Last Updated on November 27, 2025 by Bilal Hasdemir

We are dedicated to giving top-notch cancer care. Radiation oncology is key in this effort. Radiation therapy, or XRT, uses high-energy particles or waves to treat cancer and some non-cancerous conditions.
Radiation oncology is a part of oncology that uses radiation to fight cancer cells. XRT, or external radiation therapy, is a common method. It targets cancer cells while protecting healthy tissue nearby.Get the ultimate radiation oncology meaning in our powerful guide. Discover what XRT means and other amazing essential medical terms in this field.
Key Takeaways
- Radiation oncology is a medical specialty that uses radiation to treat cancer and some non-cancerous conditions.
- XRT stands for external radiation therapy, a common treatment approach for cancer.
- Radiation therapy is used to kill or control the growth of malignant cells.
- Radiation oncology is a subspecialty of oncology that focuses on using radiation to treat cancer.
- Effective cancer care often involves a combination of treatments, including radiation therapy.
Radiation Oncology: A Comprehensive Overview
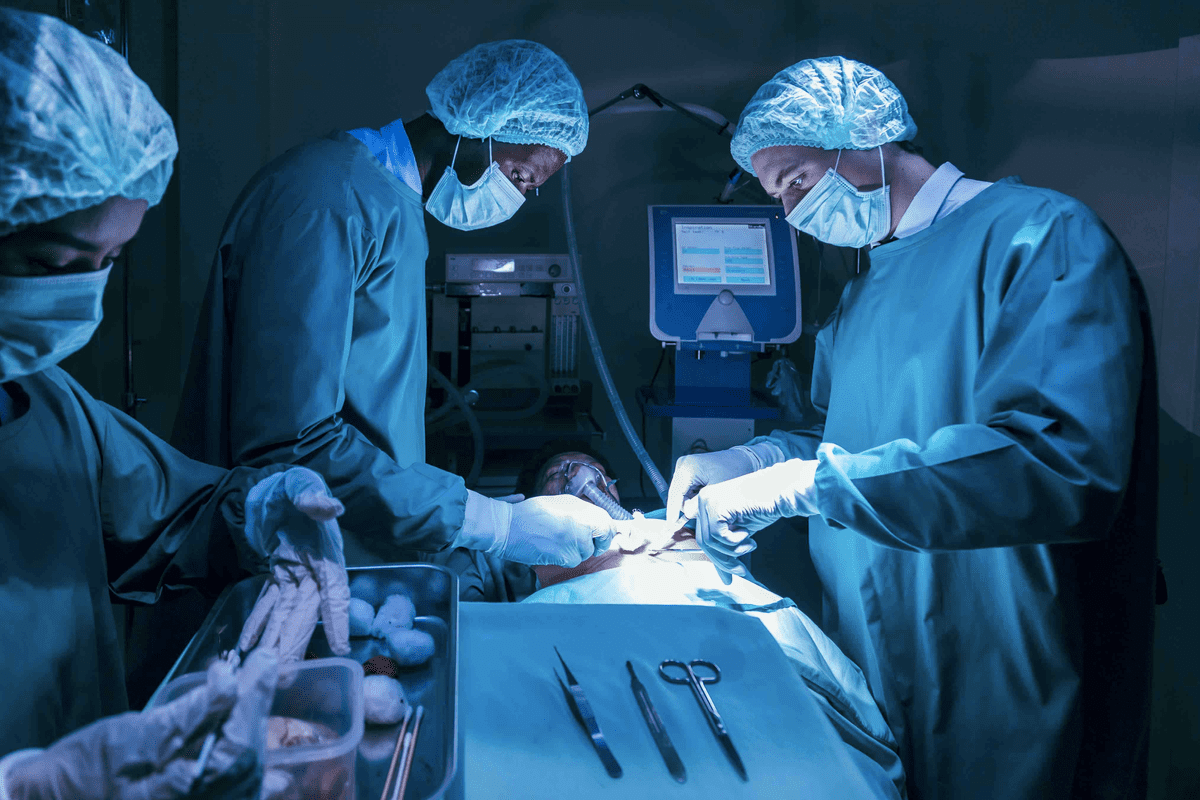
Radiation oncology is a medical field that fights cancer. It has a long history and keeps getting better. A team of experts, like radiation oncologists and therapists, works together to treat cancer well.
Definition and Scope of the Specialty
Radiation oncology uses radiation to fight cancer. It covers many areas, from diagnosing to treating cancer with radiation. We use new tech to hit cancer cells hard but spare healthy tissues.
It needs a lot of knowledge in radiation and cancer. Doctors plan treatments that fit each patient’s needs. They consider the cancer type, stage, and where it is, and the patient’s health.
Historical Development of Radiation as Cancer Treatment
Radiation therapy started in the early 1900s, after X-rays were discovered. At first, it was used for many health issues, including cancer. As we learned more about radiation, we got better at treating cancer.
From old methods to new ones like IMRT, radiation oncology has changed a lot. Now, we use advanced tech like SBRT and proton therapy. These help give treatments that are more precise and effective.
Terminology Variations in Radiation Therapy

Radiation therapy is a key part of cancer treatment. It has different names and spellings in various places and medical texts. Knowing these differences is important for doctors and patients.
Common Spellings: Radiotherapy, Radiotherapy, Radiotherapy
In English-speaking areas, “radiotherapy” is the usual term. But, you might see “radiotherapy and “radiotherapy” too. These come from typing mistakes or different spelling rules.
It’s key to know these to talk and write clearly and correctly.
“Radiotherapy” is the top choice in medical papers and talks. It shows it’s widely accepted by doctors.
International Terms: Radioterapia Oncologica and Regional Variations
In Spanish-speaking areas, “radioterapia oncologica” is often used. It shows how radiation therapy fits into cancer care. Other languages have their own terms, like “radiothérapie” in French and “Radiotherapie” in German.
Knowing these terms is important today. Patients might get care in different places or talk to doctors from other countries.
Incorrect Variants: Radiotrapy, Radiotehrapy, Radiotherpay
Some spellings, like “radiotrapy,” “radiotehrapy,” and “radiotherpay,” are wrong. They come from mistakes or not understanding the correct term.
We need to watch out for these errors. This keeps medical talk clear and makes sure patients get the right info.
XRT Meaning Medical: Understanding the Abbreviation
The world of medical terms is full of abbreviations. XRT, short for External Radiation Therapy, needs to be understood. It’s key for both doctors and patients in cancer treatment and radiation oncology.
What XRT Stands For in Clinical Context
XRT means External Radiation Therapy. It’s a treatment where a machine outside the body sends beams to kill cancer cells. This method is a mainstay in cancer treatment, giving a non-invasive way to control tumors.
We use XRT to treat many cancers, like breast, prostate, lung, and head and neck cancers. It’s precise, allowing high doses of radiation to hit tumors while protecting healthy tissues.
Other Common Abbreviations: RT, RTx
There are other terms used in radiation therapy, too. RT means Radiation Therapy, covering both external and internal treatments. RTx is another term for radiation therapy, often seen in treatment plans and notes.
| Abbreviation | Meaning | Context |
| XRT | External Radiation Therapy | Specific to external beam radiation |
| RT | Radiation Therapy | General term for radiation treatments |
| RTx | Radiation Therapy | Often used in clinical documentation |
XRT vs. Other Medical Imaging Abbreviations
It’s important to know the difference between XRT and other medical imaging terms. XRT is for External Radiation Therapy, while RT and RTx are for all types of radiation therapy. Knowing these differences helps in clear communication among healthcare teams and with patients.
Experts in radiation oncology say, “Using the right terms is key for the right treatment. XRT, being a specific type of radiation therapy, needs careful planning and execution for the best results.”
“Radiation therapy is a critical component of cancer treatment, and understanding the nuances of abbreviations like XRT is essential for effective patient care.”
Expert in Radiation Oncology
The Science Behind Radiation Therapy
Radiation therapy is a treatment that uses ionizing radiation to harm cancer cells. It damages their DNA, stopping them from growing. This method targets cancer cells more than normal cells, making it effective.
How Radiation Affects Cancer Cells
Radiation therapy sends ionizing radiation to the tumor. This radiation harms the DNA of cancer cells, stopping them from dividing. Over time, these cells die, and the tumor gets smaller.
We use advanced technology to aim the radiation at the tumor. This helps protect healthy tissues around it.
The success of radiation therapy depends on several factors. These include the cancer type and stage, and the patient’s health. By planning and delivering the right amount of radiation, we aim to treat the cancer well while keeping side effects low.
Types of Radiation Used in Treatment
There are different types of radiation used in cancer treatment. Each type has its own use and benefits. The choice depends on the tumor’s location and the patient’s needs.
| Type of Radiation | Description | Common Applications |
| Photon Radiation | High-energy X-rays that penetrate deep into the body | Treating tumors in various parts of the body, including deep-seated tumors |
| Proton Radiation | Protons that release energy at a specific depth, reducing damage to surrounding tissue | Treating tumors close to critical structures or in sensitive areas |
| Electron Radiation | Electrons that penetrate to a certain depth, depending on their energy | Treating superficial tumors or areas just beneath the skin |
Understanding radiation therapy and its types helps us create personalized treatment plans. This approach improves the care we give our patients.
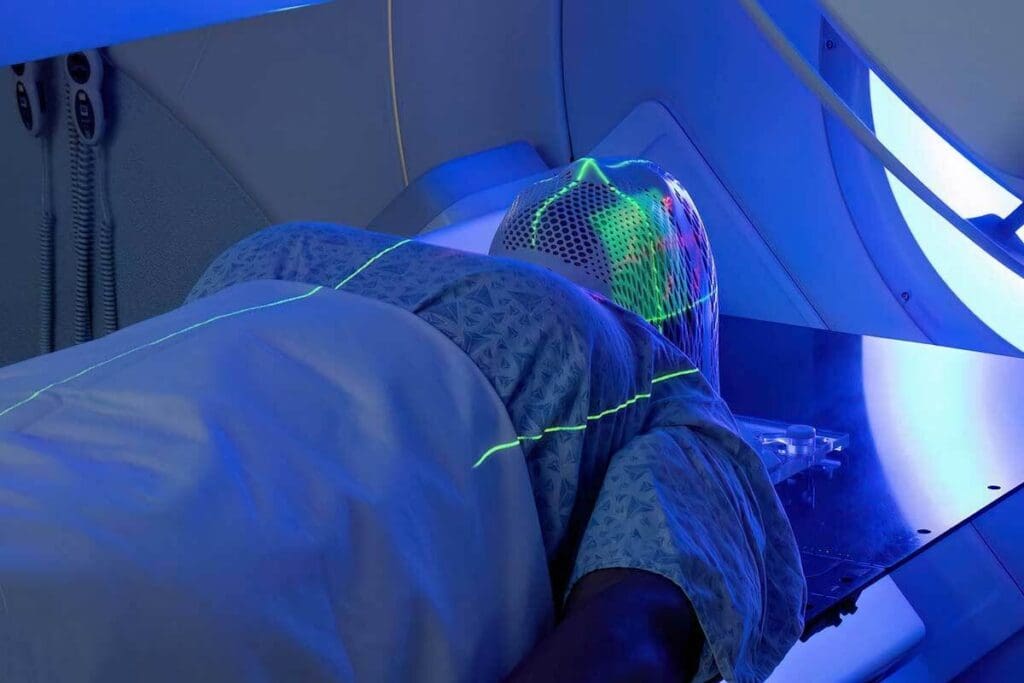
External Beam Radiation Therapy (XRT) Explained
External Beam Radiation Therapy (XRT) is a key cancer treatment. It sends high-energy beams from outside the body to kill cancer cells. We use the latest tech to make sure the radiation hits the right spot, keeping healthy tissues safe.
Treatment Techniques
XRT uses different methods to fit each patient’s needs. Some main techniques are:
- 3D Conformal Radiation Therapy: This method shapes beams to fit the tumor, ensuring accurate doses.
- Intensity-Modulated Radiation Therapy (IMRT): IMRT changes beam intensity for more precise tumor targeting and less damage to nearby areas.
- Image-Guided Radiation Therapy (IGRT): IGRT takes images before and during treatment to ensure radiation is delivered correctly.
Modern Delivery Methods
Today’s XRT methods have greatly improved treatment results. Some key advancements are:
| Technique | Description | Benefits |
| Volumetric Modulated Arc Therapy (VMAT) | Delivers radiation in a continuous arc around the patient | Reduces treatment time, improves dose distribution |
| Stereotactic Body Radiation Therapy (SBRT) | Highly precise radiation delivery to small tumors | Effective for early-stage cancers, fewer sessions required |
| Proton Therapy | Uses protons instead of X-rays to kill cancer cells | Reduces damage to surrounding healthy tissue, beneficial for kids |
These new methods have made XRT more effective and safe. They help us treat many cancers better. We keep improving our tech to give our patients the best care possible.
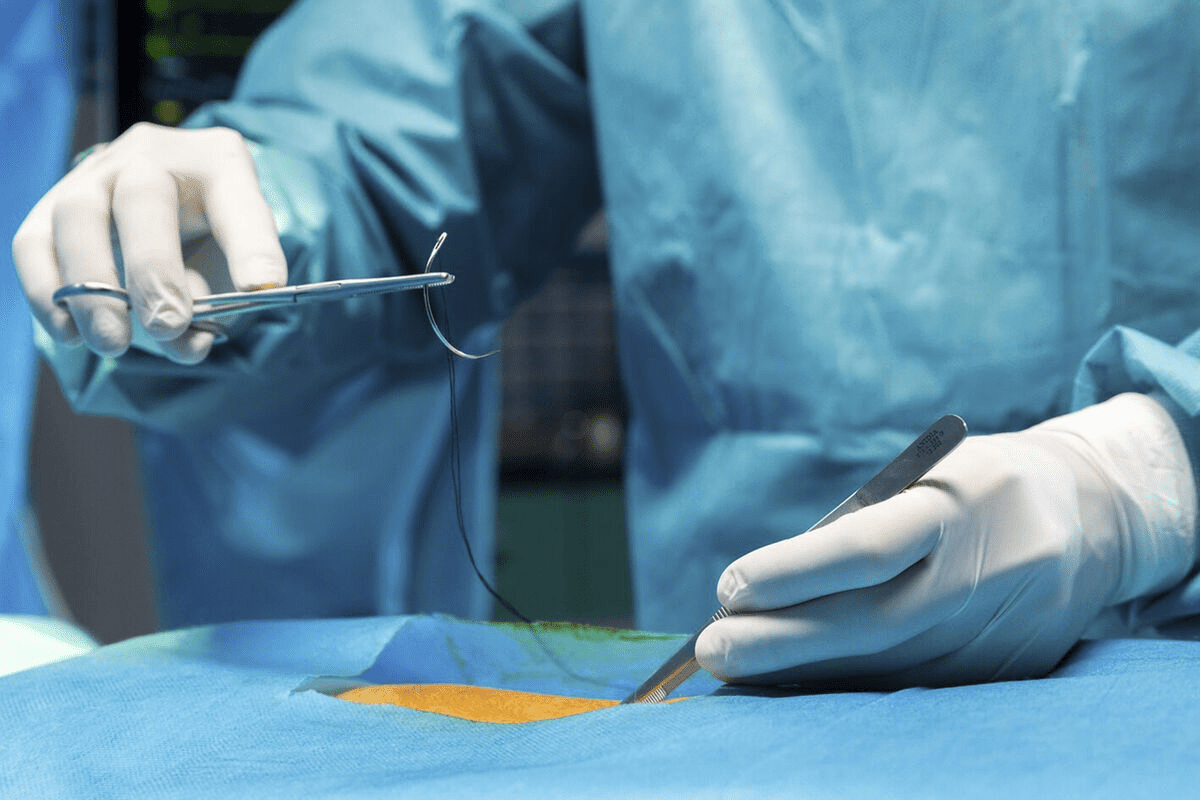
Internal Radiation: Brachytherapy and Bradytherapy
Internal radiation therapy is a precise way to treat cancer. It involves putting radioactive material inside or near the tumor. This method allows for high doses of radiation to be given to specific areas. It also helps protect healthy tissues around the tumor.
How Internal Radiation Differs from XRT
Internal radiation therapy is different from External Beam Radiation Therapy (XRT). XRT sends radiation from outside the body. But internal radiation places the source right inside or near the tumor. This makes brachytherapy more focused and reduces side effects on nearby tissues.
Placement Methods and Applications
Brachytherapy uses different ways to place radioactive materials. These include temporary or permanent implants. The choice depends on the cancer type, tumor location, and the patient’s needs. It’s often used for prostate, breast, and cervical cancers.
- Permanent implants for prostate cancer
- Temporary implants for breast cancer
- Intracavitary brachytherapy for cervical cancer
Advantages and Limitations
The benefits of internal radiation therapy include delivering high doses of radiation directly to the tumor. This reduces damage to nearby tissues. But it needs special skills and tools. Not all cancers can be treated this way.
In summary, brachytherapy is a valuable treatment for many cancers. It provides a focused and effective way to use radiation therapy.
Common Cancers Treated with Radiation Therapy
Radiation therapy is used for many cancers, like breast, prostate, lung, and head and neck cancers. It’s chosen based on the cancer’s type, stage, and where it is. This makes it a flexible treatment option.
Breast Cancer
Radiation therapy is key for breast cancer, after surgeries like lumpectomy or mastectomy. It kills any cancer cells left in the breast, chest wall, or underarm area. This lowers the chance of cancer coming back. We use external beam radiation therapy to hit the right spots.
Prostate Cancer
For prostate cancer, radiation is a main treatment for cancers that are close or have spread a bit. Brachytherapy puts radioactive seeds right in the prostate. This method gives high doses of radiation to the tumor but not to other tissues.
Lung Cancer
Lung cancer treatment often includes radiation, alone or with surgery or chemotherapy. Stereotactic body radiation therapy (SBRT) is used for small lung tumors. It gives precise, high doses of radiation. This helps keep lung function good and side effects low.
Head and Neck Cancers
Head and neck cancers, like those in the mouth, throat, and nose, are often treated with radiation. The goal is to stop the tumor while keeping the area working and looking good. Intensity-modulated radiation therapy (IMRT) is used to target the tumor well but not harm nearby important areas.
These examples show how radiation therapy is used for different cancers. By matching the treatment to the cancer, we can get better results and improve life quality for patients.
Radiation Medicine: Beyond Cancer Treatment
Radiation medicine is more than just treating cancer. It also helps with non-cancerous conditions and diagnostic tools. This shows how radiation medicine is used in many ways in healthcare.
Non-Malignant Conditions Treated with Radiation
Radiation therapy is not just for cancer. It’s also used for conditions like heterotopic ossification and Graves’ ophthalmopathy. These are conditions where bone forms in soft tissues or affects the eyes.
It’s also used for macular degeneration to stop vision loss. And for severe cases of keloid formation, there is no way to reduce scar recurrence after surgery.
Diagnostic vs. Therapeutic Applications
Radiation medicine has two main uses: diagnostic and therapeutic. Diagnostic uses radiation to see inside the body. This includes X-rays, CT scans, and PET scans for diagnosing diseases.
Therapeutic uses radiation to treat diseases. It targets and destroys diseased cells or relieves symptoms. The choice between these depends on the treatment plan.
The Multidisciplinary Approach in Radiation Medicine
Radiation medicine needs a team effort. Radiation oncologists, medical physicists, radiologists, and others work together. They ensure radiation is used safely and effectively.
Creating personalized treatment plans is key. For treatments, it’s about giving the right dose to the right area. For diagnostics, it’s about choosing the best imaging method to get the needed info with low radiation.
| Application Type | Examples | Purpose |
| Diagnostic | X-rays, CT scans, and PET scans | Visualize internal structures, diagnose conditions |
| Therapeutic | Cancer treatment, heterotopic ossification, Graves’ ophthalmopathy | Treat diseases, alleviate symptoms |
Exploring radiation medicine shows its big role in healthcare. It treats non-cancerous conditions and helps with diagnostics. This highlights the need for a team approach in its practice.
The Patient Experience: What to Expect with XRT
Getting ready for XRT means knowing what to expect at each stage. We know radiation therapy can seem complex and scary. Our goal is to help you through every step, from the first meeting to aftercare, making sure you’re ready for your treatment.
Initial Consultation and Planning
Your XRT journey starts with a meeting with your radiation oncologist. They will check your condition, talk about XRT’s benefits and risks, and create a treatment plan just for you. This plan will look at your cancer type, stage, and health.
Here are some key things you’ll discuss during the initial consultation:
- Treatment goals and what you can expect
- Side effects and how to manage them
- XRT’s role in your overall treatment
Simulation and Treatment Mapping
Next, you’ll have simulation and treatment mapping. This uses CT scans to find the tumor and plan the treatment area. Your team will make a detailed map to ensure the radiation is precise.
During simulation, you might lie on a table and use immobilization devices to stay in place. This session is key to your personalized treatment plan.
Daily Treatment Sessions
Daily sessions are a big part of your XRT. They usually happen Monday to Friday, lasting from a few minutes to 30 minutes. Our therapists will make sure you’re comfortable and then give the treatment.
| Day | Time | Duration |
| Monday | 9:00 AM | 15 minutes |
| Tuesday | 9:00 AM | 15 minutes |
| Wednesday | 9:00 AM | 15 minutes |
Follow-up Care
After XRT, follow-up care is vital. It helps check how you’re doing and manage side effects. Your doctor will schedule visits to monitor your progress and offer guidance.
“Follow-up care is a critical component of the treatment process, ensuring that patients receive the support they need after XRT.” – Radiation Oncologist
Knowing what to expect with XRT helps you navigate your treatment. Our team is here to support you every step of the way.
Side Effects and Management in Radiation Treatment
It’s important for patients to know about the side effects of radiation therapy. This knowledge helps them manage their treatment better. Remember, everyone’s experience is different.
Common Acute Side Effects
Radiation therapy can cause several side effects that happen during or right after treatment. These include:
- Fatigue: Feeling very tired, which can be helped by resting and using relaxation techniques.
- Skin Changes: The treated area might get red, itchy, or dry. Using creams and gentle skin care can help.
- Hair Loss: Hair may fall out in the treated area, but it’s not always permanent.
Potential Long-term Effects
Some side effects can last a long time or even be permanent. These include:
- Fibrosis: Scarring that can change the skin’s texture or function.
- Lymphedema: Swelling due to damage to lymph nodes or vessels.
- Secondary Cancers: Though rare, there’s a small chance of getting secondary cancers in the treated area.
Knowing about these long-term effects is important for making informed decisions about care.
Strategies for Side Effect Management
Managing side effects well is key to better outcomes and quality of life. Strategies include:
- Personalized Care Plans: Tailoring treatment and support to each patient’s needs.
- Multidisciplinary Teams: Working with a team of healthcare professionals for all aspects of care.
- Patient Education: Teaching patients about their treatment and managing side effects.
Using these strategies can greatly improve the patient experience and treatment results.
Comparing Radiation Therapy with Other Cancer Treatments
Radiation therapy is a key cancer treatment. It’s often compared to surgery and chemotherapy. Knowing how radiation therapy works with these treatments is important.
Radiation vs. Surgery
Radiation therapy and surgery target cancer in one area. The choice depends on the tumor’s type, size, and location. It also depends on the patient’s health.
Surgery removes the tumor. It’s used when the cancer is in one place and can be safely taken out.
Radiation therapy kills cancer cells with high-energy rays. It can be used before or after surgery. This helps remove any remaining cancer cells.
Radiation vs. Chemotherapy
Chemotherapy uses drugs to kill cancer cells all over the body. It’s different from radiation therapy, which targets one area.
Radiation therapy is better for localized cancer. It avoids the side effects of chemotherapy. But chemotherapy can be used with radiation to make it more effective.
Combination Approaches
Often, the best treatment plan combines different methods. Combination therapy might include radiation, surgery, and chemotherapy together.
Combining treatments attacks cancer from different sides. For example, chemotherapy can shrink tumors before radiation. This makes radiation more effective.
We help patients choose the best treatment. We consider the cancer type, the patient’s health, and their preferences.
Conclusion: Advances and Future Directions in Radiation Oncology
Radiation oncology is changing fast, thanks to new research and tech. These changes help us treat cancer better and with fewer side effects. This makes a big difference for patients.
The future of radiation oncology looks bright. We’re moving towards treatments that are more precise and tailored to each patient. Thiswaysludes new waylike precision radiation therapy and immunotherapy. These advancements aim to make treatments more effective and less harsh.
Keeping research and development going is key. It helps us find new ways to fight cancer. This means we can offer better care to those fighting cancer.
We’re dedicated to top-notch healthcare and support for patients worldwide. Our goal is to give patients the best care possible. We use the latest in radiation oncology to do this.
FAQ
What does XRT stand for in medical terms?
XRT stands for External Beam Radiation Therapy. It’s a common treatment for many cancers.
What is the difference between XRT and brachytherapy?
XRT uses radiation from outside the body. Brachytherapy puts a radioactive source inside or near the tumor.
What are the common side effects of radiation therapy?
Side effects include fatigue, skin changes, and pain. The exact side effects depend on the treatment area and dose.
How is radiation therapy used in cancer treatment?
It can be used alone or with surgery and chemotherapy. It treats cancers like breast, prostate, lung, and head and neck cancers.
What is radiation oncology?
Radiation oncology uses radiation to diagnose and treat cancer. It focuses on using radiation therapy to manage and cure cancer.
Are there different types of radiation therapy?
Yes, there are different types. These include external beam radiation therapy (XRT), brachytherapy, and systemic radiation therapy. Each has its own uses and benefits.
How is XRT delivered?
XRT uses a linear accelerator. It produces high-energy X-rays that target the tumor precisely, protecting healthy tissue.
Can radiation therapy be used for non-cancerous conditions?
Yes, it can treat some non-cancerous conditions. This includes benign tumors and certain eye conditions.
What is the role of radiation medicine in patient care?
Radiation medicine is key in treating cancer and some non-cancerous conditions. It offers a team approach to care, including diagnosis, treatment, and follow-up.
How does radiation therapy compare to surgery and chemotherapy?
Radiation therapy is a localized treatment. It can be used alone or with surgery and chemotherapy. It offers a different way to fight cancer, depending on the type and stage.
What should patients expect during XRT treatment?
Patients go through a consultation, simulation, and treatment planning before starting treatment. They should also expect follow-up care to manage side effects and monitor their response.
What are the advantages of modern radiation therapy techniques?
Modern techniques like IMRT and SBRT allow for precise tumor targeting. This reduces damage to healthy tissues, improving treatment outcomes.
References
- ScienceDirect. (n.d.). Radiation oncology – an overview. https://www.sciencedirect.com/topics/medicine-and-dentistry/radiation-oncology