Last Updated on November 6, 2025 by
Myelodysplastic syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells. These problems usually start in the bone marrow.
A significant number of MDS patients are diagnosed incidentally during examinations for unrelated conditions. This shows how hard it can be to spot this disease.
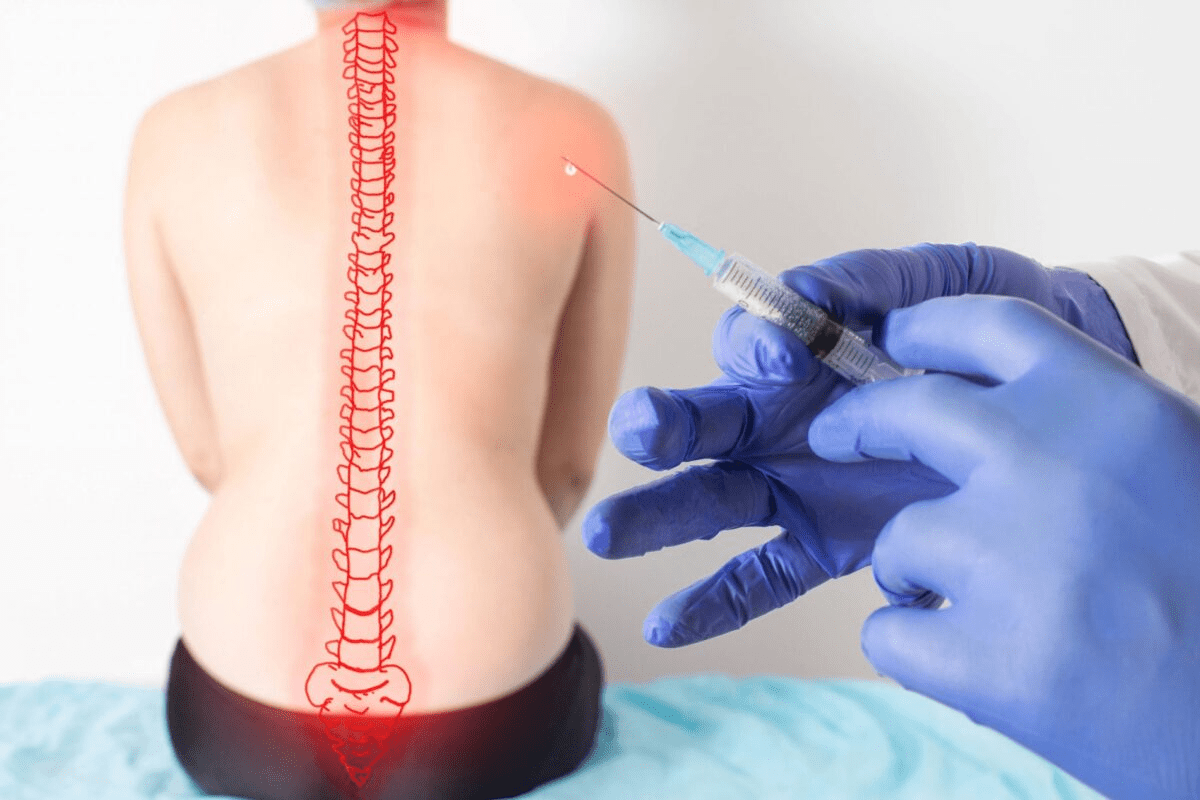
To diagnose MDS, doctors use a few methods. These include bone marrow biopsy, blood tests, and sometimes MRI. MRI is not the primary diagnostic tool for MDS, but it can provide valuable insights into bone marrow changes and related complications.
This is true when there’s a chance the bone marrow is involved or when there are specific complications.
Key Takeaways
- MDS is characterized by the production of abnormal blood cells in the bone marrow.
- Diagnosis involves a combination of bone marrow biopsy, blood tests, and sometimes imaging.
- MRI can be used to assess certain aspects of MDS, particular complications.
- Understanding MDS requires a complete approach to diagnosis and treatment.
- MDS diagnosis is often found by chance during tests for other conditions.
What is Myelodysplastic Syndrome?
Myelodysplastic syndrome, or MDS, is a group of disorders. It happens when blood cells don’t form right. This makes it hard for the bone marrow to make healthy blood cells.
Definition and Basic Characteristics
MDS means the bone marrow can’t make blood cells fast enough. The bone marrow makes stem cells that turn into different blood cells. But in MDS, these stem cells don’t grow right, leading to low blood cell counts.
Key characteristics of MDS include:
- Dysplasia in one or more blood cell lines
- Ineffective hematopoiesis leading to cytopenias
- Risk of progression to acute myeloid leukemia (AML)
Prevalence and Risk Factors
MDS is rare, with about 4-5 cases per 100,000 people in the U.S. each year. It mostly affects people over 70.
Risk factors for MDS include:
- Exposure to certain chemicals and toxins
- Previous chemotherapy or radiation therapy
- Genetic predisposition
Impact on Blood Cell Production
MDS messes with blood cell production. This can cause anemia, neutropenia, and thrombocytopenia. Anemia makes you tired and weak. Neutropenia raises your risk of getting sick. Thrombocytopenia can cause bleeding problems.
Knowing how MDS affects blood cell production is key. It helps manage the condition and improve life quality for those affected.
MDS Medical Abbreviation and Related Terminology
Myelodysplastic Syndrome, or MDS, is a group of bone marrow disorders. It affects how blood cells are made. Knowing the MDS medical abbreviation is key for doctors and patients to understand blood disorders better.
Decoding MDS in Medical Context
MDS is a set of disorders where blood cells don’t form right. The bone marrow can’t make healthy blood cells. This leads to health problems. The MDS abbreviation is used a lot in medical texts and patient records. It helps doctors talk clearly about patient conditions.
“Myelodysplastic syndromes are a heterogeneous group of clonal hematopoietic disorders characterized by ineffective hematopoiesis and a variable risk of progression to acute myeloid leukemia.”
Other Important Abbreviations in Hematology
Hematology, the study of blood disorders, uses many abbreviations. These make complex terms easier to understand. Some important ones are:
- AML – Acute Myeloid Leukemia
- CMML – Chronic Myelomonocytic Leukemia
- MDS/MPN – Myelodysplastic Syndromes/Myeloproliferative Neoplasms overlap syndromes
Knowing these abbreviations is important for correct diagnosis and treatment plans.
| Abbreviation | Full Form | Description |
| MDS | Myelodysplastic Syndrome | A group of disorders caused by poorly formed blood cells |
| AML | Acute Myeloid Leukemia | A type of cancer of the myeloid line of blood cells |
| ICD-10 | International Classification of Diseases, 10th Revision | A coding system used for classifying diagnoses and procedures |
ICD-10 Classification for Myelodysplastic Syndrome
The ICD-10 system is used globally for health condition coding, including MDS. Specific MDS codes under ICD-10 help in recording and analyzing the disorder. For example, D46 is a code for myelodysplastic syndromes.
Correct ICD-10 coding is key for studies, healthcare management, and insurance. It helps document and analyze MDS cases. This leads to better understanding and management of the condition.
Types and Classification of Myelodysplastic Syndromes
Myelodysplastic syndromes (MDS) are a group of disorders with different characteristics. Understanding these differences is key to managing them. The classification helps us grasp their pathophysiology and treatment options.
WHO Classification System
The World Health Organization (WHO) classification system is widely used for MDS. It considers morphological features, genetic abnormalities, and clinical characteristics. This system helps predict prognosis and guide treatment.
The WHO classification includes several MDS subtypes. These include MDS with single lineage dysplasia, MDS with multilineage dysplasia, and MDS with ring sideroblasts. Each subtype has its own diagnostic criteria and prognosis.
MDS with Ringed Sideroblasts
MDS with ringed sideroblasts (MDS-RS) is marked by ring sideroblasts in the bone marrow. These cells have abnormal iron accumulation in mitochondria. MDS-RS can occur with or without multilineage dysplasia.
The presence of ring sideroblasts is linked to mutations in genes like SF3B1. Patients with MDS-RS may have a better prognosis than others with MDS.
MDS with Multilineage Dysplasia
MDS with multilineage dysplasia (MDS-MLD) shows dysplastic changes in multiple lineages. This includes erythroid, granulocytic, and megakaryocytic lineages. It often presents with cytopenias and has a variable prognosis.
MDS-MLD can be further divided based on ring sideroblast presence. Diagnosing MDS-MLD requires a detailed examination of bone marrow and peripheral blood smears.
Stages and Progression of MDS
Knowing the stage of MDS is key for planning treatment. MDS is a group of disorders with different progressions. Each patient’s journey is unique.
IPSS and IPSS-R Scoring Systems
The International Prognostic Scoring System (IPSS) and its updated version, IPSS-R, help sort MDS patients. They look at factors like genetic changes, blast counts, and blood counts.
The IPSS-R offers a more detailed look at prognosis. It groups patients into very low, low, intermediate, high, and very high-risk categories. This helps doctors choose the right treatment.
| IPSS-R Score | Risk Category | Median Survival (years) |
| ≤ 1.5 | Very Low/Low | 8.8 |
| 1.5-3 | Intermediate | 5.3 |
| 3-4.5 | High | 1.8 |
| > 4.5 | Very High | 0.8 |
Low-Risk vs. High-Risk MDS
MDS patients are split into low-risk and high-risk groups. Low-risk patients tend to have a slower disease. High-risk patients are more likely to turn into AML.
Low-risk MDS is often treated with supportive care like blood transfusions. High-risk MDS might need stronger treatments, like hypomethylating agents or stem cell transplants.
Monitoring Disease Progression
Regular checks are important to track MDS. This includes blood tests, bone marrow biopsies, and genetic tests.
Spotting disease progression early can lead to better outcomes. Doctors should watch for signs like more blasts or worse blood counts.
MDS and Anemia: A Common Manifestation
The link between myelodysplastic syndrome (MDS) and anemia is complex. Anemia happens when there aren’t enough red blood cells. This makes it hard for tissues and organs to get enough oxygen.
Mechanisms of MDS-Related Anemia
Anemia in MDS patients comes from several causes. One reason is ineffective erythropoiesis. This means the bone marrow can’t make enough red blood cells, even when it’s trying hard.

Other reasons include:
- Increased apoptosis of erythroid precursors
- Impaired iron utilization
- Defects in the bone marrow microenvironment
These causes work together. They can be affected by the genetic changes in MDS.
Clinical Presentation of MDS Anemia
People with MDS anemia might feel tired, weak, or short of breath. They might also have pale skin. A study found that about 80-90% of MDS patients have anemia when they’re first diagnosed.
“Anemia is a major contributor to the morbidity associated with MDS, impacting patients’ quality of life and potentially influencing disease outcomes.”
Management Approaches for MDS Anemia
There are several ways to manage MDS anemia. These include:
| Management Strategy | Description |
| Red Blood Cell Transfusions | Regular transfusions to improve hemoglobin levels and alleviate symptoms |
| Erythropoiesis-Stimulating Agents (ESAs) | Medications that stimulate the production of red blood cells |
| Iron Chelation Therapy | Treatment to reduce iron overload resulting from frequent transfusions |
Doctors pick the best treatment based on the patient’s situation. This includes how bad the anemia is and if there are other MDS problems.
Diagnostic Approaches for Myelodysplastic Syndrome
The process to diagnose MDS involves several key steps. It starts with an initial check-up that guides further tests.
Initial Assessment and Blood Tests
Diagnosing MDS begins with a detailed medical history and physical check-up. This helps spot symptoms and signs of bone marrow issues. Blood tests are also vital, showing any oddities in blood cell counts and shapes.
Blood tests include a complete blood count (CBC) and differential count. These tests can show anemia, low platelets, or low white blood cells. Such findings often lead to more tests.
Bone Marrow Biopsy and Aspiration
A bone marrow biopsy and aspiration are key for diagnosing MDS. These tests remove a bone marrow sample for study.
The biopsy shows the marrow’s cell count and structure. The aspiration lets doctors look at individual marrow cells. Together, they spot the dysplastic changes seen in MDS.
Key findings in bone marrow biopsy for MDS include:
- Dysplasia in one or more cell lines
- Increased blasts
- Ringed sideroblasts
Peripheral Blood Smear Analysis
A peripheral blood smear analysis adds to the CBC by showing blood cell shapes in detail. This test can spot oddities like dysplastic neutrophils or blasts, helping confirm MDS.
| Diagnostic Test | Key Findings in MDS |
| Blood Tests (CBC) | Anemia, thrombocytopenia, leukopenia |
| Bone Marrow Biopsy | Dysplasia, increased blasts, ringed sideroblasts |
| Peripheral Blood Smear | Dysplastic neutrophils, blasts |
“The diagnosis of MDS requires a combination of clinical evaluation, blood tests, and bone marrow examination. Integrating these findings is key for accurate diagnosis and classification.” – Hematology Expert
By using these diagnostic methods, doctors can accurately diagnose MDS. This helps in creating the right treatment plan.
Imaging Techniques in Blood Disorders
In the world of blood disorders, medical imaging is key for diagnosis and tracking. It’s used for Myelodysplastic Syndrome (MDS) and more.
Overview of Medical Imaging for Hematological Conditions
Medical imaging is now vital for diagnosing and managing blood diseases. MRI, CT scans, and PET scans give insights into bone marrow and blood cells. They help doctors diagnose and keep track of MDS.
Medical imaging in hematology has many uses:
- It helps see how diseases progress.
- It spots complications from blood diseases.
- It helps decide on treatments by showing detailed images.
Limitations of Conventional Imaging
Even though imaging has improved hematology, it’s not perfect. For example:
- Some methods don’t show enough detail, like soft tissue issues.
- Imaging with radiation, like CT scans, has risks.
- Advanced imaging can be expensive and hard to get in some places.
Despite these issues, traditional imaging is very important for diagnosing and treating blood diseases.
When Imaging Is Indicated in MDS
Imaging is needed in MDS for a few reasons:
- To check the bone marrow for problems.
- To see how widespread the disease is and any complications.
- To watch how treatment is working and make changes if needed.
In summary, imaging is very important for managing MDS and other blood diseases. Knowing when and how to use these tools is key for the best care.
MRI Technology and Its Applications
MRI has greatly improved our ability to diagnose and monitor medical conditions, including bone marrow issues. It uses a strong magnetic field, radio waves, and computer algorithms to create detailed images of the body’s internal structures.
How MRI Works
MRI technology is based on nuclear magnetic resonance. When a patient is in the MRI machine, the strong magnetic field aligns the hydrogen nuclei in their body. Radio waves then disturb these nuclei, causing them to emit signals.
These signals are captured by the MRI machine and processed into detailed images.
Key components of MRI technology include:
- The main magnetic field, which aligns the hydrogen nuclei.
- Gradient coils, which encode the signals spatially.
- Radiofrequency coils, which transmit and receive the signals.
Strengths and Limitations of MRI
MRI has many benefits, like high-resolution images of soft tissues and no ionizing radiation. But, it also has downsides like high cost and claustrophobia in some patients. It’s not suitable for patients with certain metal implants.
Despite these drawbacks, MRI is a powerful tool, mainly for soft tissue and bone marrow assessments.
MRI in Bone Marrow Assessment
MRI is great for assessing bone marrow because it can show different marrow types and detect issues. It helps diagnose myelodysplastic syndrome by showing the bone marrow’s structure and any problems.
Using MRI for bone marrow assessment can help catch MDS early and track it. This can lead to better patient outcomes. Its ability to show detailed images without radiation makes it key in managing hematological disorders.
Can MDS Be Detected on an MRI?
Researchers are studying MRI’s role in spotting MDS. They look at how MRI shows changes in bone marrow linked to the syndrome. Myelodysplastic Syndromes (MDS) are disorders where blood cells don’t form right, diagnosed by bone marrow biopsy and blood tests.
Direct Visualization Possibilities
Directly seeing MDS on MRI means looking at bone marrow changes. MRI can tell different types of bone marrow apart by their fat and water levels. In MDS, MRI can show bone marrow changes, like different signal intensity due to cell and fat changes.
MRI sequences like T1-weighted and T2-weighted images, and Short-Tau Inversion Recovery (STIR) sequences, are key. T1-weighted images spot marrow replacement by abnormal cells. STIR sequences show marrow edema or infiltration.
Indirect Signs and Associated Findings
Seeing MDS directly on MRI is hard, but indirect signs hint at its presence. These include:
- Changes in bone marrow signal intensity
- Presence of marrow edema
- Signal pattern changes in spleen or liver, linked to hematopoiesis outside the bone marrow
These signs, while not proof, can lead to more tests, like bone marrow biopsy, to confirm MDS.
Research on MRI in MDS Detection
Recent studies look into MRI’s role in diagnosing and tracking MDS. They found MRI can show how severe MDS is and if certain genetic changes are present.
| Study | Findings | Implications |
| Smith et al. (2020) | Correlation between MRI marrow signal changes and MDS severity | Potential for MRI to non-invasively assess MDS severity |
| Johnson et al. (2019) | Use of MRI to detect extramedullary hematopoiesis in MDS patients | Enhanced detection of disease complications |
In summary, MRI isn’t a surefire way to diagnose MDS, but it offers insights into bone marrow and related findings. Ongoing studies aim to better understand MRI’s role in managing MDS.
Alternative Imaging Methods for MDS
While MRI is a powerful tool, other imaging methods are key in diagnosing Myelodysplastic Syndrome. These methods give valuable info that can add to MRI findings. They help us understand the disease better.
CT Scans and Their Role
CT scans are often used to check MDS, focusing on how far the disease has spread. They show detailed images of the abdomen and chest. This helps spot any problems.
PET Scans in Hematological Malignancies
PET scans show how active tissues are, which is great for finding cancer. In MDS, they help spot when the disease might turn into AML.
Ultrasound Applications
Ultrasound is a safe way to check for spleen or lymph node issues. It’s good for watching how MDS progresses in patients.
Experts say,
“Using different imaging methods helps us understand MDS better. It guides how we treat it.”
| Imaging Technique | Primary Use in MDS | Advantages |
| CT Scan | Assessing disease extent, detecting splenomegaly or lymphadenopathy | Detailed cross-sectional images, widely available |
| PET Scan | Detecting transformation to AML, assessing metabolic activity | High sensitivity for detecting metabolically active disease |
| Ultrasound | Assessing splenomegaly, monitoring disease progression | Non-invasive, low cost, no radiation |
The Relationship Between MDS and Leukemia
MDS can turn into leukemia, like AML, which is a big worry in hematology. Myelodysplastic syndromes (MDS) are disorders where blood cells don’t form right. This makes people more likely to get acute myeloid leukemia (AML).
MDS Progression to AML
MDS can turn into AML, where bad white blood cells grow fast in the bone marrow. How likely this happens depends on the type of MDS and other factors. These include genetic changes and certain bone marrow problems.
The International Prognostic Scoring System (IPSS) helps guess if MDS will turn into AML. It looks at things like how many bad cells are in the bone marrow, the bone marrow’s genetic makeup, and how many blood problems there are.
Risk Factors for Transformation
Some things make it more likely for MDS to turn into AML. These include:
- More bad cells in the bone marrow
- Complex genetic problems in the bone marrow
- Genetic changes, like in the TP53 gene
- Being older and not feeling well
Knowing these risk factors helps doctors manage MDS better. It might even stop or slow down AML from happening.
Monitoring and Prevention Strategies
It’s important to keep an eye on MDS patients for signs of AML. This means:
- Regular blood tests to see if blood cell counts change
- Bone marrow biopsies to check for bad cells and genetic problems
- Genetic tests to find mutations that raise AML risk
Preventing AML might involve treatments like hypomethylating agents and lenalidomide. New treatments are also being tested in clinical trials.
In short, knowing how MDS and leukemia are connected is key to good care. By spotting risk factors and using the right treatments, doctors can help MDS patients a lot.
Treatment Approaches for Myelodysplastic Syndrome
It’s important to know the different ways to treat myelodysplastic syndrome. Each treatment plan is made just for the patient. It considers the patient’s MDS, health, and what they prefer.
Supportive Care Strategies
Supportive care is key in managing MDS. It aims to ease symptoms and improve life quality. This includes:
- Blood transfusions to address anemia and reduce fatigue
- Growth factors to stimulate the production of blood cells
- Antimicrobial therapy to prevent and treat infections
Table 1: Supportive Care Measures in MDS
| Measure | Purpose | Benefits |
| Blood Transfusions | Address anemia | Reduce fatigue, improve quality of life |
| Growth Factors | Stimulate blood cell production | Reduce need for transfusions, improve blood counts |
Medication Options and Targeted Therapies
There are many medications and targeted therapies for MDS. These include:
- Immunomodulatory drugs to modify the immune system’s response
- Hypomethylating agents to improve blood counts and potentially alter the disease course
- Lenalidomide for specific subtypes of MDS, with certain genetic abnormalities
Stem Cell Transplantation
Stem cell transplantation is a possible cure for MDS. It replaces the patient’s diseased bone marrow with healthy stem cells from a donor.
Choosing to have a stem cell transplant is a big decision. It depends on the patient’s health, MDS risk, and if a donor is available.
Recent Advances in MDS Diagnosis and Imaging
The field of MDS diagnosis is changing fast. New imaging and diagnostic methods are key. They help improve patient care and tailor treatments.
Emerging Diagnostic Technologies
New diagnostic tools are making MDS diagnosis more accurate. Next-Generation Sequencing (NGS) helps find genetic mutations important for diagnosis. Flow cytometry now lets us study bone marrow cells in detail. This helps tell MDS apart from other blood disorders.
Novel Imaging Approaches
Imaging has also improved a lot. Magnetic Resonance Imaging (MRI) is now key for checking bone marrow. PET-CT scans might show where the disease is active in the bone marrow.
Future Directions in MDS Detection
The future looks bright with artificial intelligence (AI) and machine learning algorithms. They can quickly analyze lots of data, including images and genes. This could lead to faster and more accurate diagnoses. Also, liquid biopsies might soon let us track the disease without invasive tests.
The future of MDS diagnosis and imaging is exciting. New technologies will likely change patient care a lot. They promise more personalized and effective treatments.
Conclusion
Myelodysplastic Syndrome (MDS) is a complex disorder that affects how our body makes blood cells. It’s important to understand what MDS is, how common it is, and how it impacts our health. This article has covered many aspects of MDS, including how it’s diagnosed and the role of MRI in this process.
Diagnosing MDS involves several steps, including blood tests and a bone marrow biopsy. MRI isn’t the main tool for diagnosing MDS. Yet, it can offer insights into bone marrow changes and help track how the disease progresses.
In summary, MDS is a complex condition that needs a detailed diagnostic approach. By knowing the strengths and weaknesses of different imaging methods, doctors can make better decisions for their patients. Research into new diagnostic technologies and imaging methods is ongoing. This research aims to improve our understanding and treatment of MDS.
This summary wraps up the main points discussed, stressing the need for a team effort in diagnosing and treating MDS. As medical knowledge grows, it’s vital for healthcare professionals and patients to stay updated on the latest findings.
FAQ
What is Myelodysplastic Syndrome (MDS)?
Myelodysplastic Syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells. This often leads to bone marrow failure.
What does MDS stand for in medical terminology?
MDS stands for Myelodysplastic Syndrome. It’s a condition where the body makes abnormal blood cells.
How is MDS classified according to the ICD-10?
The ICD-10 classifies MDS under code D46. This code covers different subtypes of myelodysplastic syndromes.
What are the different types of Myelodysplastic Syndromes?
The World Health Organization (WHO) classifies MDS into several subtypes. These include MDS with ringed sideroblasts and MDS with multilineage dysplasia.
Can MDS be detected using MRI?
MRI is not the main tool for diagnosing MDS. But, it can help check bone marrow changes. It can also spot indirect signs of the condition.
What is the relationship between MDS and anemia?
Anemia is common in MDS. It happens because of ineffective erythropoiesis. This is when the body can’t make enough red blood cells.
How is MDS diagnosed?
Diagnosing MDS involves several steps. Blood tests, bone marrow biopsy, and peripheral blood smear analysis are used. These help check blood cell morphology and bone marrow function.
What is the role of imaging techniques in diagnosing MDS?
Imaging techniques like MRI, CT scans, and PET scans help evaluate bone marrow. They can spot changes linked to MDS. But, they’re not the main tools for diagnosis.
Can MDS progress to acute myeloid leukemia (AML)?
Yes, MDS can turn into AML. AML is a more aggressive blood cancer. Some subtypes and risk factors make this more likely.
What are the treatment approaches for MDS?
Treatment for MDS varies. It includes supportive care, medications, targeted therapies, and stem cell transplantation. The choice depends on the subtype, risk category, and the patient’s needs.
What are the recent advances in MDS diagnosis and imaging?
New technologies and imaging methods are being explored. They aim to better detect and manage MDS. This includes advancements in MRI and other imaging tools.