Last Updated on October 21, 2025 by mcelik

Myeloproliferative neoplasms (MPNs) are blood disorders that can be serious. They need to be diagnosed and treated right away. A key test for this is the MPL blood test. It helps find the MPL gene mutation, linked to some MPNs.
The MPL blood test is important for diagnosing MPNs. It finds the MPL mutation. This helps doctors to better diagnose and manage these conditions.
Key Takeaways
- The MPL blood test is used to diagnose myeloproliferative neoplasms.
- It detects the MPL gene mutation associated with certain MPNs.
- Understanding the MPL mutation is key to effective diagnosis and management.
- The test is a big step in diagnosing blood disorders.
- Early detection through the MPL blood test can lead to better patient outcomes.
Understanding the MPL Gene and Its Function
Learning about the MPL gene helps us understand how blood cells are made. The MPL gene makes a receptor that is key in signaling. This signaling helps control the making of platelets and other blood cells.
Role in Blood Cell Production
The MPL gene is vital for making megakaryocytes in the bone marrow. These cells are responsible for creating platelets. MPL works with thrombopoietin (TPO) to help these cells grow and mature.
This teamwork is important for keeping platelet levels right.
- The MPL receptor is found on megakaryocytes and their early forms.
- When TPO binds to MPL, it starts a chain of signals. These signals help these cells live, grow, and change into platelets.
- If this process goes wrong, it can cause too many or too few platelets. This can lead to health issues.
Thrombopoietin Receptor Signaling
Thrombopoietin receptor signaling is a detailed process. It happens when TPO binds to MPL. This signaling is key for controlling the growth of megakaryocytes and platelet production.
When TPO binds to MPL, it starts a series of signals. These signals go through the JAK/STAT pathway. This pathway is important for sending messages from the cell surface to the nucleus. It affects how genes work and how cells behave.
Normal MPL Protein Function
The MPL protein works as a receptor for TPO. It helps TPO’s effects on megakaryocytes and platelet production. MPL’s job is critical for healthy blood cell making, focusing on megakaryocytes and platelets.
In short, the MPL gene and its receptor are very important for blood cell production. Understanding MPL helps us learn about healthy blood cell making and diseases related to it.
The MPL Mutation: Causes and Mechanisms

The MPL gene mutation affects the thrombopoietin receptor’s function. This leads to abnormal blood cell production. It plays a big role in myeloproliferative neoplasms (MPNs), which cause too many blood cells.
Types of MPL Gene Mutations
MPL gene mutations can differ, with some seen more in MPNs. The most common happens in exon 10. They change tryptophan to leucine at position 515 (W515L/K/A).
This change makes the thrombopoietin receptor always active, even without thrombopoietin. MPL mutations are split into types based on the genetic change. Knowing these types helps in diagnosing and treating MPNs.
Somatic vs. Germline Mutations
MPL mutations can be somatic or germline. Somatic mutations happen in non-reproductive cells and are picked up over a lifetime. They might come from environmental factors or DNA copying errors.
On the other hand, germline mutations are passed down from parents and are present in all cells. Knowing if a mutation is somatic or germline is key to disease diagnosis, outlook, and treatment. Somatic mutations are more common in MPNs and often mean a worse prognosis.
Molecular Pathways Affected
MPL mutations mess with important pathways for blood cell making. The thrombopoietin receptor, from the MPL gene, controls megakaryopoiesis and thrombopoiesis. MPL mutations activate pathways like JAK/STAT, which help cells grow and live longer.
This messes up blood cell production, leading to MPNs. Knowing how MPL mutations work is key to making new treatments.
Myeloproliferative Neoplasms (MPNs): An Overview
Myeloproliferative neoplasms (MPNs) are a group of disorders. They cause abnormal growth of blood cells. This happens because of the overproduction of different blood cells.
Classification of MPNs
MPNs are divided into several types. These types are based on their clinical and molecular features. The main types include:
- Polycythemia Vera (PV): This is when there are too many red blood cells.
- Essential Thrombocythemia (ET): It’s when there are too many platelets.
- Primary Myelofibrosis (PMF): This is when the bone marrow gets scarred.
Knowing the type of MPN is key. It helps doctors choose the right treatment and predict how well a patient will do.
Epidemiology and Risk Factors
MPNs are not very common. They affect about 1-3 people for every 100,000 each year. The risk of getting MPNs can vary. It depends on genetics and the environment.
| Subtype | Incidence | Common Risk Factors |
| Polycythemia Vera | 0.8-1.4 per 100,000/year | Advanced age, genetic mutations (e.g., JAK2) |
| Essential Thrombocythemia | 0.6-1.7 per 100,000/year | Family history, exposure to certain chemicals |
| Primary Myelofibrosis | 0.3-0.6 per 100,000/year | Exposure to radiation, genetic predisposition |
Clinical Presentation
MPNs can show up differently in each person. It depends on the type and how severe it is. Common signs include:
- Fatigue and weakness
- Splenomegaly (enlargement of the spleen)
- Bleeding or thrombotic events
- Bone pain
Getting diagnosed and treated early can really help. Knowing how MPNs present is key. It helps doctors make the right diagnosis and treatment plan.
When Is the MPL Blood Test Ordered?
The MPL blood test is ordered when doctors suspect myeloproliferative neoplasms.
Clinical Indications
Doctors order the MPL blood test for patients showing signs of essential thrombocythemia or primary myelofibrosis.
These signs include:
- Sustained elevation in platelet count
- Splenomegaly
- Thrombotic events
- Bone marrow fibrosis
Diagnostic Algorithm
Diagnosing MPNs involves clinical assessment, lab tests, and molecular diagnostics.
The MPL blood test is key in this process. It helps find MPL mutations in MPN subtypes.
Screening Recommendations
Screening for the MPL blood test depends on the patient’s situation and risk factors.
| Patient Group | Screening Recommendation |
| Patients with suspected MPNs | Recommended as part of diagnostic workup |
| Family history of MPNs | Consider screening in the absence of symptoms |
| Patients with unexplained thrombocytosis | Recommended to rule out MPNs |
The MPL Blood Test Procedure
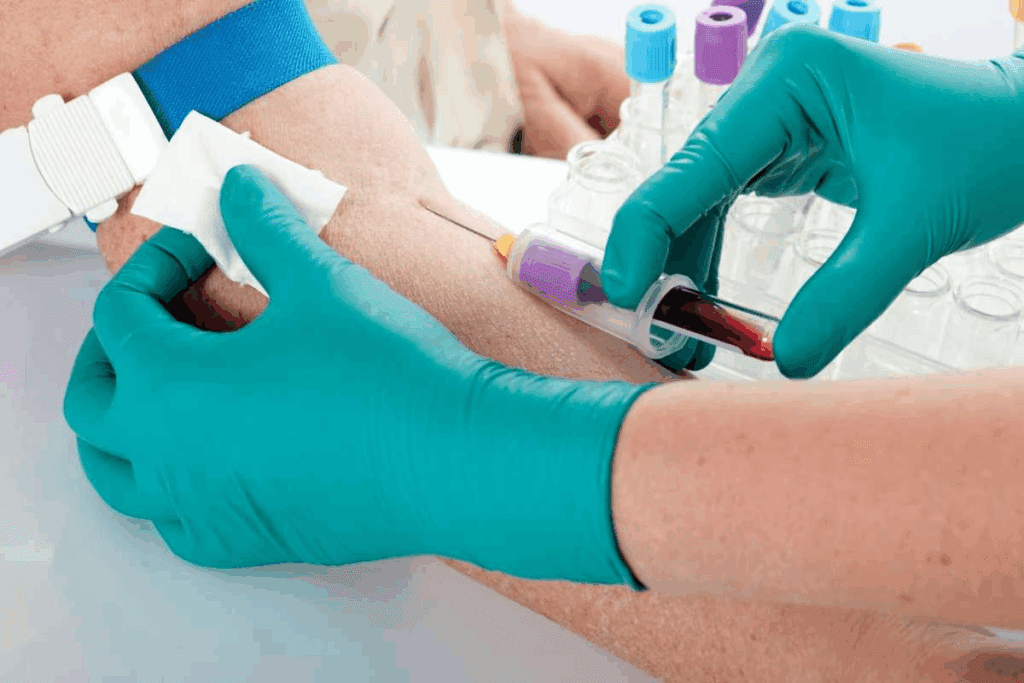
Getting an MPL blood test involves a few steps. First, you prepare, then your blood is taken, and lastly, it’s analyzed in a lab. Knowing these steps can make you feel more at ease and help the process go smoothly.
Patient Preparation
Before your MPL blood test, you need to get ready. You might be told to fast for a few hours before the test. But your doctor might give you different instructions. It’s also important to tell your doctor about any medicines you’re taking. Some can affect the test results.
Sample Collection Process
The blood test is done by taking a venipuncture. A healthcare professional will take blood from your arm. It’s quick and doesn’t hurt much. Then, the blood goes to a lab for testing.
What to Expect During Testing
Here’s what happens during the MPL blood test:
- A healthcare professional will clean the area around the vein with an antiseptic.
- A tourniquet may be applied to make the vein more accessible.
- The blood sample will be drawn into one or more tubes, depending on the required amount for the test.
- After the sample is collected, the needle is withdrawn, and pressure is applied to the puncture site to stop any bleeding.
The whole process takes just a few minutes. After it’s done, you can go back to your usual activities without any big changes.
Laboratory Methods for MPL Mutation Analysis
Laboratory tests for MPL mutations use advanced techniques. These methods help find specific genetic changes linked to myeloproliferative neoplasms (MPNs).
Finding MPL mutations is key to diagnosing, predicting outcomes, and planning treatments. Many lab methods exist to spot these mutations. Each has its own benefits and drawbacks.
PCR-Based Techniques
Polymerase Chain Reaction (PCR) is a common method for MPL mutation analysis. It amplifies DNA sequences to find mutations.
- Allele-Specific PCR: This method uses special primers to find mutant alleles, even in small amounts.
- Real-Time PCR: It measures how much mutant allele is present, helping track the disease.
PCR is very sensitive. It can find MPL mutations in a few cells, helping catch diseases early and track them.
Next-Generation Sequencing
Next-Generation Sequencing (NGS) has changed genetic analysis, including MPL mutation detection. NGS can look at many genes and mutations at once.
- Targeted NGS: Focuses on specific genes like MPL, giving detailed mutation info.
- Whole-Exome Sequencing: Sequences all protein-coding regions, finding more mutations related to MPNs.
NGS gives a full genetic picture. It helps with diagnosis, predicting outcomes, and tailoring treatments.
Other Detection Methods
Other methods for MPL mutation analysis include:
- Sanger Sequencing: A classic method that shows detailed sequences but is less good at finding low-level mutations.
- High-Resolution Melting Analysis: A sensitive method that uses DNA melting characteristics to find mutations.
These methods work together. The choice depends on the situation, the sample, and the lab’s skills.
Interpreting MPL Blood Test Results
Understanding MPL blood test results is key to diagnosing and managing myeloproliferative neoplasms. The test looks for mutations in the MPL gene, which can cause certain blood disorders. Knowing how to read these results means grasping the genetic changes and their effects on health.
Positive vs. Negative Results
A positive MPL blood test result means a mutation in the MPL gene has been found. This can point to diseases like essential thrombocythemia or primary myelofibrosis. But a negative result means no MPL mutation was found. It’s important to remember, though, that a negative result doesn’t mean a disease is ruled out, as other mutations could be present.
Knowing if an MPL mutation is present or not can change how a patient is treated. For example, those with a positive result might need more frequent check-ups and different treatments than those with a negative result.
Allele Burden Quantification
Allele burden quantification measures how many cells have the MPL mutation. This info helps doctors understand how severe the disease is and how well treatment is working. A higher allele burden might mean a more serious disease, possibly leading to a poorer outlook.
Tracking the allele burden over time is also important. Changes in this number can lead to changes in treatment plans. This ensures the treatment stays effective.
Clinical Correlation
Linking MPL blood test results with a patient’s overall health is vital for accurate diagnosis and treatment. Doctors must look at the test results alongside the patient’s symptoms, medical history, and other test findings.
By combining MPL blood test results with other diagnostic information, doctors get a clearer picture of the patient’s health. This helps them make treatment plans that are tailored to the patient’s needs.
MPL Mutations in Primary Myelofibrosis
Understanding MPL mutations is key to diagnosing and treating primary myelofibrosis. This disease causes bone marrow fibrosis, spleen enlargement, and a chance of turning into leukemia.
Prevalence and Significance
MPL mutations are found in some patients with primary myelofibrosis. Research shows these mutations occur in 5% to 15% of cases. They are linked to older age, anemia, and a higher risk of blood clots.
The role of MPL mutations is significant. They affect how the disease behaves and patient outcomes. MPL-mutated patients may have a different disease path than those with JAK2 or CALR mutations.
Disease Progression
MPL mutations can make primary myelofibrosis more aggressive. Patients with these mutations may see faster bone marrow fibrosis and a higher risk of leukemia.
Doctors watch MPL-mutated patients closely. They check blood counts, spleen size, and molecular markers regularly.
Prognostic Implications
MPL mutations have big implications for primary myelofibrosis prognosis. Studies link these mutations to worse outcomes, including shorter survival and faster disease progression.
Models like the Dynamic International Prognostic Scoring System (DIPSS) help predict outcomes. MPL mutations play a big role in these models. They help doctors make better treatment plans for patients.
MPL Mutations in Essential Thrombocythemia
MPL mutations are key genetic changes in essential thrombocythemia, a condition with too many platelets. This condition, known as ET, makes platelets grow too much. It’s a type of MPN.
Frequency and Clinical Features
About 3-5% of ET patients have MPL mutations. These mutations show up in older patients. They might have different blood counts than those with JAK2 or CALR mutations.
Having MPL mutations can change how ET shows up. For example, platelet counts might move differently. This could affect the risk of blood clots.
Thrombotic Risk Assessment
Assessing the risk of blood clots is key in ET. MPL mutations, along with age and past blood clots, shape a patient’s risk. This helps doctors plan care.
| Risk Factor | Description | Impact on Thrombotic Risk |
| MPL Mutation | Genetic mutation affecting the MPL gene | Increased risk |
| Age >60 | Older age at diagnosis | Increased risk |
| Previous Thrombosis | History of thrombotic events | Significantly increased risk |
Differential Diagnosis
Diagnosing ET means figuring out if it’s different from other blood disorders. Finding MPL mutations helps doctors make this distinction. Other genetic markers like JAK2 and CALR also play a role.
Getting the right diagnosis is vital. It helps doctors choose the best treatment. MPL mutations help doctors understand the risks and benefits of treatments.
Relationship Between MPL, JAK2, and CALR Mutations
Myeloproliferative neoplasms (MPNs) have mutations in important genes like MPL, JAK2, and CALR. These changes are key to how MPNs develop and show up in patients.
Mutational Landscape in MPNs
The genetic picture of MPNs is complex. MPL, JAK2, and CALR mutations are major players. The JAK2 V617F mutation is the most common, found in most polycythemia vera (PV) patients and many with essential thrombocythemia (ET) and primary myelofibrosis (PMF). CALR mutations are also common, mainly in ET and PMF. MPL mutations are less frequent but important too.
Mutual Exclusivity Patterns
Research shows that MPL, JAK2, and CALR mutations often don’t appear together. This suggests they might be working through similar molecular paths in the disease.
- MPL mutations are typically found in ET and PMF.
- JAK2 mutations are associated with PV, ET, and PMF.
- CALR mutations are more commonly seen in ET and PMF.
Combined Genetic Testing Approaches
Because of the complex genetics of MPNs, testing for MPL, JAK2, and CALR mutations together is becoming more common. This helps doctors understand the disease better in each patient.
| Gene | Mutation Frequency | Associated MPNs |
| MPL | Less common | ET, PMF |
| JAK2 | High | PV, ET, PMF |
| CALR | Moderate | ET, PMF |
Clinical Implications of MPL Mutation Testing
The MPL mutation test has a big impact on how we diagnose and treat diseases. It helps us pick the right treatment and keep an eye on how the disease is progressing. Knowing how it works is key for doctors.
Diagnostic Value
MPL mutation testing is very useful in finding MPNs, like primary myelofibrosis and essential thrombocythemia. It helps tell these diseases apart. This helps doctors know how to manage each case better.
Doctors use a mix of clinical checks, lab tests, and genetic tests, including MPL mutation testing. This detailed method makes diagnosis more accurate. It helps doctors plan the best treatment for each patient.
Treatment Selection
The results of MPL mutation testing are very important for choosing treatments. Patients with MPL mutations might need different treatments than those with JAK2 or CALR mutations. Knowing the mutation helps doctors tailor treatments to fit each patient’s needs.
Treatments might include JAK inhibitors, which work well for MPNs, no matter the mutation. But, having an MPL mutation might affect which other treatments are used or if they should join clinical trials.
Monitoring Disease Progression
MPL mutation testing is also key to watching how diseases progress. By testing regularly, doctors can see how the disease is changing. This helps them understand the risk of the disease getting worse.
Regular checks let doctors adjust treatments as needed. This ensures patients get the best care possible. It helps improve their health and quality of life.
Future Directions in MPL Mutation Research
The future of MPL mutation research is exciting. It promises to deepen our understanding of MPNs and better patient care. As we learn more about the genetics of these diseases, new ways to diagnose and treat them will emerge.
Advancements in Diagnostic Techniques
New testing methods for MPL mutations are on the horizon. These advancements will make diagnosis more accurate and earlier. This means better monitoring and care for MPN patients.
Some new technologies include:
- Next-generation sequencing (NGS) for detailed genetic profiles
- Digital PCR for exact counts of mutant genes
- Advanced bioinformatics tools for analyzing and understanding data
Exploring Therapeutic Targets
Research into therapeutic targets is vital. Scientists aim to find ways to intervene in the molecular pathways affected by MPL mutations. This could lead to new treatments.
| Therapeutic Target | Potential Benefit | Current Status |
| JAK-STAT pathway inhibitors | Less disease burden and fewer symptoms | Ongoing clinical trials |
| MPL receptor modulators | Stable platelet counts and lower risk of blood clots | Preclinical development |
| Epigenetic modifiers | Reversing disease progression | Early-stage research |
Personalized Medicine Approaches
Using personalized medicine in MPN treatment is a promising area. Tailoring treatments to a patient’s genetic makeup could lead to better outcomes. It could also reduce the risk of complications.
Future studies will likely focus on:
- Creating genetic risk models to guide treatment
- Studying how MPL mutations affect disease progression and treatment response
- Exploring combination therapies based on individual patient profiles
Conclusion
The MPL blood test is key in diagnosing myeloproliferative neoplasms (MPNs). It finds MPL mutations, helping doctors classify and treat MPNs like primary myelofibrosis and essential thrombocythemia.
Knowing about MPL mutations is essential for doctors to create good treatment plans. The MPL blood test, along with JAK2 and CALR tests, gives a full picture of MPN mutations. This helps in tailoring treatments to each patient.
The MPL blood test is important for making better treatment choices and improving patient care. As new research comes out, the MPL blood test will play an even bigger role in treating MPNs.
FAQ
What is the MPL gene, and what is its role in blood cell production?
The MPL gene makes the thrombopoietin receptor. It’s key in making blood cells, mainly in megakaryocytes.
What is the MPL blood test used for?
The MPL blood test finds MPL gene mutations. It helps diagnose and manage myeloproliferative neoplasms (MPNs) like primary myelofibrosis and essential thrombocythemia.
What are the different types of MPL gene mutations?
Most MPL gene mutations are somatic. They happen in body cells and aren’t passed down. These can cause MPNs.
How is the MPL blood test performed?
To do the MPL blood test, a blood sample is taken. It’s then analyzed in a lab using PCR or next-generation sequencing.
What does a positive MPL blood test result mean?
A positive result means an MPL gene mutation is found. This can raise the risk of MPNs or other blood issues.
Can MPL mutations be found in healthy individuals?
Yes, MPL mutations can be in healthy people, too. But their meaning is not fully understood yet.
How do MPL, JAK2, and CALR mutations relate to each other in MPNs?
MPL, JAK2, and CALR mutations are different genetic changes. They can lead to MPNs. Usually, only one mutation is found in a patient.
What is the significance of MPL mutations in primary myelofibrosis?
MPL mutations in primary myelofibrosis show specific traits. They might affect how the disease progresses and the patient’s outlook.
How do MPL mutations affect the risk of thrombosis in essential thrombocythemia?
MPL mutations in essential thrombocythemia can change the risk of blood clots. Finding these mutations helps in managing the risk.
What are the future directions in MPL mutation research?
Research will focus on better testing methods and finding new treatments. It aims to improve care for MPN patients.
What is the role of MPL mutation testing in clinical practice?
MPL mutation testing is key in diagnosing and managing MPNs. It helps doctors make treatment plans and track the disease.
Are there any other conditions associated with MPL gene mutations?
MPL mutations are mainly linked to MPNs. But studies are looking into their role in other blood disorders and conditions.
References
- Tiryaki, T. O., et al. (2025). CALR and MPL driver mutations and their role in the diagnosis of myeloproliferative neoplasms. Turkish Journal of Hematology, 42(2), 101-109. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12194900/