full care. This is for patients with scleroderma and other autoimmune conditions.
Conclusion: Navigating the Complex Landscape of Scleroderma and Associated Autoimmune Diseases
We’ve looked into how scleroderma and other autoimmune diseases are connected. This shows the challenges in diagnosing and treating them. Scleroderma, a complex autoimmune condition, often happens with other autoimmune diseases. This makes it hard for doctors to treat.
Understanding the relationship between scleroderma and other autoimmune diseases is key. By knowing the unique traits of each condition, we can create better treatment plans. This way, we can meet the specific needs of each patient.
As we learn more about scleroderma and its links to other autoimmune diseases, we can help patients more. A detailed and team-based approach helps manage scleroderma’s complexities. This way, we can give the best care to those dealing with this condition.
FAQ
What is scleroderma, and how is it related to other autoimmune diseases?
Scleroderma is a chronic autoimmune disease that affects the skin and internal organs. It is often linked to other autoimmune diseases like primary biliary cirrhosis and Sjögren’s syndrome.
What are the different types of scleroderma, and how are they classified?
Scleroderma is divided into types based on severity and organ involvement. It includes localized and systemic scleroderma. Systemic scleroderma is split into limited and diffuse types.
What is the role of the immune system in scleroderma?
The immune system is complex in scleroderma. It involves many cell types and pathways leading to inflammation and fibrosis.
What is the connection between scleroderma and primary biliary cirrhosis?
Primary biliary cirrhosis is a chronic liver disease that often coexists with scleroderma. Research is ongoing to understand the link between the liver and skin in scleroderma patients.
What is CREST syndrome, and how is it related to scleroderma?
CREST syndrome is a subtype of limited cutaneous systemic sclerosis. It is characterized by calcinosis, Raynaud’s phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia.
What is Raynaud’s phenomenon, and how is it managed in scleroderma patients?
Raynaud’s phenomenon is a vascular condition causing digital vasospasm, often triggered by cold or stress. In scleroderma, it is a significant symptom needing specific management, including lifestyle changes and medications.
How does scleroderma impact internal organs, and what are the possible complications?
Scleroderma can severely affect internal organs like the lungs, heart, and gastrointestinal tract. This can lead to complications such as interstitial lung disease, cardiac manifestations, and gastrointestinal dysmotility.
What are the treatment options for scleroderma and overlapping autoimmune conditions?
Treating scleroderma and overlapping autoimmune conditions involves various therapies. These include immunosuppressive treatments, targeted biological treatments, and organ-specific management strategies.
What is the epidemiology of scleroderma, and are there any gender or racial disparities?
Scleroderma’s epidemiology shows significant gender disparities, with females more frequently affected. There are also racial and ethnic variations in prevalence, highlighting the need for tailored diagnosis and treatment approaches.
What is the significance of autoantibodies in scleroderma diagnosis and classification?
Autoantibodies are critical in diagnosing and classifying scleroderma. Different autoantibodies are linked to various clinical manifestations and outcomes.
References
- Adigun, R., Goyal, A., & Hariz, A. (2024, April 5). Systemic sclerosis (scleroderma). In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430875/ NCBI
- Romanowska-Próchnicka, K., Dziewit, M., Lesiak, A., Reich, A., & Olesińska, M. (2024). Scleroderma and scleroderma-like syndromes. Frontiers in Immunology, 15, 1351675. https://doi.org/10.3389/fimmu.2024.1351675 Frontiers+2Frontiers+2
- Therapeutic promise of hyaluronidase in systemic sclerosis. (2024). PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11314198/ PubMed Central
- “Systemic scleroderma: who gets scleroderma?” (n.d.). National Organization for Rare Disorders. Retrieved from https://scleroderma.org/who-gets-scleroderma/ National Organization for Rare Disorders
- Inflammation: Types, symptoms, causes, and treatment. (n.d.). Medical News Today. Retrieved from https://www.medicalnewstoday.com/articles/175235 PubMed+1





