Myelodysplastic syndrome (MDS) is a group of disorders. They are caused by blood cells that are poorly formed or don’t work right. This leads to ineffective hematopoiesis, causing different types of cytopenias.
The most common finding in MDS is cytopenia, often seen as anemia. This happens when the bone marrow can’t make enough healthy blood cells. It causes fatigue, infections, and bleeding problems.
Key Takeaways
- Myelodysplastic syndrome (MDS) is characterized by ineffective hematopoiesis.
- The most common finding in MDS is cytopenia, often presenting as anemia.
- MDS is a group of disorders with poorly formed or dysfunctional blood cells.
- Cytopenia leads to various complications, including fatigue and infections.
- Understanding MDS is key to managing its symptoms.
Understanding Myelodysplastic Syndrome (MDS)
Myelodysplastic syndrome (MDS) is a complex blood disorder. It needs a deep understanding for the right diagnosis and treatment. MDS is a condition where blood cells don’t work right and can turn into acute myeloid leukemia (AML).
Definition and Basic Concepts
MDS is a group of disorders where blood cells don’t form or work well. This leads to low counts of different blood cells. Doctors use blood tests and bone marrow exams to diagnose MDS.
Research is ongoing to understand MDS better. This includes studying its molecular and genetic underpinnings. Knowing this helps in creating better treatments and improving patient care.
Significance in Hematological Disorders
MDS is very important in hematology because it can turn into AML. Catching it early and treating it right is key to preventing this. MDS also affects patients’ quality of life, causing anemia, infections, and bleeding.
It’s vital for hematologists to understand MDS’s causes. This includes genetic mutations and environmental factors. Knowing this helps in giving the best care to patients.
Epidemiology of Myelodysplastic Syndrome
Myelodysplastic syndrome (MDS) is studied to understand its spread and causes. This study helps us see how MDS affects different groups of people. It’s key to knowing how the disease moves through various populations.
Prevalence and Incidence Rates
MDS becomes more common with age, hitting the elderly hard. Research shows a big jump in cases after 60. The latest numbers say 4-5 cases per 100,000 people get MDS each year, with men getting it more often than women.
The number of people living with MDS is also growing. This is because more people are getting older and doctors can diagnose it better now.
Demographic Patterns
Demographics are important in studying MDS. The disease is more common in men and gets worse with age. Other factors like ethnicity and where you live can also affect MDS rates.
- Age: MDS mostly affects people over 60.
- Gender: Men are more likely to get MDS than women.
- Ethnicity and Geography: Different groups and places have different rates of MDS.
Knowing these patterns helps doctors create better treatments. It also improves care for patients with MDS.
Pathophysiology of MDS
To understand MDS, we need to look at its cellular and molecular roots. It’s caused by genetic changes in stem cells, leading to poor blood cell production.
Cellular and Molecular Mechanisms
MDS comes from complex changes in cells and genes. Genetic mutations are key in messing up blood cell creation.
At the cell level, MDS shows an imbalance in cell growth and death. This imbalance causes poor blood cell making, leading to anemia and other blood issues.
Genetic Abnormalities in MDS
Genetic changes are a big part of MDS. Mutations in SRSF2, ASXL1, and RUNX1 affect how cells work and grow.
| Gene | Function | Frequency in MDS |
| SRSF2 | Splicing factor | 10-15% |
| ASXL1 | Transcriptional regulator | 15-20% |
| RUNX1 | Hematopoiesis regulator | 10-15% |
These genetic changes make MDS different for everyone. Knowing the specific mutations helps doctors choose the right treatment.
Classification Systems for Myelodysplastic Syndrome
Many classification systems help diagnose and predict myelodysplastic syndrome (MDS). They make understanding MDS easier and guide treatment plans.
These systems have changed over time. They show how our knowledge of MDS has grown. Now, we can predict outcomes more accurately.
WHO Classification
The World Health Organization (WHO) system is widely used for MDS. It sorts MDS by its look, the number of affected cell lines, and certain genetic changes.
The WHO system separates MDS into different types. These include MDS with single lineage dysplasia, MDS with multilineage dysplasia, and MDS with ring sideroblasts. Knowing the type helps predict how the disease will progress.
International Prognostic Scoring System (IPSS)
The International Prognostic Scoring System (IPSS) is key for MDS assessment. It looks at the number of blood cell shortages, bone marrow blasts, and genetic changes to forecast outcomes.
The IPSS gives a score that shows the risk of turning into acute myeloid leukemia and survival chances. It helps doctors decide on treatments.
Common Clinical Manifestations of MDS
MDS can cause many symptoms, including anemia, neutropenia, and thrombocytopenia. These symptoms greatly affect the quality of life for those with MDS.
Symptoms Related to Cytopenias
Cytopenias are a key feature of MDS, leading to various symptoms. Anemia causes fatigue, weakness, and shortness of breath. Neutropenia raises the risk of infections. Thrombocytopenia can cause bleeding issues.
The severity of these symptoms varies among patients. Some may feel only mildly tired, while others face severe infections or bleeding.
| Cytopenia | Common Symptoms | Potential Complications |
| Anemia | Fatigue, weakness, shortness of breath | Reduced quality of life, increased risk of cardiovascular events |
| Neutropenia | Increased infections | Severe infections, sepsis |
| Thrombocytopenia | Bleeding gums, easy bruising | Significant bleeding, hemorrhage |
Other Clinical Presentations
Some patients with MDS may also have other symptoms. These can include an enlarged spleen, liver, or skin issues.
These symptoms can make diagnosis more complex and may need extra tests.
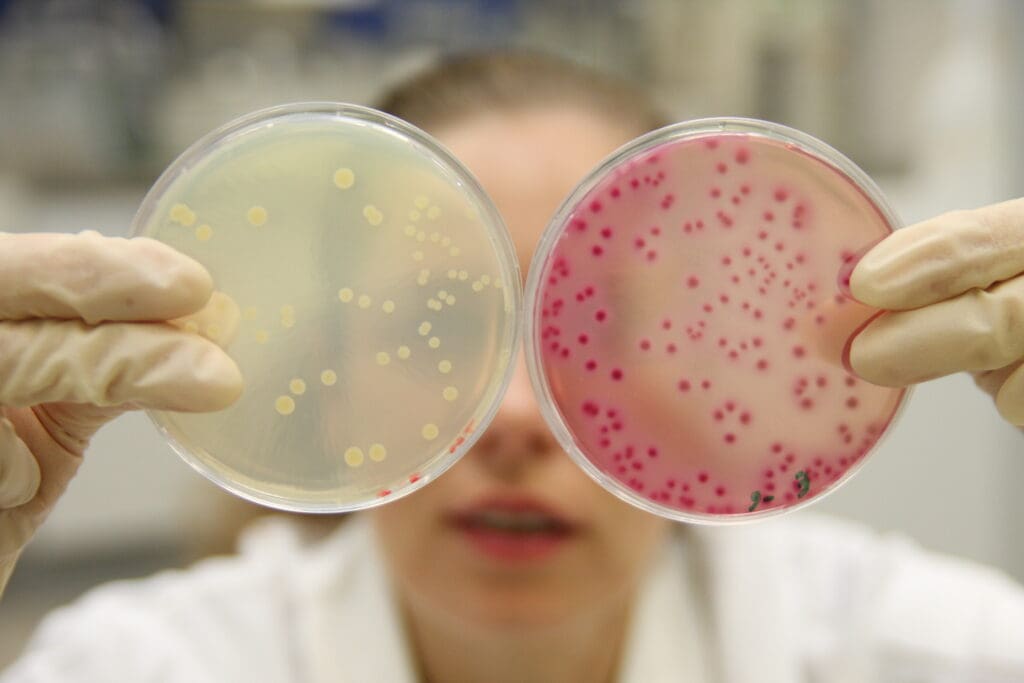
Laboratory Findings in Myelodysplastic Syndrome
Understanding MDS laboratory findings is key for correct diagnosis and treatment. Lab tests are vital to spot MDS and its related blood issues.
Peripheral Blood Abnormalities
Peripheral blood issues are a big sign of MDS. These problems include cytopenias, which mean fewer blood cells. Anemia, a drop in red blood cells, is the most common.
Neutropenia and thrombocytopenia, which affect neutrophils and platelets, can also happen. A blood smear can show dysplastic changes in blood cells. These might include odd shapes or abnormal nuclei.
Bone Marrow Findings

Bone marrow tests are essential for MDS diagnosis. The marrow usually looks hypercellular, meaning it has more cells than usual. Dysplastic changes in marrow cells are typical of MDS.
These changes can be seen in different cell types, like red, white, and platelet-making cells. Some MDS types have ringed sideroblasts. These are red blood cells with iron buildup around the nucleus.
The Most Common Finding in MDS: Cytopenia
Cytopenia is a key feature of MDS, showing up as anemia, neutropenia, or thrombocytopenia. These issues happen when the bone marrow can’t make enough blood cells. This leads to different health problems.
Anemia as the Predominant Finding

Anemia, the most frequent manifestation of MDS, results from insufficient red blood cell production, causing fatigue, weakness, and shortness of breath. Anemia’s severity can vary, and often, blood transfusions are needed to help manage symptoms and improve life quality.
Anemia in MDS comes from the bone marrow’s failure to make enough red blood cells. This failure is due to genetic and molecular problems affecting the cells that make red blood cells.
Neutropenia and Thrombocytopenia
Neutropenia (low neutrophil count) and thrombocytopenia (low platelet count) are also big concerns in MDS. Neutropenia makes it harder to fight off infections because neutrophils are key in defending against pathogens. Thrombocytopenia can cause bleeding problems because platelets are vital for blood clotting.
Managing neutropenia and thrombocytopenia involves supportive care. This includes using growth factors to boost neutrophil production and platelet transfusions to prevent or treat bleeding.
Morphological Abnormalities in MDS
MDS is known for its unique cell shapes, which help doctors diagnose and understand it. These odd shapes are seen in blood tests and bone marrow samples.
Dysplastic Changes in Blood Cells
Dysplastic changes in MDS affect different types of blood cells. This includes red blood cells, white blood cells, and platelet-making cells. These changes can make cells look irregular, with odd shapes and problems in growing right.
Key dysplastic features include:
- Nuclear irregularities and multinucleation in erythroblasts
- Hypogranulation and pseudo-Pelger-Huët anomaly in granulocytes
- Micromegakaryocytes and megakaryocytes with separated nuclei
Ringed Sideroblasts and Other Distinctive Features
Ringed sideroblasts are a key sign in some MDS types, like those with del(5q) or SF3B1 mutations. These cells show up as a ring around the nucleus when stained blue.
Seeing ringed sideroblasts and other unique cell shapes helps doctors diagnose and classify MDS. Below is a table that shows these changes and what they mean for diagnosis:
| Morphological Abnormality | Cell Lineage | Diagnostic Implication |
| Ringed Sideroblasts | Erythroblasts | Associated with MDS-RS, often with SF3B1 mutation |
| Pseudo-Pelger-Huët Anomaly | Granulocytes | Indicative of dysgranulopoiesis |
| Micromegakaryocytes | Megakaryocytes | Suggestive of dysmegakaryopoiesis |
Knowing about these cell shape changes is key for diagnosing and treating MDS. By spotting these signs, doctors can pinpoint the right subtype and plan the best treatment.
Diagnostic Approach to Myelodysplastic Syndrome
Identifying MDS requires a detailed diagnostic process. It involves clinical assessment and specialized tests. The goal is to accurately diagnose and manage the condition through a combination of clinical findings, laboratory results, and bone marrow analysis.
Initial Evaluation and Testing
The first step in diagnosing MDS is a thorough medical history and physical exam. This helps identify symptoms and signs that might suggest MDS, like cytopenias or other blood issues.
Laboratory tests are key in the diagnostic process. They include:
- Complete Blood Count (CBC) to check for cytopenias
- Peripheral blood smear to look at blood cell morphology
- Bone marrow aspiration and biopsy to examine bone marrow cells and detect dysplastic changes
Confirmatory Diagnostic Criteria
The diagnosis of MDS is confirmed by combining clinical findings, lab results, and specific criteria. The World Health Organization (WHO) classification system is used to categorize MDS into subtypes based on morphology and genetics.
The criteria for diagnosing MDS include:
| Diagnostic Criteria | Description |
| Cytopenia | Presence of anemia, neutropenia, or thrombocytopenia |
| Dysplasia | Morphological evidence of dysplasia in one or more myeloid lineages |
| Blast Count | Percentage of blasts in the bone marrow or peripheral blood |
| Genetic Abnormalities | Presence of specific genetic mutations or chromosomal abnormalities |
Accurate diagnosis and classification of MDS are vital. They help determine prognosis and guide treatment decisions.
Differential Diagnosis of MDS
MDS diagnosis is about figuring out if it’s the cause of low blood cell counts. It’s important to do a detailed check-up to be sure.
Other Causes of Cytopenia
Cytopenia, a sign of MDS, can also happen for other reasons. For example, aplastic anemia makes the bone marrow stop making blood cells. Or, not enough vitamin B12 or folate can also cause low blood cell counts.
Other things that might cause cytopenia include chronic diseases like HIV/AIDS or hepatitis. Some medicines, like chemotherapy or drugs that weaken the immune system, can also cause it. Even tumors or fibrosis in the bone marrow can lead to cytopenia.
Distinguishing MDS from Related Conditions
Telling MDS apart from AML is key. AML has more blasts in the bone marrow or blood than MDS does.
The World Health Organization (WHO) has rules to tell MDS from AML and other blood disorders. They look at things like the number of blasts in the bone marrow.
“The differential diagnosis of MDS requires a thorough check-up. This includes looking at cell shapes, testing for specific proteins, checking the chromosomes, and doing molecular studies.”
Source: Hematology guidelines
| Condition | Key Diagnostic Features |
| MDS | Dysplasia in one or more myeloid lineages, |
| AML | ≥20% blasts in bone marrow or peripheral blood |
| Aplastic Anemia | Bone marrow failure with pancytopenia, absence of dysplasia |
In conclusion, figuring out if someone has MDS means looking closely at their symptoms and test results. This helps tell it apart from other blood disorders.
Types of Myelodysplastic Syndromes
MDS can be divided into different types based on the number of lineages affected. This helps us understand the disease better and how to manage it.
MDS with Single Lineage Dysplasia
MDS with single lineage dysplasia (MDS-SLD) shows dysplasia in just one lineage. It often leads to anemia. The bone marrow shows changes in erythroid, granulocytic, or megakaryocytic lineages.
The disease’s course can vary. Some patients stay stable for a long time. Others may see their disease worsen or turn into acute myeloid leukemia (AML).
MDS with Multilineage Dysplasia
MDS with multilineage dysplasia (MDS-MLD) has dysplastic changes in two or more lineages. This type has a more complex presentation and a worse prognosis than MDS-SLD.
Patients with MDS-MLD often have several types of cytopenias. This includes anemia, neutropenia, and thrombocytopenia. It shows the involvement of multiple lineages.
Distinguishing between MDS-SLD and MDS-MLD is key for planning treatment. It helps doctors tailor care to each patient’s needs.
- MDS-SLD involves dysplasia in one lineage.
- MDS-MLD involves dysplasia in multiple lineages.
- Accurate classification is vital for management.
A leading hematologist notes, “Classifying MDS into subtypes like MDS-SLD and MDS-MLD is critical for patient care and outcomes.”
Risk Factors and Causes of MDS
It’s important to know the risk factors and causes of Myelodysplastic Syndrome (MDS) for early treatment. MDS is a group of disorders with ineffective blood cell production. It’s influenced by genetics, environment, and demographics.
Primary vs. Secondary MDS
MDS can be primary (de novo) or secondary. Primary MDS happens without known risk factors. Secondary MDS is linked to past treatments or toxins.
Secondary MDS often has a worse outlook. This is because of the damage from past treatments or exposures.
Environmental and Genetic Risk Factors
Many environmental and genetic factors contribute to MDS. Environmental risk factors include benzene, pesticides, and heavy metals. Genetic risk factors involve mutations in genes like TP53, ASXL1, and RUNX1.
The image below shows how genetics and environment interact in MDS.
Knowing these risk factors helps in early detection and treatment of MDS. More research is needed to better understand and treat MDS.
Disease Progression and Prognosis
Myelodysplastic Syndrome (MDS) is a group of disorders with different outcomes. The disease’s progress and how well patients do can change a lot. This depends on the type of MDS, any genetic changes, and the patient’s health.
Natural History of MDS
The disease starts with a slow decline in bone marrow function. This leads to low blood counts. Some patients stay stable for years, but others quickly get worse.
The type of MDS affects how the disease goes. For example, those with MDS in one blood cell line often do better than those with it in multiple lines.
Transformation to Acute Myeloid Leukemia
One big worry in MDS is turning into Acute Myeloid Leukemia (AML). The chance of this happening depends on the MDS type and genetic changes.
Patients with high-risk MDS are more likely to get AML. The International Prognostic Scoring System (IPSS) helps predict this risk. It also helps doctors decide on treatments.
Knowing the risks and how MDS progresses is key to managing the disease. It helps improve patient outcomes.
Treatment Approaches for MDS
Managing Myelodysplastic Syndrome (MDS) is complex. It involves supportive care and therapies that change the disease’s course. Treatment plans are made for each patient. They consider the MDS type, the patient’s health, and the risk of the disease getting worse.
Supportive Care Strategies
Supportive care is key in managing MDS. It aims to ease symptoms and enhance life quality. This includes:
- Blood transfusions to address anemia and thrombocytopenia
- Growth factors to stimulate the production of blood cells
- Antimicrobial prophylaxis to prevent infections
- Iron chelation therapy to manage iron overload resulting from frequent transfusions
Table: Supportive Care Measures in MDS
| Supportive Care Measure | Purpose | Benefits |
| Blood Transfusions | Address anemia and thrombocytopenia | Improves hemoglobin levels, reduces fatigue |
| Growth Factors | Stimulate blood cell production | Reduces need for transfusions, improves blood counts |
| Antimicrobial Prophylaxis | Prevent infections | Reduces risk of infections, improves survival |
| Iron Chelation Therapy | Manage iron overload | Reduces risk of organ damage from iron overload |
Disease-Modifying Therapies
Disease-modifying therapies aim to change MDS’s course. They can improve survival and lower the risk of turning into AML. These include:
- Immunomodulatory drugs (e.g., lenalidomide)
- Hypomethylating agents (e.g., azacitidine, decitabine)
- Intensive chemotherapy in selected cases
The choice of therapy depends on several factors. These include the MDS subtype, patient health, and genetic mutations.
In conclusion, treating MDS needs a detailed approach. It combines supportive care and therapies that change the disease. Understanding these options helps healthcare providers create personalized plans. These plans aim to improve patient outcomes.
Conclusion
Myelodysplastic syndrome (MDS) is a complex group of blood disorders. It affects how blood cells are made and can lead to leukemia. Doctors need to understand MDS well to make the right diagnosis and treatment plans.
A detailed look at MDS shows that anemia is a common problem. Doctors use several methods to diagnose MDS. These include checking the blood and bone marrow.
Managing MDS requires a personalized approach. This includes supportive care and treatments that target the disease. Knowing how MDS works helps doctors improve patient care and life quality.
In summary, MDS is a complex disorder. It needs a detailed summary to help doctors and improve patient care.
FAQ
What is myelodysplastic syndrome (MDS)?
Myelodysplastic syndrome (MDS) is a group of disorders. They are caused by poorly formed or dysfunctional blood cells. This often leads to cytopenia, which is a lack of certain blood cells, like anemia.
What is the most common finding in myelodysplastic syndrome?
The most common finding in MDS is cytopenia. This often shows up as anemia, neutropenia, or thrombocytopenia.
How is MDS diagnosed?
MDS is diagnosed through a detailed diagnostic process. This includes looking at peripheral blood, bone marrow, and blood cell morphology. It checks for dysplastic changes and ringed sideroblasts.
What are the different types of MDS?
MDS has different types. These are classified based on the WHO and IPSS systems. They include MDS with single lineage dysplasia and multilineage dysplasia.
What are the risk factors for developing MDS?
Several factors can increase the risk of getting MDS. These include primary and secondary MDS, and genetic and environmental factors. Exposure to certain chemicals and genetic abnormalities are examples.
How does MDS progress?
MDS can progress to acute myeloid leukemia (AML). The progression varies based on the subtype and individual factors.
What are the treatment approaches for MDS?
Treatments for MDS include supportive care and disease-modifying therapies. Supportive care includes blood transfusions. Disease-modifying therapies include immunomodulatory agents and hypomethylating agents.
What is the significance of ringed sideroblasts in MDS?
Ringed sideroblasts are a key feature in some MDS subtypes. They show abnormal iron accumulation in mitochondria. This is linked to specific genetic abnormalities.
How does MDS affect different populations?
MDS affects different populations in different ways. The incidence rates vary based on age, sex, and environmental exposure.
What is the role of genetic abnormalities in MDS?
Genetic abnormalities are key in MDS development and progression. Specific mutations and chromosomal abnormalities contribute to the disease.
What is the International Prognostic Scoring System (IPSS)?
The IPSS is a prognostic scoring system for MDS. It predicts patient outcomes based on cytopenias, blast percentage, and karyotype.





