Last Updated on October 21, 2025 by mcelik
Sepsis affects over 1.7 million adults in the United States each year. It leads to more than 270,000 deaths annually.
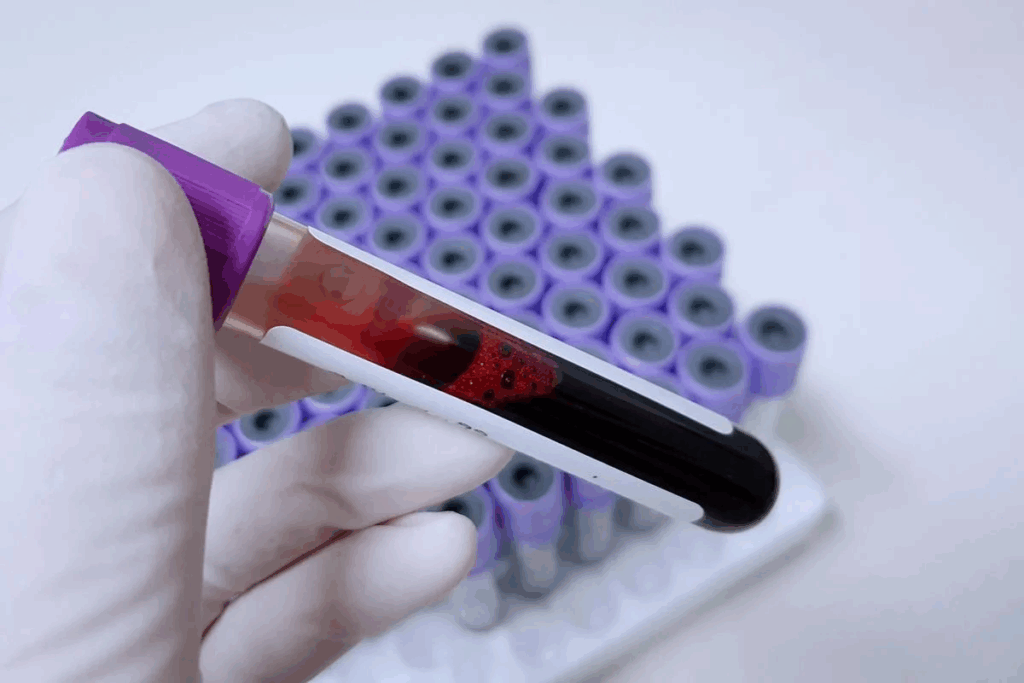
A Complete Blood Count (CBC) is key to spotting sepsis. It checks different blood parts, like white blood cells. These can show if there’s an infection and help identify CBC and sepsis indicators.
Knowing the signs of sepsis in a CBC is important. It helps find sepsis early. Changes in white blood cell counts can mean sepsis is starting.
Key Takeaways
- Sepsis is a life-threatening condition that needs quick diagnosis.
- CBC is a vital test for finding sepsis signs.
- Changes in white blood cell count can signal sepsis.
- Early detection through CBC can improve sepsis treatment outcomes.
- CBC results help healthcare providers spot sepsis signs.
Understanding Sepsis: A Life-Threatening Condition

Sepsis is a serious condition where the body’s response to an infection harms its own tissues and organs. This damage is due to a dysregulated host response to infection. It’s vital to catch it early and treat it quickly.
Definition and Pathophysiology of Sepsis
Sepsis is a severe condition that harms organs due to an infection. The pathophysiology of sepsis involves a complex battle between the pathogen and the host’s immune system. This battle can lead to organ failure if not treated fast.
The journey from infection to sepsis is complex. It depends on the pathogen’s strength, the infection site, and the host’s immune response. Knowing these factors helps in early sepsis diagnosis and treatment.
Sepsis Progression: From Infection to Septic Shock
The progression of sepsis differs from person to person. It depends on age, health, and how quickly and well medical care is given. Sepsis can turn into septic shock, a severe condition with a high risk of death.
It’s key for healthcare providers to know the stages of sepsis progression. Recognizing when sepsis turns into septic shock is critical. It means the patient’s condition has worsened, needing more aggressive treatment.
Epidemiology and Mortality Rates
The epidemiology of sepsis shows it’s a major cause of illness and death worldwide. It affects millions each year. The mortality rates of sepsis are high, showing the need for quick action.
Research indicates sepsis cases are rising. This is due to an aging population and more chronic diseases. Knowing the epidemiology of sepsis helps in finding ways to improve patient outcomes.
The Complete Blood Count (CBC): A Fundamental Diagnostic Tool

The CBC test is a key tool for doctors to check health. It looks at many parts of the blood to see how well someone is doing.
Components of a CBC Test
A CBC test checks several important things:
- Red Blood Cell (RBC) count
- White Blood Cell (WBC) count
- Platelet count
- Hemoglobin (Hb) level
- Hematocrit (Hct) level
- Red Blood Cell indices
These parts tell us about oxygen transport, fighting infections, and blood clotting.
Normal Reference Ranges
Knowing the normal ranges for CBC tests is key. These ranges can change a bit between labs. But usually, they are:
| Parameter | Normal Range |
| RBC Count | 4.32-5.72 million cells/μL (male) |
| WBC Count | 4,500-11,000 cells/μL |
| Platelet Count | 150,000-450,000/μL |
| Hemoglobin (Hb) | 13.5-17.5 g/dL (male) |
| Hematocrit (Hct) | 40-54% (male) |
These numbers can change with age, sex, and other things.
When and Why CBCs Are Ordered
CBCs are ordered for many reasons:
- To diagnose anemia or infection
- To monitor the effects of chemotherapy or other treatments
- To check for bleeding disorders
- To monitor overall health
Doctors might order a CBC for a routine check or because of symptoms.
CBC and Sepsis Indicators: The Critical Connection
It’s important to know how Complete Blood Count (CBC) results relate to sepsis indicators. Sepsis is a serious condition that can be life-threatening. It happens when the body overreacts to an infection. CBC tests help show if sepsis is present and how it’s progressing.
How Sepsis Affects Blood Parameters
Sepsis can change blood counts in many ways. For example, it can make white blood cell counts go up or down. It also affects platelet counts. The neutrophil-to-lymphocyte ratio (NLR) is another key area that can change.
Timeline of CBC Changes During Sepsis Progression
As sepsis gets worse, blood counts change. At first, white blood cell counts might go up as the body fights the infection. Later, these counts can drop or change in other ways.
- Early stages: Elevated WBC count and neutrophilia
- Progression: Possible decrease in WBC count, thrombocytopenia
- Severe sepsis: Big changes in many CBC parameters
Sensitivity and Specificity of CBC for Sepsis Detection
Even though CBC is helpful for spotting sepsis, it’s not perfect. It can pick up changes in blood, b, ut it isn’t always specific to sepsis. So, doctors need to look at CBC results along with other signs and symptoms.
“The CBC is a fundamental diagnostic tool that, when used in conjunction with clinical evaluation, can aid in the early detection of sepsis.”
– Expert in Critical Care Medicine
In summary, the link between CBC and sepsis is key for quick detection and treatment. Knowing how sepsis changes blood counts helps doctors use CBC results better. This way, they can spot and track sepsis more effectively.
White Blood Cell Count Abnormalities in Sepsis
Abnormalities in white blood cell count are common in septic patients. Sepsis is a dangerous condition caused by the body’s reaction to an infection. It can greatly affect white blood cell counts.
Leukocytosis: Elevated WBC Count
Leukocytosis, or an elevated white blood cell count, is a common response to sepsis. It shows the body is fighting an infection. The normal range for WBC count is between 4,500 and 11,000 cells per microliter. In sepsis, this count can rise significantly.
Leukopenia: Decreased WBC Count
On the other hand, some septic patients may have leukopenia, a decreased WBC count. This condition can indicate a more severe infection where the body’s response is overwhelmed.
Neutrophilia and Left Shift
Neutrophilia, an increase in neutrophils, is often seen in sepsis. A “left shift” refers to the presence of immature neutrophils in the blood. It indicates an increased production of neutrophils in response to infection.
Lymphopenia in Sepsis
Lymphopenia, or a decrease in lymphocytes, can also occur in septic patients. This condition may reflect the severity of the infection and the body’s immune response.
The following table summarizes the white blood cell count abnormalities in sepsis:
| Condition | Description | Implication in Sepsis |
| Leukocytosis | Elevated WBC count | The body’s response to infection |
| Leukopenia | Decreased WBC count | Severe infection, overwhelmed immune response |
| Neutrophilia | Increase in neutrophils | Response to bacterial infection |
| Left Shift | Presence of immature neutrophils | Increased neutrophil production |
| Lymphopenia | Decrease in lymphocytes | Severity of infection, immune response |
“The white blood cell count is a critical parameter in diagnosing and managing sepsis. Abnormalities in WBC count can indicate the severity of the condition and guide treatment decisions.”
– Expert in Critical Care Medicine
Understanding these abnormalities is key for healthcare providers to diagnose and manage sepsis effectively.
Neutrophil Changes as Key Sepsis Indicators
Neutrophils play a big role in our body’s defense. They change a lot when we have sepsis. These changes help doctors spot sepsis early.
Neutrophil-to-Lymphocyte Ratio (NLR)
The Neutrophil-to-Lymphocyte Ratio (NLR) is important for checking sepsis. A high NLR means our immune system is out of balance. This often happens with serious infections.
Research shows that a high NLR can lead to worse outcomes for septic patients.
Immature Granulocytes and Band Cells
Seeing immature granulocytes and band cells in the blood is a big sign of sepsis. These cells come from the bone marrow when we’re very sick. They show our body is fighting hard.
Spotting these cells early can help doctors catch sepsis before it gets worse.
Neutrophil Morphology Changes
Neutrophils can also change shape when we’re sick. This includes things like toxic granulation and vacuolization. These changes show our body is fighting off an infection.
In summary, changes in neutrophils are key signs of sepsis. These include a high NLR, immature granulocytes, and changes in neutrophil shape. Spotting these signs early helps doctors treat sepsis quickly.
Red Blood Cell Abnormalities Associated with Sepsis
It’s key to know about red blood cell changes in sepsis for the best care. Sepsis, a serious condition, can change red blood cell counts. These changes are important for diagnosing and treating the condition.
Anemia in Sepsis: Causes and Significance
Anemia often happens in septic patients. It’s caused by inflammation, fewer red blood cells being made, and more destruction. Anemia can really affect how well a patient does, leading to less oxygen in tissues.
Anemia in sepsis comes from many sources. Pro-inflammatory cytokines can stop red blood cell production and cause nutritional issues. Knowing why anemia happens is key to treating it well in septic patients.
Red Cell Distribution Width (RDW) Changes
The Red Cell Distribution Width (RDW) shows how different red blood cells are. High RDW values in septic patients mean more variation in cell size. This can mean worse outcomes and a higher risk of death.
RDW changes in sepsis come from many things. These include poor nutrition, inflammation, and oxidative stress. Watching RDW helps see how severe sepsis is and how well treatment is working.
Hemoglobin and Hematocrit Alterations
Hemoglobin and hematocrit levels change in sepsis. This is due to dilution, inflammation, and fewer red blood cells being made. Changes in these levels are very important because they affect how well oxygen gets to tissues.
Keeping an eye on hemoglobin and hematocrit is critical for septic patients. It helps doctors see how bad anemia is and decide if blood transfusions are needed.
Platelet Count Abnormalities in Septic Patients
Platelet count changes are common in septic patients. These changes show how severe the condition is. The complete blood count (CBC) test includes platelet count, which is key.
Thrombocytopenia: A Common Finding
Thrombocytopenia, or low platelet count, is often seen in septic patients. It can lead to more serious health issues and even death. Several factors cause thrombocytopenia in sepsis, like platelet consumption, impaired production, and increased destruction.
A study found that thrombocytopenia can predict death in septic patients.
“Thrombocytopenia is a common complication of sepsis and is associated with a higher risk of death.”
Mean Platelet Volume (MPV) Changes
Mean platelet volume (MPV) is also affected in sepsis. MPV shows the average size of platelets. Changes in MPV can show how severe sepsis is and how the body is fighting the infection.
An elevated MPV might mean more platelet turnover. A decreased MPV could point to bone marrow issues.
Platelet-to-Lymphocyte Ratio (PLR)
The platelet-to-lymphocyte ratio (PLR) is a new marker in sepsis studies. It’s the platelet count divided by the lymphocyte count. An elevated PLR is linked to worse outcomes in septic patients.
PLR helps understand the balance between inflammation and immune response in sepsis.
Early Detection of Sepsis Through CBC Parameters
Sepsis is a serious condition that can be caught early through CBC tests. The Complete Blood Count (CBC) is a key tool for doctors. It helps spot early signs of sepsis, which can save lives.
Subtle CBC Changes Before Clinical Manifestations
Even before symptoms show, CBC tests can pick up small changes. These might include changes in white blood cells, neutrophil-to-lymphocyte ratio, and platelet count. Spotting these early signs is vital for quick action.
Key CBC Changes:
- White Blood Cell Count (WBC) abnormalities
- Neutrophil-to-Lymphocyte Ratio (NLR) alterations
- Platelet count variations
High-Risk Patient Monitoring with CBC
For high-risk patients, regular CBC tests are key. These include those with weak immune systems, chronic illnesses, or after major surgeries. Regular checks can catch sepsis early in these groups.
| Patient Group | CBC Parameter | Significance |
| Immunocompromised | WBC Count | Early signs of infection |
| Chronic Illness | NLR | Indicator of systemic inflammation |
| Post-Surgery | Platelet Count | Potential sign of sepsis or DIC |
Combining CBC with Vital Signs for Early Warning
Using CBC results with vital signs gives a full picture of a patient’s health. Signs like heart rate, breathing rate, and blood pressure, when checked with CBC, help spot sepsis early. This way, doctors can start treatment sooner.
By using CBC and vital signs together, doctors can catch sepsis sooner. This improves care and outcomes for patients.
CBC and Organ Dysfunction Assessment in Sepsis
The Complete Blood Count (CBC) is key in checking organ function in septic patients. Sepsis can harm many organs, like the liver and kidneys. The CBC shows how much damage has been done.
Hematological Markers of Liver Dysfunction
Liver problems in sepsis can show up in the CBC. For example, bilirubin levels and white blood cell count changes can mean liver issues. This is because of the body’s fight against infection.
CBC Indicators of Kidney Involvement
Kidney issues in sepsis, like acute kidney injury (AKI), can be seen in the CBC. Anemia and thrombocytopenia are common in septic patients with AKI. Also, the neutrophil-to-lymphocyte ratio (NLR) might help predict AKI in sepsis.
Correlation Between CBC Changes and Multiple Organ Failure
The more severe the CBC changes, the worse the organ damage. Multiple organ failure shows up with big changes in CBC, like leukocytosis or leukopenia, thrombocytopenia, and anemia. Watching these changes helps catch sepsis early and treat it right.
In short, CBC is very important for checking organ damage in sepsis. Doctors use it to understand how bad sepsis is and how many organs are affected. This helps them make the right treatment plans quickly.
Sepsis-Related Blood Clotting Issues Reflected in CBC
Disseminated intravascular coagulation (DIC) is a serious condition linked to sepsis. CBC tests are key in spotting it. Sepsis messes with blood clotting, causing too much clotting or bleeding. CBC tests, along with others, help find these problems.
DIC Markers
DIC is marked by both clotting and bleeding. It happens when the body’s clotting system goes into overdrive. This leads to many small clots in blood vessels. It uses up platelets and clotting factors, which can cause bleeding.
Key signs of DIC include:
- Low platelet count: Thrombocytopenia is common in DIC because platelets are used up in clotting.
- Prolonged PT and aPTT: PT and aPTT are often long because clotting factors are low.
- Elevated D-dimer: D-dimer goes up because of fibrin breakdown.
- Low fibrinogen levels: Fibrinogen, a key clotting factor, is used up, leading to low levels.
Platelet Function Abnormalities
Sepsis can also mess with platelet function. Platelets don’t work right, which can lead to bleeding or clotting problems. CBC tests can show platelet count and shape, helping to check platelet function.
Monitoring Coagulopathy with CBC and Complementary Tests
Tracking coagulopathy in sepsis needs CBC tests and other tests. Regular CBCs track changes in platelet count and other blood factors. Tests like PT, aPTT, D-dimer, and fibrinogen levels give a full picture of clotting status.
Using these tests together, doctors can manage sepsis-related clotting better. They can tailor treatment to each patient’s needs.
Limitations of CBC in Sepsis Diagnosis
The CBC is useful but has its limits in diagnosing sepsis. Its parameters are not specific enough. Healthcare providers must keep these limits in mind when looking at CBC results.
Non-Specific Nature of CBC Changes
One big problem with using CBC for sepsis is that the changes are not specific. Many conditions can cause similar changes in blood tests. This makes it hard to know for sure if someone has sepsis just by looking at CBC results.
An elevated white blood cell count can mean sepsis, but it can also mean other things, like trauma or surgery. So, it’s important to think about the whole situation when looking at CBC results.
Impact of Pre-existing Conditions on Interpretation
Pre-existing conditions can make it harder to understand CBC results for sepsis. Patients with long-term health issues might already have abnormal CBC results. This can make it tricky to tell if they have sepsis.
For example, people with liver disease might have low platelets because of their liver. This could be mistaken for sepsis. So, it’s key to know a patient’s health history when looking at CBC results.
| Pre-existing Condition | Potential CBC Abnormality | Impact on Sepsis Diagnosis |
| Chronic Kidney Disease | Anemia | May mask or mimic sepsis-related anemia |
| Hematological Disorders | Abnormal WBC count | Can complicate the interpretation of sepsis-related WBC changes |
| Chronic Liver Disease | Thrombocytopenia | May be misattributed to sepsis-induced DIC |
Timing Considerations in CBC Analysis
When to do CBC tests is very important for sepsis diagnosis. How often and when you do the tests can help find sepsis early.
It’s good to do CBC tests regularly, but how often is up for debate. High-risk patients should be tested more often to catch sepsis early.
Complementary Tests to Enhance Sepsis Detection
Tests like CBC are just the start in finding sepsis. Other tests give more details to help doctors diagnose and treat sepsis better.
Biomarkers: Procalcitonin, CRP, and Lactate
Biomarkers like procalcitonin, CRP, and lactate are key in spotting sepsis. Procalcitonin levels go up with bacterial infections. This makes it great for telling apart bacterial and viral infections or inflammation not caused by infection.
CRP shows inflammation. It’s not just for sepsis, but high levels help confirm it when looked at with other signs and tests.
Blood Culture and Microbiology Tests
Blood cultures are the top choice for finding the cause of sepsis. They grow bacteria or fungi from blood samples. This info is key for choosing the right antibiotics.
Microbiology tests like Gram staining and susceptibility testing help find the exact pathogen and its antibiotic resistance. This guides treatment choices.
Organ Function Tests in Sepsis Evaluation
Checking how organs work is key in sepsis. Tests like serum creatinine for the kidneys, liver enzymes for the liver, and arterial blood gases for breathing help see how organs are doing.
These tests help doctors keep track of sepsis and how well treatments are working. This lets them make changes to treatment plans as needed.
Conclusion: The Value of CBC in Sepsis Management
The Complete Blood Count (CBC) is key in managing sepsis. It gives vital info on the patient’s health and how they’re doing with treatment. Doctors can spot early signs of sepsis and track how it’s progressing.
What makes CBC so valuable is that it gives a full picture of the patient’s blood health. Changes in white blood cells, neutrophil-to-lymphocyte ratio, and platelets can show sepsis. It also helps when used with other tests and checks to find and watch sepsis better.
In short, CBC is essential in treating sepsis. It helps doctors make better choices and improve patient care. By using CBC results in a complete care plan, doctors can better treat sepsis and lower the chance of serious problems.
FAQ
What are the common signs of sepsis in a Complete Blood Count (CBC) test?
Signs of sepsis in a CBC include changes in white blood cell count. This can be an increase or a decrease. Neutrophilia with a left shift, lymphopenia, and thrombocytopenia are also common. Changes in red blood cell indices are another sign.
How does sepsis affect white blood cell count?
Sepsis can cause white blood cell counts to go up or down. Neutrophilia with a left shift is common. This means the bone marrow is releasing more immature neutrophils.
What is the significance of the neutrophil-to-lymphocyte ratio (NLR) in sepsis?
The NLR is a marker of inflammation. It is often higher in sepsis. A higher NLR is linked to more severe cases and higher mortality rates.
Can CBC detect sepsis early?
CBC is not definitive for sepsis. But it can show early signs through changes in blood parameters. This includes white blood cell count abnormalities before symptoms appear.
How does sepsis affect platelet count?
Sepsis often causes a decrease in platelet count. This is known as thrombocytopenia. It can indicate how severe the sepsis is and if there’s a risk of DIC.
What is the role of CBC in monitoring organ dysfunction in sepsis?
CBC can show signs of organ dysfunction in sepsis. It can indicate liver and kidney problems. These signs can show how severe the sepsis is and if there’s a risk of multiple organ failure.
Are CBC changes specific to sepsis?
No, CBC changes seen in sepsis are not specific. They can also be seen in other conditions. So, CBC results need to be looked at with the patient’s symptoms and other tests in mind.
What complementary tests can be used alongside CBC to enhance sepsis detection?
Tests like procalcitonin, CRP, and lactate can be used with CBC. Blood cultures, microbiology tests, and organ function tests also help improve sepsis detection and management.
How does sepsis affect red blood cell indices?
Sepsis can cause anemia and changes in red cell distribution width (RDW). It can also affect hemoglobin and hematocrit levels. These changes show how severe the condition is and whether there’s organ dysfunction.
Can pre-existing conditions affect the interpretation of CBC in sepsis?
Yes, pre-existing conditions can change CBC parameters. They can affect how CBC results are interpreted in sepsis. Clinicians need to consider these factors when looking at CBC results.
How does CBC help in assessing sepsis-related blood clotting issues?
CBC can show signs of blood-clotting problems in sepsis. This includes thrombocytopenia and changes in coagulation parameters. These signs help guide further evaluation and management.
References
- Agnello, L., Biglia, C., Bruno, R. M., et al. (2021). The value of a complete blood count for sepsis diagnosis and prognosis. Medicina (Kaunas), 57(10), 1107. https://pmc.ncbi.nlm.nih.gov/articles/PMC8534992/