Last Updated on November 17, 2025 by Ugurkan Demir
Blood clots are the body’s natural defense to stop bleeding and start healing. However, when clots form in the wrong place or don’t dissolve properly, they can become life-threatening.
At LivHospital, we understand how crucial it is to know the kinds of blood clots that can develop in the body. Each type affects your health differently and requires specific medical attention.
Our medical experts provide top-quality care for patients worldwide, ensuring that each case is handled with precision and care. In this guide, we explore the main types of blood clots, their causes, and their impact on overall health.
Key Takeaways
- Knowing the different types of blood clots is key to staying healthy.
- Blood clots can be deadly if they cut off blood to vital organs.
- LivHospital offers world-class healthcare.
- We prioritize support for international patients.
- Learning about blood clot types helps in early detection and treatment.
Understanding Blood Clots: Formation and Classification

It’s important to know about blood clots to understand heart problems. Blood clots form as a natural response to injury. But, when they form in the wrong place, they can cause serious health issues.
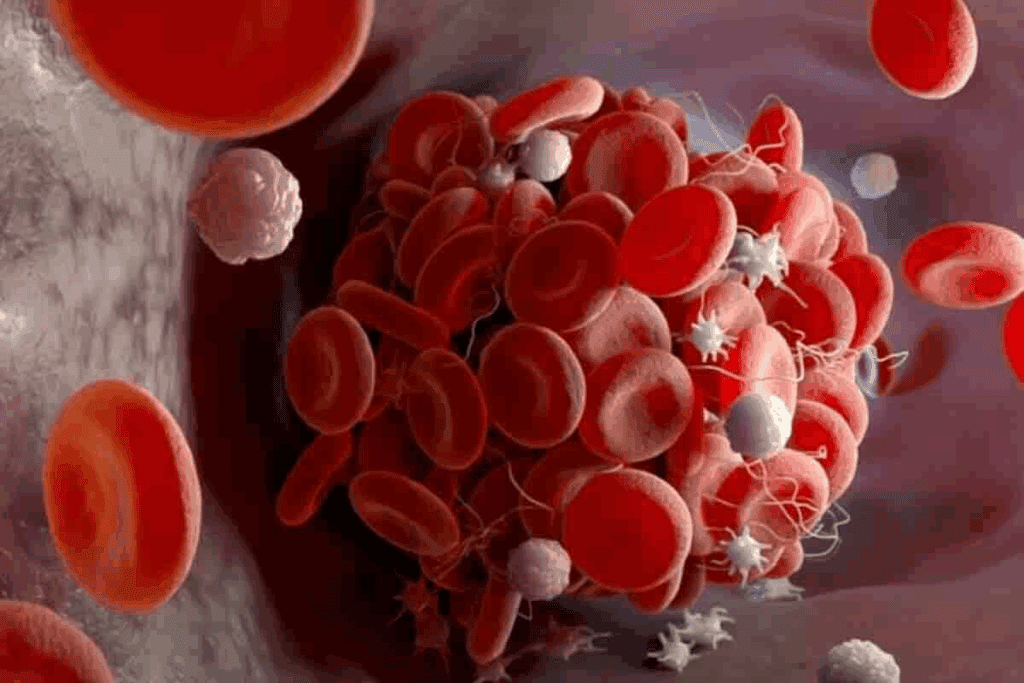
The Blood Clotting Process
Blood clots form through a complex process. Platelets and fibrin play key roles. When a blood vessel gets injured, platelets stick together and to the vessel wall.
This creates a plug that stops bleeding temporarily. Then, fibrinogen turns into fibrin, making the clot stronger. Together, platelets and fibrin form a clot that stops bleeding well.
What Is a Blood Clot Called: Medical Terminology
In medical terms, a stationary blood clot is called a thrombus. If a thrombus breaks loose and moves through the blood, it’s an embolus. Knowing these terms helps us understand the dangers of blood clots.
| Term | Definition |
| Thrombus | A stationary blood clot that forms within a blood vessel. |
| Embolus | A blood clot that has broken loose and is traveling through the bloodstream. |
It’s key to know the difference between a thrombus and an embolus. An embolus can cause serious problems if it blocks a vital area, like the lungs or brain.
Different Kinds of Blood Clots: Physical Characteristics
The look and feel of blood clots tell us a lot about their health risks. Clots can look and feel very different, which is important for knowing their impact on our bodies.
Are Blood Clots Hard or Soft?
Blood clots can be either soft or hard, depending on how old they are. New clots are soft and break easily, while older ones are harder and more stable. The feel of a clot can show how long it’s been in the body.
Many wonder if blood clots are hard or soft. It really depends on the clot’s age. New clots are softer and more likely to break, while older ones are more solid.
Jelly-Like Blood: Appearance and Texture
Blood clots often look like reddish, jelly-like masses. This is because red blood cells get trapped in the clot’s mesh. The jelly-like feel is common in many clots, mostly the new ones.
The look of blood clots can be described as “jelly-like” or “blood like jelly.” This comes from the clot’s mix of platelets, fibrin, and blood cells. Knowing how clots look and feel helps us spot health problems.
In summary, the look and feel of blood clots are key to understanding their risks. By knowing if a clot is soft or hard and its jelly-like look, we can spot health risks better.
Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis, or DVT, is a serious condition. It happens when a blood clot forms in a deep vein, usually in the legs. This can cause serious health problems if not treated quickly.
Common Locations and Symptoms
DVT often happens in the legs, like the calf or thigh. Symptoms include swelling, redness, and tenderness in the leg. Some people might feel pain or warmth where the clot is.
But, DVT can also be without symptoms. This makes it hard to catch without a doctor’s check-up. When symptoms do show up, they can mean the clot is serious and needs quick medical help.
Risk Factors for DVT
Several things can make you more likely to get DVT. These include:
- Recent Surgery or Injury: Surgery or injuries can hurt veins and raise clot risk.
- Immobility: Long periods without moving, like on flights or in bed, can cause clots.
- Family History: If your family has DVT, you’re more at risk.
- Age and Obesity: Being over 40 and overweight also increases risk.
Potential Complications
If DVT is not treated, it can cause big problems. The biggest risk is the clot breaking loose and going to the lungs. This can be deadly.
Other issues include post-thrombotic syndrome. This is chronic pain, swelling, and skin color changes in the affected limb.
Knowing the risks and spotting DVT symptoms early is key. It helps get medical help fast and avoid long-term health issues.
Pulmonary Embolism (PE)
A blood clot that moves to the lungs is a serious issue. We’ll look into what causes it, its symptoms, and why quick medical help is key.
A Moving Blood Clot Is Called an Embolus
An embolus is a blood clot that travels in the blood. If it reaches the lungs, it can block a pulmonary artery. This is a life-threatening situation that needs immediate care.
Recognizing PE Symptoms
Symptoms of pulmonary embolism include shortness of breath, chest pain, and coughing up blood. Spotting these signs early is vital for treatment.
Emergency Response and Treatment
Pulmonary embolism is a medical emergency. It needs quick treatment. Doctors might use medicines to stop more clots or remove the clot. Fast action is essential to avoid serious problems or death.
Arterial Thrombosis
Arterial thrombosis is a serious condition where a blood clot forms in an artery. This is different from other blood clots because arteries carry oxygen-rich blood. It’s vital to get medical help right away.
Differences Between Arterial and Venous Clots
Arterial clots and venous clots are not the same. Arterial clots are more likely to be platelet-rich, while venous clots are fibrin-rich. This affects how they are treated.
- Arterial clots form in high-pressure arteries.
- They often cause acute symptoms like severe pain or loss of function.
- Treatment usually involves anticoagulation and sometimes thrombolysis.
Heart Attacks and Strokes: The Connection
Arterial thrombosis is a major cause of heart attacks and strokes. If an arterial clot blocks blood flow to the heart, it can cause a myocardial infarction, or heart attack. If it blocks blood flow to the brain, it can cause an ischemic stroke.
Immediate Treatment Needs
The symptoms of arterial thrombosis, like sudden chest pain or neurological deficits, need immediate medical help. Quick treatment can greatly improve outcomes by restoring blood flow.
- Administering anticoagulant medications to prevent further clotting.
- Using thrombolytic therapy to dissolve the clot.
- In some cases, performing surgical procedures to remove the clot or bypass the blocked artery.
It’s important to understand the urgency of arterial thrombosis for prevention and treatment. Recognizing risk factors and symptoms can help save lives by getting timely medical help.
Superficial Venous Thrombosis
A blood clot near the skin’s surface is called superficial venous thrombosis. It can cause pain and discomfort. But, it’s usually less serious than deep vein thrombosis (DVT).
Distinguishing from DVT
The main difference is where the clot forms. Superficial venous thrombosis happens in veins close to the skin. DVT forms in deeper veins, like in the legs. Both have blood clots, but they’re not the same.
Key differences include:
- The location of the clot: superficial vs. deep veins
- Risk of pulmonary embolism: lower in superficial venous thrombosis
- Symptoms: while both can cause pain and swelling, DVT can lead to more severe complications
Common Causes and Risk Factors
Several factors can raise the risk of getting superficial venous thrombosis. These include:
- Varicose veins
- Recent trauma or injury to the affected limb
- Prolonged periods of immobility
- Certain medical conditions, such as cancer or autoimmune disorders
Knowing these risk factors helps in preventing and catching superficial venous thrombosis early.
Management and Prognosis
Managing superficial venous thrombosis focuses on easing symptoms and stopping clot growth. Treatment may include:
- Anticoagulant medications to prevent clot progression
- Compression stockings to reduce swelling
- Pain management through medication
Most people get better within a few weeks. But, it’s important to keep an eye on things and follow up to avoid problems.
Cerebral Venous Sinus Thrombosis
Cerebral Venous Sinus Thrombosis happens when blood clots block the cerebral venous sinuses. These sinuses are key for draining blood from the brain. This rare condition can cause headaches, seizures, and other brain problems.
Dangers and Unique Aspects
The main danger of Cerebral Venous Sinus Thrombosis is its location in the cerebral venous sinuses. It can lead to high brain pressure, swelling, and even bleeding. This condition can cause serious brain damage.
Key risks include:
- Severe headache
- Seizures
- Neurological deficits
- Cerebral edema
Diagnostic Challenges
Diagnosing Cerebral Venous Sinus Thrombosis is hard because its symptoms are similar to other brain conditions. MRI and CT venography are key for finding the right diagnosis.
The diagnostic process typically involves:
- Clinical evaluation
- Imaging studies (MRI, CT venography)
- Laboratory tests to assess clotting factors
Treatment Approaches
Treating Cerebral Venous Sinus Thrombosis usually means using anticoagulation therapy. This helps prevent more clots and dissolves existing ones. Sometimes, more intense treatments are needed.
Treatment options include:
- Anticoagulation therapy
- Thrombolysis in selected cases
- Management of complications (e.g., seizures, intracranial hypertension)
Risk Factors and Prevention of Different Types of Blood Clots
Blood clots can be caused by genetics, lifestyle, and the environment. Knowing these factors helps prevent and catch blood clots early.
Who Is at Risk?
Many things can make someone more likely to get blood clots. These include:
- Immobility: Long periods without moving, like on flights or in bed, raise the risk.
- Surgery: Operations, like those on the hips, knees, or belly, can cause blood clots.
- Cancer: Some cancers and treatments can increase the risk of blood clots.
- Genetic Disorders: Conditions like Factor V Leiden thrombophilia can make blood clotting more likely.
- Lifestyle Factors: Being overweight, smoking, and not being active also raise the risk.
Knowing who’s at risk is key to stopping blood clots. Healthcare providers can then take steps to prevent them.
Preventive Measures
Preventing blood clots requires lifestyle changes and medical help. Some good ways to prevent them include:
- Anticoagulant Medications: These drugs stop blood clots from forming.
- Compression Stockings: These stockings help blood flow better and lower clot risk.
- Staying Hydrated: Drinking enough water is key for blood flow and avoiding dehydration, which can cause clots.
- Regular Exercise: Moving regularly improves blood flow and lowers clot risk.
By taking these steps, people can greatly lower their chance of getting dangerous blood clots.
Conclusion: Recognizing and Responding to Blood Clot Dangers
It’s important to know the signs of blood clots and act fast. This can prevent serious problems and improve health outcomes. We’ve looked at the different types of blood clots, how they form, and their risks.
At LivHospital, we focus on top-notch care for blood clot patients. Our team is ready to provide world-class healthcare. We aim to give our patients the best treatment and support.
Understanding blood clot dangers and acting quickly can lower serious risks. If you think you have a blood clot, get medical help right away. Quick action is key to dealing with blood clots effectively.
FAQ
What is a blood clot called in medical terms?
In medicine, a blood clot is called a thrombus if it stays in one place. It’s called an embolus if it moves through the blood.
Are blood clots hard or soft?
Blood clots can be either soft or hard. Fresh ones are soft and jelly-like. Older ones tend to be harder.
What does a blood clot look like?
Blood clots look like jelly-like masses. Their look can change based on where they are and how much blood they have.
What is Deep Vein Thrombosis (DVT)?
Deep Vein Thrombosis is when a blood clot forms in deep veins, usually in the legs. It can cause swelling, pain, and redness in the affected limb.
What is a moving blood clot called?
A moving blood clot is called an embolus. When it travels and blocks a smaller vessel, it can cause a blockage.
What are the symptoms of Pulmonary Embolism (PE)?
Pulmonary Embolism symptoms include sudden shortness of breath and chest pain that gets worse with deep breathing. Coughing up blood is also a symptom. It’s a medical emergency.
How does Arterial Thrombosis differ from Venous Thrombosis?
Arterial Thrombosis happens when a clot forms in an artery. This can lead to heart attacks or strokes. Venous Thrombosis, like in Deep Vein Thrombosis, involves clotting in veins.
What is Cerebral Venous Sinus Thrombosis?
Cerebral Venous Sinus Thrombosis is a rare condition where a clot forms in the brain’s venous sinuses. It can cause severe headache and seizures.
How can I reduce my risk of developing blood clots?
To lower your risk, use anticoagulant meds as directed, wear compression stockings, stay hydrated, and avoid sitting for too long.
What are the risk factors for developing different types of blood clots?
Risk factors include genetic predispositions, lifestyle choices like smoking and obesity, and prolonged sitting. Certain medical conditions also increase risk. Knowing these can help prevent blood clots.
Reference
- NIH National Heart, Lung, and Blood Institute – Pulmonary Embolism





