Last Updated on October 21, 2025 by mcelik
Myelodysplastic syndrome (MDS) is a rare blood disorder. It disrupts normal blood cell production. MDS can affect various organs and systems in the body, leading to a range of complications.
The impact of MDS on the body can be significant. It causes fatigue, infections, and anemia due to disrupted blood cell production.
Myelodysplastic syndrome (MDS) is a complex group of blood disorders. It happens when the bone marrow can’t make healthy blood cells. This leads to health problems.
MDS is like cancer because it involves abnormal cell growth in the bone marrow. It’s classified based on the blood cells affected and genetic changes. The World Health Organization (WHO) has different subtypes of MDS.
“Diagnosing and classifying MDS need a detailed look, including bone marrow biopsy and genetic tests,” say hematologists.
The exact cause of MDS is not always clear. But some things can increase your risk. These include exposure to harmful chemicals, radiation, and past treatments. Age also plays a big role, with MDS more common in older people.
Knowing these risk factors helps in early detection and treatment of MDS. As a leading medical source notes, “Understanding MDS and its risk factors is key to effective treatment.”
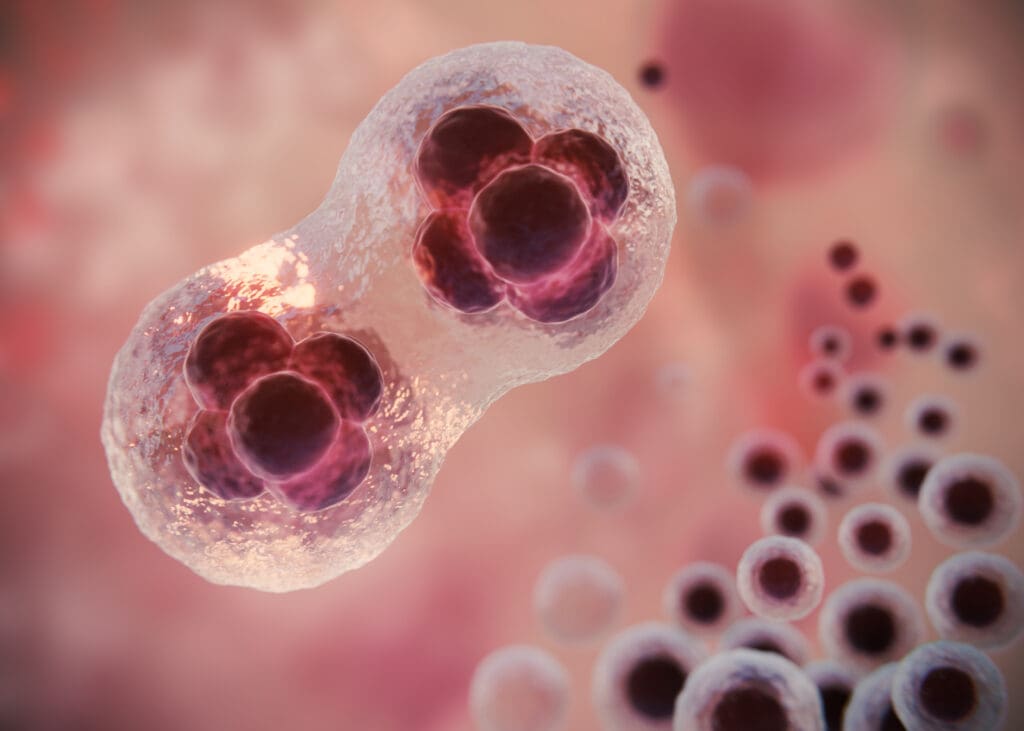
MDS, or myelodysplastic syndrome, is a blood cancer that starts in the bone marrow. It affects how healthy blood cells are made. The bone marrow makes blood cells like red, white, and platelets through a complex process.
The bone marrow is like a factory for blood cells. It turns stem cells into different blood cells. Red blood cells carry oxygen, white blood cells fight infections, and platelets help with blood clotting.
The bone marrow makes blood cells at a rate that meets the body’s needs. It replaces old or damaged cells.
In MDS, the bone marrow can’t make healthy blood cells well. This leads to a lack of healthy cells. It can cause anemia, infections, and bleeding disorders.
Research shows MDS changes the bone marrow’s environment. This affects blood cell production and function. A study on AI prognostic tools in AML found insights into MDS progression and its impact on the bone marrow.
MDS causes changes in stem and progenitor cells in the bone marrow. These changes lead to defective blood cells that can’t work right.
A key sign of MDS is dysplastic changes in bone marrow cells. These changes can be seen under a microscope. They include abnormal cell shape and disrupted maturation.
| Cell Type | Normal Function | MDS-Related Complications |
| Red Blood Cells | Carry oxygen | Anemia |
| White Blood Cells | Fight infections | Increased infection risk |
| Platelets | Blood clotting | Bleeding disorders |
MDS disrupts bone marrow function, causing health issues. Experts say, “Understanding MDS biology is key to finding effective treatments.”
MDS greatly impacts blood cell production, causing many problems. Myelodysplastic Syndrome messes with the bone marrow. This is where blood cells are made.
Anemia is a big problem in MDS. It happens when the bone marrow makes fewer or faulty red blood cells. Symptoms include feeling tired, weak, and short of breath.
Red blood cells carry oxygen around the body. In MDS, the bone marrow can’t make enough healthy ones. This leads to myelodysplastic anemia.
| Symptoms | Causes | Effects |
| Fatigue, weakness | Reduced red blood cell production | Anemia |
| Shortness of breath | Defective red blood cells | Reduced oxygen delivery |
MDS also messes with white blood cells. These cells are key for our immune system. Fewer healthy white blood cells mean a higher risk of getting sick.
White blood cells fight off infections. In MDS, they’re often not made right. This makes people more likely to get sick.
Platelets are another blood cell type affected by MDS. Low platelet counts, or thrombocytopenia, cause bleeding and bruising.
MDS affects many blood cells, including red, white, and platelets. Knowing how it impacts these cells is key to managing the disease.
The hematological system is where MDS mainly affects the body. It disrupts the production of healthy blood cells. This leads to various complications.
MDS changes blood composition by affecting red, white blood cells, and platelets. Anemia is common, causing fatigue and weakness. It also leads to leukopenia, making infections more likely.
Abnormal cell production causes an imbalance in blood. This is a key sign of MDS. It can lead to mds leukemia or myelodysplastic preleukemia, known as pre leukemia.
Circulation problems occur in MDS due to poor red blood cell production. This reduces oxygen to tissues and organs. Symptoms include dizziness and shortness of breath.
Cardiovascular risks also increase. Managing these issues is important.
MDS affects platelet production, causing thrombocytopenia. This raises the risk of bleeding and clotting problems. Patients may bruise easily, have nosebleeds, or bleed a lot after injuries.
Diagnosing MDS involves blood tests and bone marrow exams. Understanding MDS prognosis is key to managing it. Regular checks and treatment can reduce risks.

Myelodysplastic syndrome (MDS) greatly affects the immune system, causing many problems. The immune system fights off infections and diseases. But in MDS patients, it doesn’t work well.
In MDS, the bone marrow can’t make healthy blood cells. This includes immune cells like neutrophils and lymphocytes. These cells are key in fighting off infections. So, MDS patients often have weak immune systems.
Key mechanisms include:
People with MDS face a higher risk of getting infections. These infections can be very serious and even life-threatening.
| Infection Type | Common Causes | Consequences |
| Bacterial Infections | Gram-negative bacteria, such as Escherichia coli | Sepsis, organ failure |
| Viral Infections | Reactivation of latent viruses like CMV | Pneumonitis, hepatitis |
| Fungal Infections | Candida species, Aspergillus species | Invasive fungal disease, high mortality |
MDS can also cause the immune system to attack the body’s own tissues. This can lead to many symptoms and problems.
Examples of autoimmune manifestations in MDS include:
Patients with myelodysplastic syndrome (MDS) face serious heart problems. MDS mainly affects blood production but also impacts the heart.
Anemia, common in MDS, puts extra stress on the heart. The heart works harder to make up for fewer red blood cells. This can lead to heart failure over time.
Those with heart issues are at higher risk. The heart’s extra work can worsen existing heart disease. It’s vital to manage anemia carefully.
MDS can harm blood vessels, leading to vascular problems. These changes can affect blood vessel function and structure. This can contribute to heart disease.
The vascular effects of MDS might be hard to spot. Regular checks are key for early detection and treatment.
Treatment for MDS patients with heart issues must be carefully planned. It’s important to balance MDS treatment with heart health. This includes watching for heart side effects of MDS treatments.
| Cardiac Condition | MDS Treatment Consideration | Cardiovascular Risk |
| Heart Failure | Careful use of blood transfusions | Fluid overload |
| Coronary Artery Disease | Monitoring for anemia management | Increased cardiac workload |
| Arrhythmias | Avoiding certain medications | Electrolyte imbalance |
MDS patients with heart conditions need a team of doctors. This team should handle both MDS and heart health.
Myelodysplastic syndrome (MDS) can greatly affect the respiratory system. This can lead to various complications. These issues can impact a patient’s quality of life and overall health.
MDS patients face a higher risk of pulmonary infections. Their immune system is weakened, making them more prone to infections. These infections can be severe and even life-threatening. Prompt treatment and preventive measures are key in managing these risks.
MDS patients may struggle with breathing due to anemia or other disease-related complications. Anemia can reduce oxygen delivery to tissues, causing shortness of breath and fatigue. It’s important to manage anemia and other causes to ease these symptoms.
Treatment for MDS can also cause pulmonary issues. Some medications and therapies have side effects on the lungs. In some cases, treatment plans may need adjustments to reduce these effects. Monitoring and follow-up care are essential to address any emerging issues quickly.
In conclusion, MDS patients face significant respiratory challenges. These include pulmonary infections, breathing difficulties, and treatment-related complications. Effective management and monitoring are critical to address these risks.
Myelodysplastic Syndrome (MDS) affects more than just blood cells. It can also harm the digestive system and liver. Knowing about these effects is key to helping MDS patients fully.
MDS can cause problems like trouble swallowing, bleeding in the gut, and changes in how food moves through the body. These issues might come from the disease itself or from treatments.
Gastrointestinal bleeding is a big worry. It can cause anemia and make things worse for the patient. Doctors from different fields often work together to handle these problems.
The liver can also be affected by MDS. This might show up as changes in liver enzymes or too much iron in the liver from blood transfusions. Keeping an eye on the liver is important to avoid lasting damage.
The risk of hepatic iron overload is high. It can cause cirrhosis and other liver problems if not managed right. Regular checks and chelation therapy can help lower this risk.
MDS patients often face nutritional issues like weight loss, malnutrition, and missing out on important nutrients. It’s important to make sure they get enough food to stay healthy and support their treatment.
Dealing with these nutritional challenges needs a plan made just for each patient. It should consider their specific needs and the complications of their MDS.
The impact of MDS on the nervous system is a key area for healthcare providers. Myelodysplastic Syndrome mainly affects the bone marrow and blood cells. But, it can also have big effects on the nervous system.
Cognitive impacts are a big worry for MDS patients. They might find it hard to focus, remember things, and make decisions. “Cognitive dysfunction in MDS patients can be attributed to various factors, including anemia, infections, and treatment side effects.” Studies show that fixing these problems can help lessen cognitive symptoms.
MDS can harm the peripheral nervous system. This can cause numbness, tingling, and weakness in the limbs. Peripheral neuropathy can really lower a patient’s quality of life. To manage this, a team effort is needed, including pain management and physical therapy.
“Neurological complications in MDS patients can arise from the disease itself or as a result of treatment. It’s vital for healthcare providers to watch patients closely for any signs of neurological issues.”
Treatment for MDS can sometimes cause neurological problems. Some medicines and therapies might lead to neuropathy, seizures, or changes in thinking. Careful monitoring and adjusting treatment plans are key to reduce these risks.
In summary, MDS’s neurological effects are complex and need careful thought in managing the disease. By understanding these effects, healthcare providers can give better care to MDS patients.
MDS affects blood cell production and also impacts the renal system. The renal system is key for health. Its problems can cause many issues in MDS patients.
The kidneys filter waste, control blood pressure, and balance electrolytes. In MDS, kidney function impairment can happen. This is due to anemia, infections, and some medicines. It can cause toxin buildup, making things worse.
Urinary problems are common in MDS patients. Issues like hematuria (blood in urine) and dysuria (painful urination) can occur. These are often due to infections or MDS-related factors. It’s important to manage these to avoid more health problems.
When treating MDS, the kidneys’ health is a big concern. Some treatments can harm the kidneys. It’s vital to watch kidney health closely. Changing treatment plans to protect the kidneys is a key part of managing MDS.
In conclusion, MDS patients need care that covers all aspects of their health. This includes the renal system’s changes. It’s important to treat not just the main symptoms but also the broader effects of MDS on the body.
MDS affects more than just the bone marrow. It can also impact the skin and mucous membranes. This can greatly affect a patient’s quality of life.
MDS can cause changes in the mouth and mucous membranes. Patients may experience mucositis, oral ulcers, or other mucosal issues.
“Oral and Page changes are significant concerns Page patients, often resulting from the disease itself or its treatment.”
– Expert Opinion-
Effective management of these complications can greatly improve patient outcomes.
Myelodysplastic syndrome (MDS) greatly affects the endocrine system. This leads to hormonal and metabolic issues. The endocrine system is key for hormone production, which controls many body functions.
MDS can mess with the endocrine glands, causing hormonal imbalances. These imbalances can impact growth, metabolism, and reproductive functions. For example, thyroid problems are common, leading to hypothyroidism or hyperthyroidism.
The hormonal changes in MDS can have big effects. These include:
MDS can also cause big metabolic changes. These changes affect how the body uses nutrients. This can lead to weight changes and blood sugar level issues.
| Metabolic Change | Potential Impact |
| Altered glucose metabolism | Increased risk of diabetes |
| Changes in lipid profiles | Increased risk of cardiovascular disease |
| Nutritional deficiencies | Impaired overall health and well-being |
The endocrine system effects in MDS patients can really hurt their quality of life. Hormonal imbalances and metabolic changes cause symptoms like fatigue, mood swings, and less physical ability.
It’s important to manage these endocrine-related issues to improve MDS patients’ lives. This means watching for hormonal imbalances, managing metabolic changes, and treating symptoms.
Myelodysplastic syndrome (MDS) is a complex condition. It can turn into acute myeloid leukemia (AML), a more aggressive blood cancer. This change affects the patient’s outlook and treatment plan.
Several factors can increase the risk of MDS turning into AML. These include:
When MDS turns into AML, it can affect more organs. This makes managing the disease harder. Organs often affected include:
Regular checks are key to catching MDS turning into AML early. This includes:
Spotting progression early can lead to better treatment and outcomes for patients.
Myelodysplastic syndrome (MDS) is a complex disorder that affects many organs and systems. This leads to various complications. It’s important to have a complete care plan for MDS patients to manage these issues.
Managing MDS effectively means addressing many areas. This includes the blood, immune, heart, lungs, stomach, brain, kidneys, and hormones. Knowing how MDS impacts these areas helps doctors create better treatment plans.
Comprehensive care for MDS goes beyond just treating organ issues. It also means watching for the disease to get worse or turn into acute myeloid leukemia. A team approach can greatly improve patient outcomes and quality of life.
To manage MDS well, doctors need to understand the disease and its effects. With a complete care plan, doctors can lower the risk of serious problems and death from MDS.
Myelodysplastic Syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells. This often leads to bone marrow failure.
Symptoms of MDS include fatigue and weakness. You might also have pale skin and shortness of breath. There’s also a higher risk of infections and bleeding.
Doctors use blood tests and a bone marrow biopsy to diagnose MDS. They check the bone marrow and blood cells to assess the condition.
Risk factors for MDS include exposure to chemicals and radiation. Previous chemotherapy or radiation therapy also increases the risk. Genetic predisposition plays a role too.
Yes, MDS can progress to AML. AML is a more aggressive form of blood cancer in some patients.
Treatment for MDS varies based on the subtype and severity. It can include supportive care and medications to stimulate blood cell production. In some cases, bone marrow transplantation is considered.
Complications of MDS include anemia and infections. There’s also a risk of bleeding disorders and progression to AML. Iron overload from frequent blood transfusions can damage organs.
MDS can weaken the immune system. It does this by reducing the production of healthy white blood cells. This increases the risk of infections.
While less common, some patients with MDS may experience neurological symptoms. These can be directly or indirectly related to the disease or its treatment.
MDS can significantly impact quality of life. Symptoms like fatigue and the need for frequent medical interventions are common. The psychological burden of living with a chronic illness also affects patients.
There are no specific dietary recommendations to cure MDS. But, a balanced diet can help manage symptoms and support overall health.
The frequency of follow-up appointments for MDS patients varies. It depends on the severity of the disease, the treatment plan, and the patient’s overall health condition.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!