Last Updated on November 27, 2025 by Bilal Hasdemir
At Liv Hospital, we know how complex B cell lymphoma is. It’s a group of cancers that make up about 85% of non-Hodgkin lymphomas worldwide. Knowing the different types is key for finding the right treatment.
We focus on spotting the many types of B cell lymphomas. This includes diffuse large B-cell lymphoma (DLBCL), a common and aggressive one. Getting the right diagnosis and treatment is vital for good care.
Key Takeaways
- B cell lymphomas represent a diverse group of malignancies.
- They account for approximately 85% of all non-Hodgkin lymphomas.
- Understanding the types of B cell lymphomas is key for diagnosis and treatment.
- DLBCL is a common and aggressive form of B cell lymphoma.
- Accurate diagnosis and tailored treatment plans are essential for effective care.
The Biology and Classification of Cancer B Cell Lymphoma
Malignant B cell lymphoma comes from B lymphocytes at different stages. This leads to various symptoms. Knowing how these cancers work is key for the right diagnosis and treatment.
B Cell Development and Lymphomagenesis
B cell development is complex. It involves B lymphocytes maturing in the bone marrow and getting activated in lymphoid tissues. Lymphomagenesis happens when genetic changes mess up B cell development. This causes malignant B cells to grow and live too long.
Many things can cause lymphomagenesis. These include genetic mutations, environmental factors, and immune system problems. For example, some genetic changes can make oncogenes work too much. This can lead to B cell lymphoma.
“The development of lymphoma is a multifactorial process, involving genetic, environmental, and immune system components.”
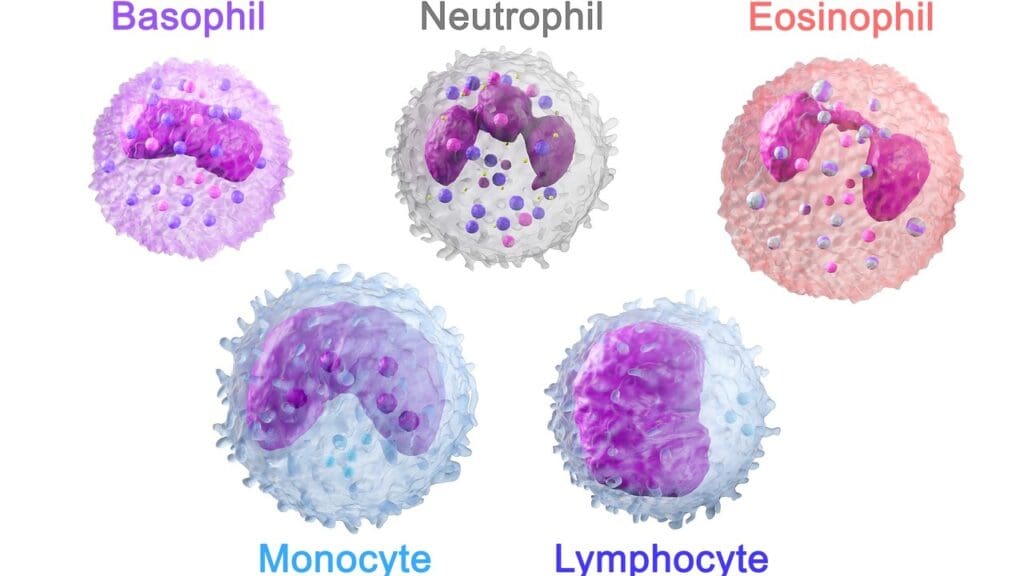
Diagnostic Biomarkers: CD19, CD20, and CD79a
Diagnostic biomarkers are vital for finding B cell lymphomas. CD19, CD20, and CD79a are important. They are found on B cells at different stages.
| Biomarker | Expression Pattern | Diagnostic Utility |
|---|---|---|
| CD19 | Expressed from early B cell development until plasma cell differentiation | Useful for identifying B cell malignancies |
| CD20 | Expressed on the surface of B cells from pre-B cell stage until maturity | Commonly used for diagnosing and treating B cell lymphomas |
| CD79a | Part of the B cell receptor complex, expressed throughout B cell development | Helpful in diagnosing B cell lymphomas, when other markers are absent |
These biomarkers help doctors accurately diagnose and classify B cell lymphomas. They guide treatment choices and predict outcomes.
Global Prevalence and Epidemiology
B cell lymphomas are a big health problem worldwide. They affect people differently in different places. Age, gender, and where you live can change how common they are.
Some B cell lymphomas are more common in certain groups. This shows we need specific health plans and research for each group.
Understanding B cell lymphoma worldwide is key. It helps us improve how we diagnose, treat, and care for patients everywhere.
Diffuse Large B-Cell Lymphoma (DLBCL)
Diffuse Large B-Cell Lymphoma (DLBCL) is a complex group of lymphomas. They need precise diagnosis and treatment plans. As the most common B cell NHL lymphoma, DLBCL has different clinical and molecular types. It’s important for doctors to know the latest in diagnosis and treatment.
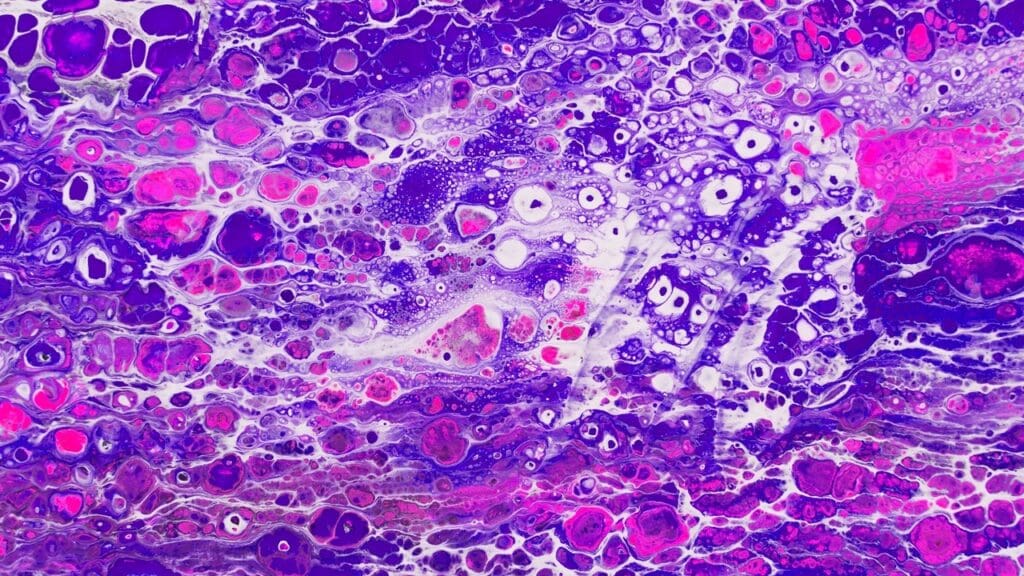
Clinical Presentation and Diagnostic Features
DLBCL often shows up with fast-growing lymph nodes and symptoms like fever, night sweats, and weight loss. Doctors diagnose it by looking at tissue samples. They look for large lymphoid cells with big nucleoli.
Immunophenotyping is key to confirm the diagnosis. It shows the presence of B cell markers like CD19, CD20, and CD79a.
Molecular Subtypes: GCB vs. ABC
DLBCL has two main molecular subtypes: Germinal Center B-cell-like (GCB) and Activated B-cell-like (ABC). GCB DLBCL usually has a better outlook than ABC DLBCL, which is more aggressive. Knowing these subtypes helps in planning treatment.
Double-Hit and Triple-Hit DLBCL
A part of DLBCL has MYC rearrangements with BCL2 and/or BCL6 translocations. These are known as double-hit or triple-hit lymphomas. They have a very poor outlook and need strong treatments. Finding these genetic changes is key to choosing the right treatment.
Treatment Approaches and Prognosis
The usual first treatment for DLBCL is R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone). But, the outlook varies a lot based on the molecular subtype, genetic changes, and patient factors. New treatments like CAR-T cell therapy are showing promise for those with relapsed or refractory DLBCL.
| DLBCL Subtype | Characteristic Features | Treatment Approach |
|---|---|---|
| GCB DLBCL | Better prognosis, germinal center origin | R-CHOP |
| ABC DLBCL | Aggressive clinical course, activated B-cell origin | R-CHOP, potentially intensified regimens |
| Double/Triple-Hit DLBCL | MYC, BCL2, and/or BCL6 rearrangements, poor prognosis | Intensive chemotherapy regimens, CAR-T cell therapy |
Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma (CLL/SLL)
Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma is a type of slow-growing B cell lymphoma. It affects B cells, causing various symptoms that need careful management.
Distinguishing Features and Diagnostic Criteria
CLL/SLL is known for its slow growth and specific markers. Doctors diagnose it by looking for CD5+, CD19+, CD20+, and CD23+ cells in blood or lymph nodes. Flow cytometry helps find these markers.
The disease may cause swollen lymph nodes, spleen, or high white blood cell count. Doctors use a mix of clinical checks, lab tests, and sometimes bone marrow biopsies to confirm it.
Prognostic Markers and Risk Stratification
Doctors use several markers to predict how CLL/SLL will progress. These include IGHV mutation status, CD38 expression, ZAP-70 expression, and genetic changes like del(17p) or del(11q). These help decide the best treatment.
The Rai and Binet systems help gauge how far the disease has spread and predict outcomes. Knowing these factors helps tailor treatment plans for each patient.
Richter’s Transformation and Disease Progression
A big risk in CLL/SLL is Richter’s transformation into a more aggressive lymphoma, like diffuse large B-cell lymphoma. This change is serious and needs quick, strong treatment.
It’s important to watch for signs of the disease getting worse or changing. Regular check-ups with a healthcare provider are key to managing CLL/SLL well.
Follicular Lymphoma
Follicular lymphoma is a common type of non-Hodgkin lymphoma. It is known for being slow-growing and having specific genetic traits. We will look into its grading, genetic features, and how it is managed.
Histological Grading and Clinical Implications
The grading of follicular lymphoma is key for predicting its course and treatment. It is based on the number of certain cells in a high-power field.
Grades 1-2 are low-grade, and grade 3 is split into 3A and 3B. Grade 3B is more aggressive. Knowing the grade helps doctors plan the best treatment.
Genetic Hallmarks: t(14;18) Translocation
Follicular lymphoma is marked by the t(14;18) translocation. This leads to too much BCL2 protein. Most cases have this genetic change, which helps the cancer cells live longer.
Management Strategies: From Observation to Targeted Therapy
Managing follicular lymphoma depends on the patient’s condition. Some get watchful waiting, while others get targeted treatments like rituximab, a CD20 antibody.
New discoveries in the disease’s biology have brought new treatments. These include cell therapy and other targeted drugs.
Mantle Cell Lymphoma
Cyclin D1 overexpression is a key feature of Mantle Cell Lymphoma. This B cell lymphoma has a unique pathophysiology and clinical presentation.
Cyclin D1 Overexpression and Pathogenesis
The t(11;14)(q13;q32) translocation causes cyclin D1 overexpression. This protein drives cell cycle progression. It’s central to Mantle Cell Lymphoma’s pathogenesis, leading to uncontrolled lymphoma cell growth.
Cyclin D1 dysregulation affects lymphomagenesis and disease behavior. Understanding its molecular mechanisms is key for targeted therapies.
Indolent vs. Aggressive Variants
Mantle Cell Lymphoma can be indolent or aggressive. The indolent form progresses slowly, while the aggressive form progresses quickly and has a worse prognosis.
We distinguish these variants by clinical features like the proliferation index (Ki-67) and secondary genetic alterations. Knowing the type is vital for choosing the right treatment.
| Clinical Features | Indolent MCL | Aggressive MCL |
|---|---|---|
| Proliferation Index (Ki-67) | Low | High |
| Disease Progression | Gradual | Rapid |
| Treatment Approach | Watchful waiting or less intensive therapy | Aggressive chemotherapy regimens |
Novel Therapeutic Approaches
The treatment for Mantle Cell Lymphoma is evolving. Targeted therapies like ibrutinib, a Bruton’s tyrosine kinase inhibitor, have shown great promise. They improve outcomes for MCL patients.
We’re also exploring PI3K inhibitors and immunotherapies like CAR-T cell therapy. These new treatments offer hope for better disease control and longer remissions.
Marginal Zone Lymphoma
Marginal Zone Lymphoma is a type of slow-growing B cell lymphoma. It starts in the area around germinal centers. These lymphomas have unique features and can show up in different ways.
MALT, Nodal, and Splenic Subtypes
There are several types of Marginal Zone Lymphoma. These include MALT, Nodal, and Splenic Marginal Zone Lymphoma. Each type has its own signs and symptoms.
- MALT Lymphoma: Linked to long-term infections, like Helicobacter pylori in the stomach.
- Nodal Marginal Zone Lymphoma: Mainly found in lymph nodes, with widespread disease.
- Splenic Marginal Zone Lymphoma: Shows up in the spleen, often with bone marrow involvement.
Infectious Triggers and Pathogenesis
The cause of Marginal Zone Lymphoma is tied to long-term infections and autoimmune diseases. For example, Helicobacter pylori is a known cause of gastric MALT lymphoma. Knowing these causes helps us find better treatments.
Removing the infection can sometimes make the lymphoma go away. This shows how infections, immune responses, and cancer are connected.
Treatment Paradigms
Treatment for Marginal Zone Lymphoma depends on the type, stage, and situation. For MALT lymphoma in one area, getting rid of H. pylori might be enough. But for more widespread disease, treatments like immunotherapy or chemotherapy might be needed.
- For MALT lymphoma, antibiotics are often the first step.
- Nodal and Splenic Marginal Zone Lymphomas might need stronger treatments, like rituximab-based regimens.
We’re always learning more about Marginal Zone Lymphoma. This helps us give our patients the best care, improving their lives and outcomes.
Burkitt Lymphoma
Burkitt lymphoma is a rare and aggressive B cell NHL. It needs quick diagnosis and treatment because it grows fast. This lymphoma has a high cell division rate, often showing bulky disease and a high risk of affecting the central nervous system.
MYC Translocation and Rapid Proliferation
The main genetic feature of Burkitt lymphoma is the MYC gene translocation on chromosome 8. This leads to too much MYC protein, causing the lymphoma to grow quickly and aggressively.
Rapid cell division is a key trait of Burkitt lymphoma. Almost all cells are in the cell cycle. This fast growth makes the tumor very aggressive and needs immediate treatment.
Endemic, Sporadic, and Immunodeficiency-Associated Forms
Burkitt lymphoma comes in three forms: endemic, sporadic, and immunodeficiency-associated. The endemic form is common in equatorial Africa and is linked to Epstein-Barr virus (EBV). The sporadic form is found worldwide, and the immunodeficiency-associated form affects people with HIV/AIDS or those on immunosuppressive therapy.
Each form has its own unique characteristics but all are aggressive and need intense treatment.
Intensive Chemotherapy Regimens and Outcomes
Treatment for Burkitt lymphoma includes strong chemotherapy, often with rituximab, a monoclonal antibody targeting CD20. These treatments aim to quickly reduce tumor size and prevent central nervous system involvement.
Thanks to modern chemotherapy, Burkitt lymphoma patients have better outcomes. High cure rates are seen in both children and adults. But, the treatment can be very toxic, so careful management and supportive care are essential.
Lymphoplasmacytic Lymphoma and Waldenström Macroglobulinemia
Lymphoplasmacytic lymphoma is a rare B cell lymphoma often linked to Waldenström macroglobulinemia. This connection helps us understand the disease’s biology and symptoms.
MYD88 Mutation and Disease Biology
The MYD88 mutation is key in lymphoplasmacytic lymphoma’s development. It activates pathways that help cells grow and live longer. Knowing how MYD88 works is vital for new treatments.
MYD88 is important in the toll-like receptor signaling pathway. Most Waldenström macroglobulinemia patients have MYD88 mutations. This shows its role in diagnosing and treating the disease.
Hyperviscosity Syndrome and Clinical Manifestations
Hyperviscosity syndrome is a key symptom of Waldenström macroglobulinemia. It’s caused by high IgM antibodies in the blood. Symptoms include tiredness, weakness, and neurological issues. It’s important to manage this condition quickly to avoid serious problems.
Patients with lymphoplasmacytic lymphoma and Waldenström macroglobulinemia show different symptoms. Some have swollen lymph nodes, spleen, or anemia. Others might not show symptoms for a long time.
Therapeutic Options and Response Assessment
Treatment for lymphoplasmacytic lymphoma and Waldenström macroglobulinemia has improved with new therapies. Ibrutinib, a BTK inhibitor, has shown good results in studies. Treatment choices depend on the patient’s age, health, and disease details.
| Therapeutic Approach | Key Features | Response Assessment |
|---|---|---|
| Ibrutinib | BTK inhibition, oral administration | Clinical response, reduction in IgM levels |
| Plasmapheresis | Removal of IgM antibodies | Reduction in serum viscosity, symptom improvement |
| Chemotherapy | Combination regimens | Tumor response, overall survival |
Checking how well treatment works involves clinical checks, lab tests, and imaging. Regular follow-ups are key to adjusting treatment plans as needed.
Conclusion: Future Directions in B Cell Lymphoma Management
We’ve looked at the different types of B cell lymphomas. Advances in understanding these diseases are leading to new treatments. We’ve talked about how to diagnose and treat these cancers, including specific subtypes.
Looking to the future, research will focus on new treatments like immunotherapies and precision medicine. These advancements will likely make treatments better, giving hope to those with these cancers.
Using new technologies and treatments will be key to better diagnosing and managing B cell lymphomas. It’s important to keep researching and developing new ways to care for patients. This way, we can give patients the best care possible.
We’re hopeful about the future of B cell lymphoma management. We look forward to seeing more progress in this field.
FAQ
What is B cell lymphoma?
B cell lymphoma is a cancer that starts in B lymphocytes. These cells are important for our immune system. It has different types, each with its own traits and effects on health.
What are the common types of B cell lymphomas?
Some common types are Diffuse Large B-Cell Lymphoma (DLBCL), Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma (CLL/SLL), and Follicular Lymphoma. Others include Mantle Cell Lymphoma, Marginal Zone Lymphoma, Burkitt Lymphoma, and Lymphoplasmacytic Lymphoma.
What is the role of diagnostic biomarkers in B cell lymphoma?
Biomarkers like CD19, CD20, and CD79a are key in finding B cell lymphomas. They help doctors diagnose and sort these cancers. This guides how to treat them.
What is Diffuse Large B-Cell Lymphoma (DLBCL)?
DLBCL is the most common B cell Non-Hodgkin Lymphoma (NHL). It grows quickly. It has subtypes like GCB and ABC, which affect how well it can be treated.
How is Follicular Lymphoma managed?
Follicular Lymphoma treatment varies. It depends on the disease’s stage, how it looks under a microscope, and the patient’s health. The t(14;18) translocation is a key genetic sign that affects the disease’s behavior.
What is the significance of the MYC translocation in Burkitt Lymphoma?
The MYC translocation is a genetic sign of Burkitt Lymphoma. It causes cells to grow fast and aggressively. It’s important for diagnosis and needs strong chemotherapy.
What is Waldenström Macroglobulinemia?
Waldenström Macroglobulinemia is a type of Lymphoplasmacytic Lymphoma. It makes too much IgM protein, causing blood to thicken. The MYD88 mutation is key to understanding this disease.
What are the treatment options for Mantle Cell Lymphoma?
Treatment for Mantle Cell Lymphoma depends on how fast it grows. New treatments are being developed, giving patients new hope.
How do infectious triggers contribute to Marginal Zone Lymphoma?
Some Marginal Zone Lymphoma types, like MALT lymphoma, are linked to infections. Knowing this is important for managing the disease.
What is the prognosis for patients with Double-Hit or Triple-Hit DLBCL?
Double-Hit and Triple-Hit DLBCL have a worse outlook. Treatment is often more intense to fight these aggressive forms.
What is Richter’s Transformation in CLL/SLL?
Richter’s Transformation is when CLL/SLL turns into a more aggressive lymphoma, often DLBCL. It needs quick recognition and proper treatment.
What is B cell lymphoma?
B cell lymphoma is a cancer that starts in B lymphocytes. These cells are important for our immune system. It has different types, each with its own traits and effects on health.
What are the common types of B cell lymphomas?
Some common types are Diffuse Large B-Cell Lymphoma (DLBCL), Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma (CLL/SLL), and Follicular Lymphoma. Others include Mantle Cell Lymphoma, Marginal Zone Lymphoma, Burkitt Lymphoma, and Lymphoplasmacytic Lymphoma.
What is the role of diagnostic biomarkers in B cell lymphoma?
Biomarkers like CD19, CD20, and CD79a are key in finding B cell lymphomas. They help doctors diagnose and sort these cancers. This guides how to treat them.
What is Diffuse Large B-Cell Lymphoma (DLBCL)?
DLBCL is the most common B cell Non-Hodgkin Lymphoma (NHL). It grows quickly. It has subtypes like GCB and ABC, which affect how well it can be treated.
How is Follicular Lymphoma managed?
Follicular Lymphoma treatment varies. It depends on the disease’s stage, how it looks under a microscope, and the patient’s health. The t(14;18) translocation is a key genetic sign that affects the disease’s behavior.
What is the significance of the MYC translocation in Burkitt Lymphoma?
The MYC translocation is a genetic sign of Burkitt Lymphoma. It causes cells to grow fast and aggressively. It’s important for diagnosis and needs strong chemotherapy.
What is Waldenström Macroglobulinemia?
Waldenström Macroglobulinemia is a type of Lymphoplasmacytic Lymphoma. It makes too much IgM protein, causing blood to thicken. The MYD88 mutation is key to understanding this disease.
What are the treatment options for Mantle Cell Lymphoma?
Treatment for Mantle Cell Lymphoma depends on how fast it grows. New treatments are being developed, giving patients new hope.
How do infectious triggers contribute to Marginal Zone Lymphoma?
Some Marginal Zone Lymphoma types, like MALT lymphoma, are linked to infections. Knowing this is important for managing the disease.
What is the prognosis for patients with Double-Hit or Triple-Hit DLBCL?
Double-Hit and Triple-Hit DLBCL have a worse outlook. Treatment is often more intense to fight these aggressive forms.
What is Richter’s Transformation in CLL/SLL?
Richter’s Transformation is when CLL/SLL turns into a more aggressive lymphoma, often DLBCL. It needs quick recognition and proper treatment.





