Last Updated on November 25, 2025 by

Prostatectomy, or prostate removal surgery, is a procedure to remove part or all of the prostate gland. The prostate gland is key to the male reproductive system. It’s located below the bladder and around the urethra. Find out if prostate surgery is a minor surgery, explore the procedure, risks, and recovery details for prostate surgery.
This surgical procedure helps treat prostate issues like prostate cancer and benign prostatic hyperplasia (BPH).
Patients should understand what prostate surgery involves. They need to understand the good and bad sides of this treatment.
Key Takeaways
- Prostatectomy involves removing part or all of the prostate gland.
- It’s used to treat prostate cancer, BPH, and other prostate issues.
- The procedure is significant and requires careful consideration.
- Patients should understand the implications and benefits of prostate surgery.
- Prostate removal surgery is a treatment option as per medical guidelines.
Understanding the Prostate Gland and Its Function
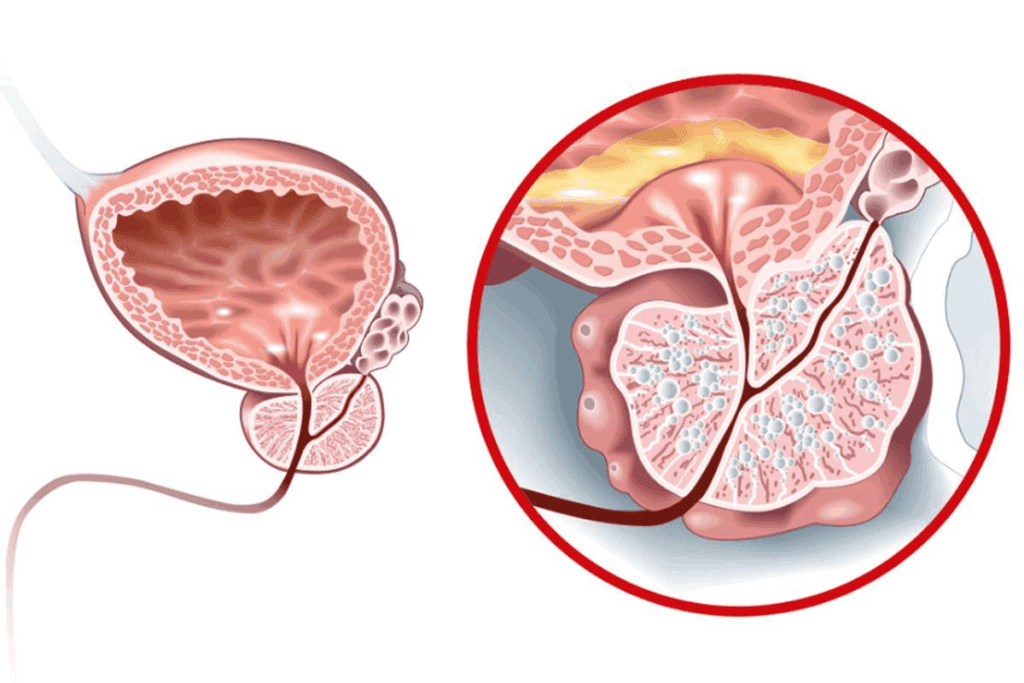
The prostate gland is key to the male reproductive system, sitting around the urethra. It’s like a walnut in size, between the bladder and penis. Its main job is to make seminal fluid, which feeds and guards sperm during ejaculation.
Anatomy and Location of the Prostate
The prostate gland is in the pelvis, below the bladder and in front of the rectum. It wraps around the urethra, the tube that carries urine from the bladder to the penis. As men age, the prostate can grow and change shape, often becoming walnut-sized in young men.
Physiological Role in Male Reproductive Health

The prostate gland mainly makes prostatic fluid, a big part of semen. This fluid gives sperm nutrients and protection, helping them move better. It also helps control urine flow, as it’s around the urethra.
Common Problems Affecting the Prostate
Many issues can hit the prostate gland, like prostate cancer, Benign Prostatic Hyperplasia (BPH), and prostatitis. These problems can lead to symptoms like trouble urinating, painful pee, and trouble getting an erection.
| Condition | Description | Common Symptoms |
| Prostate Cancer | Malignant tumor in the prostate gland | Difficulty urinating, blood in urine or semen |
| Benign Prostatic Hyperplasia (BPH) | Non-cancerous enlargement of the prostate | Frequent urination, weak urine flow |
| Prostatitis | Inflammation of the prostate gland | Painful urination, fever, painful ejaculation |
Knowing about the prostate gland is important for men to keep an eye on their reproductive health. If they notice any symptoms, they should see a doctor right away.
Is Prostate Surgery Considered a Minor Surgery?
Whether prostate surgery is minor or major depends on several things. These include the type of surgery, the health issue being treated, and the patient’s overall health.
Prostate surgery can vary from simple to very complex.
Classification of Prostate Procedures
Prostate procedures fall into a few main categories. These are:
- Diagnostic procedures
- Therapeutic procedures
- Palliative procedures
Each type has its own level of complexity and risks.
Factors That Determine Surgical Complexity
Several things make prostate surgery complex. These include:
| Factor | Description |
| Patient’s overall health | Pre-existing medical conditions can affect surgical complexity |
| Type of procedure | Different procedures have varying levels of complexity |
| Surgeon’s experience | A skilled surgeon can reduce the complexity of the procedure |
Comparison to Other Urological Procedures
Prostate surgery is just one of many urological procedures. Compared to others, prostate surgery is considered complex. This is because of the delicate nature of the prostate gland and surrounding tissues.
“The complexity of prostate surgery is often compared to other urological surgeries such as nephrectomy or cystectomy.”
Understanding how complex prostate surgery is helps patients prepare. It also helps them understand what to expect from the procedure.
Common Conditions Requiring Prostate Surgery
The prostate gland can face many issues that might need surgery. Surgery is a big step taken when other treatments don’t work. It’s for health problems related to the prostate.
Prostate Cancer
Prostate cancer is a common reason for surgery. It happens when prostate cells grow too much. At first, it might not show symptoms. But as it gets worse, you might have trouble peeing, painful pee, or see blood in your pee or semen.
Treatment for prostate cancer depends on how far it has spread and your health. Doctors might choose surgery, radiation, or watchful waiting. Removing the prostate gland and nearby tissues is one surgery option.
Benign Prostatic Hyperplasia (BPH)
BPH is another reason for surgery. It’s when the prostate gets too big and blocks urine flow. Symptoms include needing to pee a lot, weak pee, and waking up to pee a lot at night.
Doctors use your medical history, physical check-ups, and tests like uroflowmetry to diagnose BPH. Treatment options include medicines or surgery like TURP or simple prostatectomy.
Other Prostate Conditions
Prostatitis and prostate stones are other issues that might need surgery. Prostatitis causes pain, trouble peeing, and sex problems. Prostate stones can hurt and make peeing hard.
Doctors figure out these conditions with exams, imaging, and lab tests. Treatment varies based on the cause and how bad the symptoms are. It might include antibiotics, meds, or surgery.
Types of Prostate Surgery Procedures
Prostate surgery isn’t the same for everyone. Different methods are used to treat different problems. The right surgery depends on the patient’s health, the condition, and the doctor’s advice.
Radical Prostatectomy
Radical prostatectomy removes the prostate gland and some nearby tissue. It’s often chosen for prostate cancer that hasn’t spread. Radical prostatectomy can be done in several ways, like open surgery, laparoscopic, or robotic-assisted.
Simple Prostatectomy
Simple prostatectomy treats benign prostatic hyperplasia (BPH). BPH makes the prostate grow, blocking urine. This surgery removes part of the prostate to fix the problem.
Transurethral Resection of the Prostate (TURP)
TURP is a small surgery for BPH. It removes tissue that blocks urine. TURP is very effective in solving urinary issues from an enlarged prostate.
Laser Prostatectomy
Laser prostatectomy is a small surgery for BPH too. It uses a laser to remove tissue. Laser prostatectomy has less bleeding and shorter stays than TURP.
Each surgery has its own reasons, benefits, and risks. Knowing the differences helps patients choose the best treatment.
Surgical Approaches for Prostate Removal
Surgeons use different methods to remove the prostate. The choice depends on the patient’s health, cancer stage, and the surgeon’s skill.
Open Surgery Techniques
Open surgery, or prostatectomy, involves a single incision in the abdomen or perineum. It allows for direct removal of the prostate. It’s often used for larger prostates or when more tissue needs to be removed. While recovery may take longer, new surgical methods have improved results.
Laparoscopic Radical Prostatectomy
Laparoscopic radical prostatectomy is a minimally invasive method. It uses small incisions for instruments and a camera. This approach leads to less blood loss and quicker recovery. It’s great for nerve-sparing surgery, allowing for precise nerve dissection.
Robotic-Assisted Prostatectomy
Robotic-assisted prostatectomy uses a robotic system for enhanced surgery. It offers high-definition 3D vision, precise tools, and better dexterity. It’s popular for its reduced complications, less blood loss, and faster recovery.
The choice between these methods depends on the patient’s condition, the surgeon’s experience, and the prostate’s characteristics. Each method has its benefits and drawbacks. Patients should talk to their healthcare provider to choose the best option for them.
Patients should understand what prostate surgery involves.
Getting ready for prostate surgery involves many steps. You’ll need medical checks, lifestyle changes, and mental prep. It’s all about setting up for a good surgery and easy recovery.
Medical Evaluations and Tests
Before surgery, you’ll have to go through several medical tests. These tests check your health and find any risks for the surgery.
- Blood Tests: To check for infections, blood cell count, and overall health.
- Imaging Tests: Such as MRI or CT scans to assess the prostate and surrounding tissues.
- Cardiac Evaluation: For patients with heart conditions, to assess their heart health.
Medication Adjustments
You might need to change your meds before surgery. Some meds, like blood thinners, could increase bleeding risks.
- Inform your doctor about all medications you are currently taking.
- Follow the doctor’s instructions regarding medication adjustments.
Dietary and Lifestyle Preparations
Changing your diet and lifestyle can help a lot. Eating well and living healthy can make recovery easier.
- Nutritional Counseling: To ensure you are getting the necessary nutrients.
- Hydration: Drinking plenty of water to stay hydrated.
- Avoiding smoking and alcohol in the period leading up to surgery.
Mental Preparation
Mental prep is as key as physical prep. You should be ready for the emotional and psychological sides of surgery.
Counseling or support groups can offer emotional support. Knowing what to expect can also reduce anxiety.
Patients should understand what prostate surgery involves.
Choosing the right anesthesia for prostate surgery is key to a successful procedure. There are many options, each with its own benefits and risks.
General Anesthesia
General anesthesia is a popular choice for prostate surgery. It makes the patient unconscious and pain-free during the surgery. It’s given through a mix of intravenous and inhaled anesthetics.
Benefits of General Anesthesia:
- Ensures patient comfort during surgery
- Allows for controlled ventilation
- Can be adjusted according to the patient’s response
Spinal or Epidural Anesthesia
Spinal or epidural anesthesia numbs the lower body by injecting medication near the spinal cord. It’s a good alternative to general anesthesia for some patients.
“Regional anesthesia, including spinal and epidural anesthesia, can provide excellent pain relief and reduce the need for systemic opioids,”
Advantages of Spinal or Epidural Anesthesia:
- Reduced risk of respiratory complications
- Less postoperative nausea and vomiting
- Effective pain management
Use of Supraglottic Airways
Supraglottic airways help with ventilation during general anesthesia. They’re used when endotracheal intubation isn’t needed or wanted.
| Device Type | Description | Advantages |
| Laryngeal Mask Airway (LMA) | A device that sits over the laryngeal inlet | Less invasive, easier to insert than endotracheal tube |
| Other Supraglottic Airways | Various designs available, each with unique features | Provides a secure airway, reduces risk of aspiration |
Anesthesia Risks and Considerations
Anesthesia is generally safe, but there are risks. These include respiratory problems, allergic reactions, and nerve damage.
It’s important to understand these risks and talk to an anesthesiologist. This helps ensure patient safety and informed decision-making.
The Prostate Surgery Procedure in Detail
Patients should understand what prostate surgery involves.
Duration of Different Procedures
The time needed for prostate surgery changes based on the procedure. A simple surgery might be quicker than a more complex one. This includes removing the prostate gland and nearby tissues.
Here’s a quick look at how long different surgeries take:
| Procedure | Typical Duration |
| Simple Prostatectomy | 1-2 hours |
| Radical Prostatectomy | 2-4 hours |
| Transurethral Resection of the Prostate (TURP) | 1-3 hours |
Step-by-Step Surgical Process
The surgery starts with preparing the patient. This includes giving anesthesia. Then, the surgical team does the chosen procedure.
Key steps in the surgical process include:
- Incision and access to the prostate gland
- Removal or resection of the prostate tissue
- Suturing or cauterizing to control bleeding
- Closure of the incision
Technological Advancements
New technology has made prostate surgery better. Robotic-assisted surgery is more precise and less invasive. Also, new imaging helps plan and do the surgery.
What Happens in the Operating Room
In the operating room, a team works together. The surgeon, anesthesiologist, and nurses watch the patient’s health. They handle any problems during the surgery.
Advanced tools, like robotic systems, help with the surgery. They make the process more precise and controlled.
Immediate Post-Operative Care
Patients who have prostate surgery need careful care right after to avoid problems and help them heal well.
Hospital Stay Duration
The time a patient stays in the hospital after prostate surgery can change. It depends on the surgery type and the patient’s health. Patients with less invasive surgeries might stay less than those with open surgery.
Most patients stay 1 to 3 days, but it can be longer if there are issues. Doctors watch the patient closely, manage pain, and look for any problems.
Pain Management Strategies
Managing pain well is key after surgery. Patients get pain meds to help with discomfort.
The kind and amount of pain meds vary based on the patient’s pain and health history. It’s important to take pain meds as told by the doctor to avoid bad side effects.
Catheter Management
A urinary catheter is often used after prostate surgery to help with urine. Catheter management means keeping it clean and watching for infection or blockage signs.
Patients get instructions on catheter care at home. It’s important to follow these steps carefully to avoid problems.
Initial Activity Restrictions
After surgery, patients should not do too much to help their body heal. This means avoiding heavy lifting, bending, or hard exercise.
Slowly starting to do more as the doctor says can help in getting better. Patients should also know when to seek medical help for complications.
Prostate Surgery Recovery Timeline
Recovering from prostate surgery takes time and involves different stages. Each stage has its own challenges and milestones. Knowing about these stages helps manage expectations and get the best results.
Short-term Recovery (First Few Weeks)
The first few weeks after surgery are tough. Patients might feel pain, be tired, and have trouble with their urine. Pain management is key, and doctors often give medicine to help with pain.
It’s important to avoid heavy lifting, bending, and hard work to avoid problems. Regular check-ups with doctors are also vital to track healing and solve any issues.
Medium-term Recovery (1-3 Months)
As patients move into the next phase, they start to feel better. Urinary control might take time to get back, but exercises like Kegels help.
Doctors slowly let patients do more things, like driving and light exercise. But, always listen to the doctor about how much to do.
Long-term Recovery (Beyond 3 Months)
By the long-term phase, most patients have made a lot of progress. They see big improvements in their urine and sex life. Regular check-ups with doctors are key to catch any new problems.
Return to Normal Activities
How long it takes to get back to normal varies. It depends on the surgery type, health, and following doctor’s orders. Here’s a table showing the general recovery timeline:
| Recovery Phase | Typical Duration | Common Experiences |
| Short-term | First few weeks | Discomfort, fatigue, urinary issues |
| Medium-term | 1-3 months | Improving urinary control, gradual return to activities |
| Long-term | Beyond 3 months | Continued improvement in urinary and sexual function |
Knowing the prostate surgery recovery timeline helps patients prepare. It makes the journey back to normal life smoother.
Potential Complications and Risks of Prostatectomy
Patients should understand what prostate surgery involves.my. This surgery, like any major surgery, can have risks and complications. These can vary in how serious they are.
Common Side Effects
Prostatectomy can cause urinary incontinence and erectile dysfunction. These issues can be tough, but there are ways to manage them.
Some people might have urinary incontinence, which can be mild or severe. Erectile dysfunction can also happen due to nerve damage around the prostate.
Serious Complications
Though rare, serious problems can happen. These include infections, blood clots, and damage to nearby organs.
- Infection: Surgery can lead to infection.
- Blood Clots: There’s a risk of blood clots, which can be dangerous.
- Damage to Surrounding Organs: The prostate is close to other important parts, so there’s a risk of damage during surgery.
Risk Factors for Complications
Some things can make complications more likely. These include the patient’s health, age, and other medical conditions.
| Risk Factor | Description | Impact on Complications |
| Age | Older patients may have more health issues. | Increased risk of complications |
| Overall Health | Conditions like diabetes or heart disease. | Higher risk of complications |
| Obesity | Being significantly overweight. | Increased risk of infection and other complications |
Managing and Minimizing Risks
Reducing risks involves preparation, skilled surgery, and care after surgery.
Patients can lower their risk by following pre-surgery instructions. This includes stopping certain medications and getting ready for surgery.
After surgery, following the surgeon’s advice is key. This includes managing pain, staying active, and attending follow-up appointments.
Life After Prostate Removal
Men who have their prostate removed may see big changes in their health. This surgery is often done for prostate cancer or BPH. It can change a man’s life a lot.
Physiological Changes
Without the prostate, men might have trouble controlling their urine. They could also face issues with their sex life, like not being able to get an erection.
Sexual Function and Fertility
Prostate removal can hurt a man’s sex life. Many men struggle with erectile dysfunction because of nerve damage. How much this affects a man depends on the surgery and his health before it.
Also, this surgery can make it harder to have kids. Men who want to have children might want to save their sperm before surgery.
Urinary Control Challenges
Many men have trouble controlling their urine after surgery. They might leak urine when they cough or sneeze. Doing Kegel exercises can help with this.
For some, this problem doesn’t go away. They might need more help or use special products to manage it.
Can You Live Without a Prostate?
Yes, men can live without a prostate. Even though it’s important for health, losing it doesn’t mean the end. Many men stay healthy and active after surgery, making some changes to deal with side effects.
Knowing what to expect and talking to your doctor can make a big difference. It helps men live better after surgery.
Patients should understand what prostate surgery involves.
Patients often look for non-surgical options for prostate problems. They want treatments that are less invasive and fit their needs better. Luckily, there are many alternatives, each with its own benefits and things to consider.
Medication Options
Medication is a common choice instead of surgery. Alpha-blockers and 5-alpha-reductase inhibitors help manage symptoms of an enlarged prostate. They relax muscles or shrink the prostate to improve urine flow.
It’s important to talk about side effects with a doctor. Alpha-blockers can cause dizziness or affect ejaculation. 5-alpha-reductase inhibitors might lower libido or cause erectile dysfunction.
Minimally Invasive Procedures
Minimally invasive procedures are another option. Transurethral Microwave Therapy (TUMT) and Transurethral Needle Ablation (TUNA) use heat or radiofrequency to shrink the prostate. This helps with urinary symptoms.
These procedures are done on an outpatient basis and have a quick recovery. But, they might not work for everyone, and their success can vary.
Watchful Waiting Approach
For mild symptoms or those not good for surgery, watchful waiting is suggested. It means regular check-ups and tests to see if symptoms get worse or if new problems come up.
This method is for slow-growing prostate cancer or BPH with mild symptoms. Lifestyle changes and medications can help manage symptoms along with watchful waiting.
Radiation Therapy Options
Radiation therapy is a treatment for prostate cancer. It uses high-energy rays to kill or slow cancer cells. There are external beam radiation therapy (EBRT) and brachytherapy, where seeds are implanted in the prostate.
Radiation therapy can be effective, but it’s important to talk about risks and side effects. These can include urinary and bowel problems, and erectile dysfunction.
Making an Informed Decision About Prostate Surgery
Choosing prostate surgery needs careful thought. You must know your options, the risks, and the benefits.
Questions to Ask Your Surgeon
Asking the right questions is key. Find out about the surgeon’s experience, the expected outcomes, and complications. Important questions include:
- What are the reasons for recommending prostate surgery?
- What are the alternatives to surgery, and how do they compare?
- What are the possible risks and complications of the surgery?
- How will the surgery affect my quality of life and urinary or sexual function?
- What is the expected recovery time, and what kind of support will I need?
Getting Second Opinions
Getting a second opinion is wise. It can give more insights and help confirm or challenge the initial plan. It’s okay to ask for another opinion. It can offer reassurance and reveal other treatment options.
Weighing Benefits Against Risks
It’s important to weigh the benefits against the risks of prostate surgery. Benefits include removing cancer or easing symptoms. But, there are risks like incontinence and erectile dysfunction. Talk about these with your healthcare provider.
Support Resources for Patients
Patients can find help through support resources. These include support groups, counseling, and educational materials. A strong support system can greatly help in recovery and overall well-being.
By asking the right questions, getting second opinions, weighing the pros and cons, and using support resources, patients can make a well-informed choice about prostate surgery.
Conclusion
Prostate surgery is a big decision that needs careful thought. It’s often needed for prostate cancer or BPH. These conditions can make surgery a necessary choice.
A prostatectomy summary shows the different surgeries. These include radical prostatectomy, simple prostatectomy, and TURP. Each has its own reasons, benefits, and risks.
Patients should understand what prostate surgery involves.
In short, prostate surgery is a complex topic. By learning about it, people can make better choices. This helps them find the right treatment for their health needs, leading to a good prostate surgery conclusion.
FAQ
What is prostate surgery?
Prostate surgery, also known as prostatectomy, is a procedure to remove part or all of the prostate gland.
What is the prostate gland, and what is its function?
The prostate gland is a key part of the male reproductive system. It’s located below the bladder and surrounds the urethra. It’s vital for male reproductive health.
Is prostate surgery a minor surgery?
Prostate surgery can be minor or major. It depends on the procedure and the individual’s situation.
What are the common conditions that require prostate surgery?
Prostate surgery treats conditions like prostate cancer, benign prostatic hyperplasia (BPH), and other issues.
What are the different types of prostate surgery procedures?
There are several types, including radical prostatectomy, simple prostatectomy, transurethral resection of the prostate (TURP), and laser prostatectomy.
How is prostate surgery performed?
Surgery can be done through open surgery, laparoscopic radical prostatectomy, or robotic-assisted prostatectomy.
What are the benefits and risks of prostate surgery?
Surgery can treat prostate cancer and BPH symptoms. But, it may cause urinary incontinence and erectile dysfunction.
How long does prostate surgery take?
Surgery time varies. It can be a few hours for simple procedures or several hours for complex ones.
What is the recovery time for prostate surgery?
Recovery time varies. Patients usually return to normal activities in weeks to months.
Can you live without a prostate?
Yes, living without a prostate is possible. But, it may cause urinary incontinence and erectile dysfunction.
Are there alternative treatments to prostate surgery?
Yes, alternatives include medication, minimally invasive procedures, watchful waiting, and radiation therapy.
How do I make an informed decision about prostate surgery?
Discuss your options with your surgeon. Consider second opinions and weigh the benefits and risks. Use support resources too.
What are the possible complications and risks of prostatectomy?
Risks include common side effects and serious complications. Proper care can manage and minimize these risks.
What happens during the immediate post-operative care after prostate surgery?
Post-operative care includes hospital stay, pain management, catheter management, and activity restrictions. These ensure a smooth recovery.
How is anesthesia used during prostate surgery?
Anesthesia options include general anesthesia, spinal or epidural anesthesia, and supraglottic airways. Each has its benefits and risks.
Reference
- McVary, K. T. (2008). BPH and Prostate Cancer: Surgical Options and Outcomes. The Journal of Urology, 179(3), S131–S137. https://pubmed.ncbi.nlm.nih.gov/18249545/





