At Liv Hospital, we understand how serious thrombosis can be. It’s when a blood clot forms inside a blood vessel, blocking blood flow. This can happen in veins and arteries, leading to serious health issues if not treated quickly. If you’re wondering what is thrombotic, it refers to these blood clots that can obstruct circulation and require prompt medical attention.
We aim to give our patients the best care for thrombotic conditions. It’s important to know the risks, symptoms, and treatments for thrombosis. This knowledge helps us provide effective medical care.
Key Takeaways
- Thrombosis is the formation of a blood clot inside a blood vessel.
- It can occur in both veins and arteries.
- Prompt medical attention is key for managing thrombotic conditions.
- Knowing the causes, symptoms, and treatments is vital for good care.
- Liv Hospital is dedicated to providing top-notch care for thrombotic conditions.
The Definition and Mechanism of Thrombosis
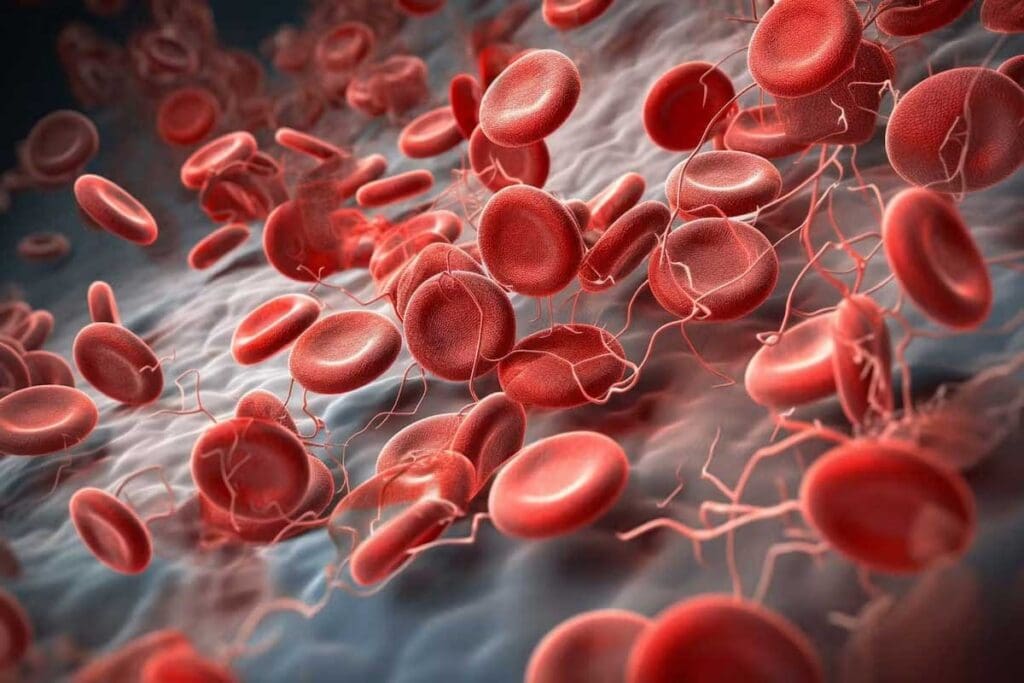
The term thrombosis means the formation of a thrombus or blood clot in a blood vessel. This can have big health effects. Knowing about thrombosis helps us understand how blood clots form and affect our blood vessels.
Medical Definition of Thrombotic Conditions
Thrombotic conditions happen when blood clots form in the blood vessels. This can happen in veins and arteries. It leads to different health problems based on where and how big the clot is. Thrombosis involves platelets, fibrin, and other clotting factors.
Thrombotic conditions are when blood clots form in vessels. This can block blood flow and cause tissue damage or organ problems. It’s important to know the difference between thrombosis and normal clotting to understand what’s happening.
How Blood Clots Form in Vessels
Blood clot formation, or thrombogenesis, is a balance between clotting and preventing clotting. When a blood vessel gets hurt, the body tries to stop bleeding by forming a clot. This starts with platelets and the coagulation cascade, making a fibrin clot.
In thrombosis, this clotting process goes wrong. It makes harmful clots that block blood flow. Things like blood stasis, hypercoagulability, and injury to the blood vessel wall can cause these problems.
The Difference Between Normal Clotting and Thrombosis
Normal clotting helps stop too much bleeding. But thrombosis happens when clotting goes wrong, making harmful clots. The main difference is how and when clotting happens.
Normal clotting is a quick response to injury. But thrombosis can happen without injury and can be very dangerous. Knowing the difference is key to diagnosing and treating blood clotting problems.
Terminology and Language Variations
Thrombosis is a condition where blood clots form. It’s known by different names in various languages and medical traditions. Knowing these names is key for doctors and patients to get the right treatment.
Etymology of “Thromb” and Related Terms
The word “thrombosis” comes from the Greek “thrombos,” meaning clot. This root is important for understanding the condition and its many names. Many medical terms related to clotting start with “thromb.”
Thrombosis is more than a medical term; it’s a word used worldwide. Its history shows how medical terms can be precise yet complex.
International Terminology: Trombos, Thrombose, Tromboza
Many languages have their own versions of “thrombosis.” For example, in European languages, the term is often changed:
| Language | Term for Thrombosis |
| Spanish | Trombo |
| French | Thrombose |
| Polish | Tromboza |
| Portuguese | Trombose |
This table shows how different languages refer to thrombosis. It highlights the need for clear communication in global healthcare.
“The clarity of medical terminology is key for good patient care. This is even more important in a world where doctors from many languages work together.”
Common Misspellings: Thorombosis, Trbosis, Trembosis
Misspelling medical terms can cause confusion. Words like “thorombosis,” “trbosis,” and “trembosis” are often misspelled. Knowing these can help make medical talk clearer.
Getting the spelling right is vital for correct treatment. Doctors and patients must pay attention to the words used in medical records and talks.
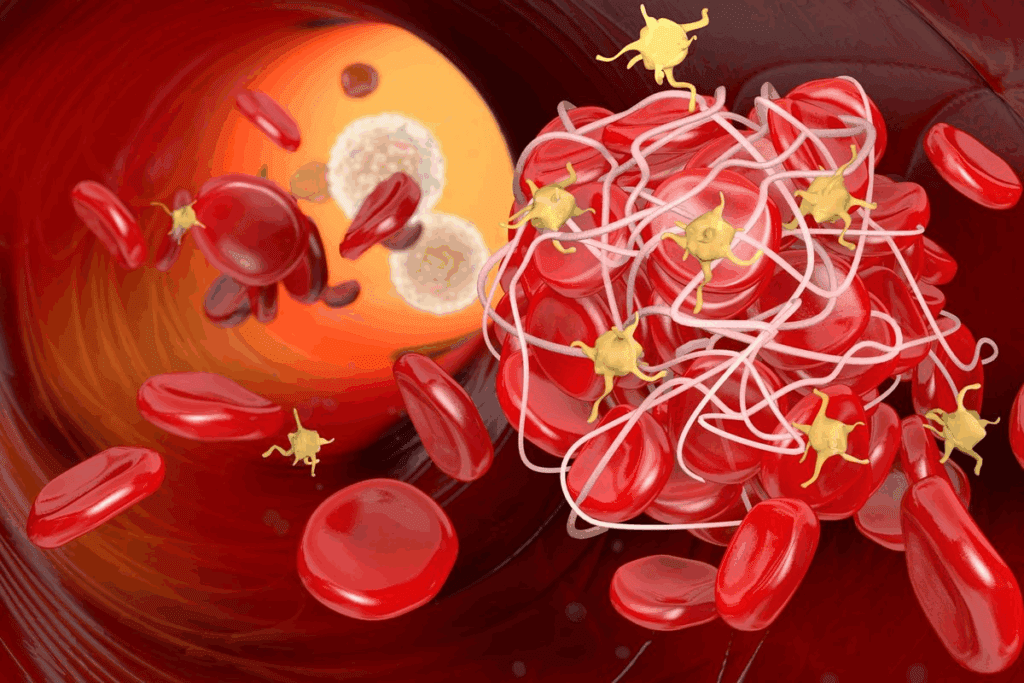
Types of Thrombotic Disorders
Thrombotic disorders are conditions where blood clots form in the body’s circulatory system. These clots can affect health, depending on where and how severe they are.
We’ll look at venous thrombosis, arterial thrombosis, and pulmonary thrombosis/embolism. Each has its own traits and risks.
Venous Thrombosis: Deep Vein Thrombosis (DVT)
Venous thrombosis is when a blood clot forms in a vein. Deep Vein Thrombosis (DVT) happens in the deep leg veins. It can cause serious problems and even lead to a life-threatening condition if the clot moves to the lungs.
Symptoms of DVT include swelling, pain, and color changes in the leg. Risk factors include being immobile, having surgery, or having a family history.
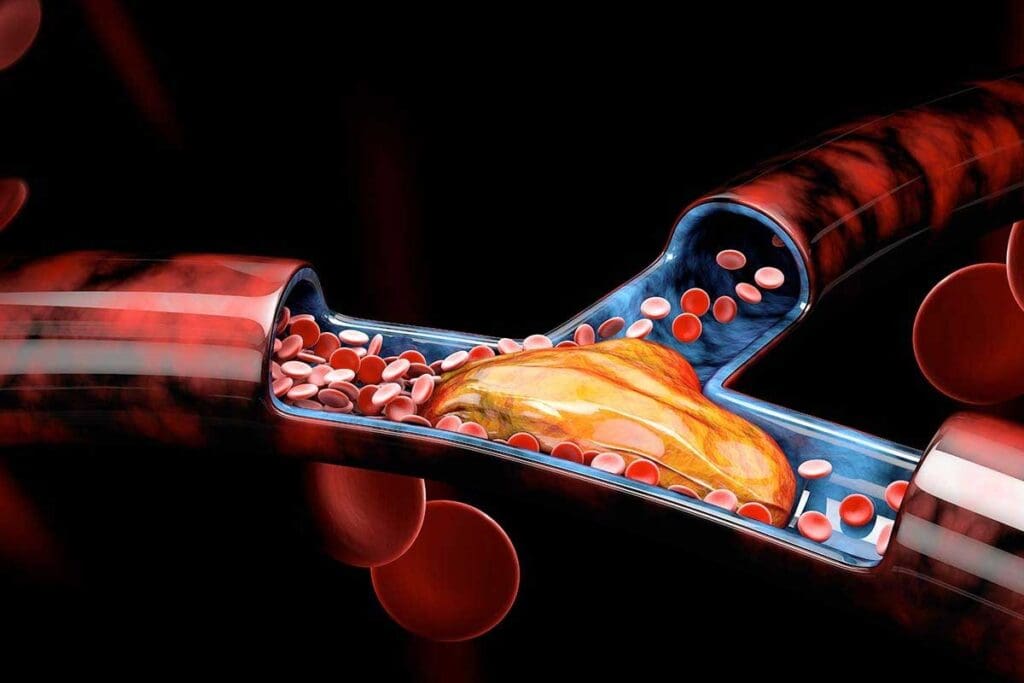
Arterial Thrombosis
Arterial thrombosis is when a clot forms in an artery. This can cut off blood flow to tissues or organs. It’s often linked to atherosclerosis and can cause heart attacks or strokes.
The symptoms of arterial thrombosis vary by location but may include sudden pain, numbness, or weakness. Quick medical help is key to prevent damage.
Pulmonary Thrombosis and Embolism
Pulmonary thrombosis is when a clot forms in the pulmonary arteries. Pulmonary embolism is when a clot, often from DVT, goes to the lungs. It’s a serious condition that needs immediate care.
Symptoms of pulmonary embolism include sudden shortness of breath, chest pain, and coughing up blood. The severity can vary, but severe cases need emergency treatment.
| Type of Thrombotic Disorder | Common Location | Potential Complications |
| Venous Thrombosis (DVT) | Deep veins of the legs | Pulmonary Embolism |
| Arterial Thrombosis | Arteries supplying vital organs | Myocardial Infarction, Stroke |
| Pulmonary Thrombosis/Embolism | Pulmonary arteries | Respiratory failure, Cardiac arrest |
What Is Thrombotic Risk? Understanding Predisposing Factors
Thrombotic risk is complex, involving genetics, lifestyle, and situations. It’s about the chance of getting a blood clot, like deep vein thrombosis (DVT) or pulmonary embolism (PE).
Genetic Risk Factors
Genetics play a big part in blood clotting. Some inherited traits can make blood clot more easily, raising the risk of clots.
- Factor V Leiden mutation
- Prothrombin gene mutation
- Antithrombin deficiency
- Protein C and Protein S Deficiency
Acquired Risk Factors
Medical conditions and lifestyle choices can also up the risk of blood clots. These factors affect how blood clots or flows.
| Condition | Description | Impact on Thrombotic Risk |
| Cancer | Malignant diseases that can affect clotting | Increased |
| Autoimmune diseases | Conditions like lupus that can increase clotting risk | Increased |
| Obesity | Excess body weight affects circulation and clotting | Increased |
Situational Risk Factors
Situations like surgery, staying in bed too long, or getting hurt can also raise the risk of blood clots. Knowing these risks helps us prevent them.
Situational Risk Factors to Consider:
- Major surgery
- Prolonged immobility
- Trauma or significant injury
Understanding these risks helps us figure out who might get a blood clot. Then, we can take steps to prevent it.
Global Prevalence and Epidemiology
It’s key to understand thrombotic disorders to fight them better. These conditions, like venous thromboembolism (VTE), cause a lot of sickness and death worldwide.
Worldwide Incidence of Venous Thromboembolism
Venous thromboembolism, or VTE, includes deep vein thrombosis (DVT) and pulmonary embolism (PE). It affects many people globally. The yearly rate of VTE is about 1 to 2 per 1,000 adults.
Some groups face a higher risk of VTE. These include older people and those with cancer or recent surgery. The risk also grows with age, affecting older populations worldwide.
High-Risk Populations and Settings
Some groups are more likely to get thrombotic disorders. These include:
- Hospitalized patients, mainly those having big surgeries or being bedridden for a long time
- People with genetic risks, like the factor V Leiden mutation
- Cancer patients, as cancer increases the risk of VTE
These high-risk groups need special care and watchful monitoring to lower the risk of blood clots.
Regional Variations in Thrombotic Disorders
The risk of blood clots varies by region and ethnicity. For example, the factor V Leiden mutation is more common in Europeans. Knowing these differences helps us make health plans and guidelines that fit each area’s needs.
Dealing with blood clot issues worldwide needs a broad plan. This includes teaching, prevention, and treatment that meet the needs of different people.
Signs and Symptoms of Thrombotic Conditions
Thrombotic disorders show different signs and symptoms based on the type and location of the clot. Clots can form in veins or arteries, leading to different symptoms.
Thrombotic conditions are serious and can be life-threatening if not treated quickly. Knowing the warning signs is key to managing the condition and preventing serious problems.
Common Symptoms of Venous Thrombosis
Venous thrombosis, like deep vein thrombosis (DVT), often causes swelling, pain, or tenderness in the affected limb. The skin may also become warm, red, or discolored. Sometimes, symptoms are mild, making diagnosis tricky.
Symptoms include:
- Pain or tenderness in the leg
- Swelling in the affected limb
- Warmth or redness of the skin
- Visible veins
Warning Signs of Arterial Thrombosis
Arterial thrombosis can cause sudden limb ischemia or organ dysfunction. Symptoms can appear suddenly and include severe pain, coldness, numbness, and paralysis.
In the case of a stroke due to arterial thrombosis in the brain, symptoms include:
- Sudden weakness or numbness in the face or limbs
- Difficulty speaking or understanding speech
- Sudden vision changes
- Severe headache
Emergency Symptoms Requiring Immediate Attention
Certain symptoms are a medical emergency. For example, pulmonary embolism, which happens when a clot travels to the lungs, needs immediate care. Symptoms include sudden shortness of breath, chest pain, and coughing up blood.
| Condition | Symptoms | Emergency |
| Deep Vein Thrombosis (DVT) | Leg pain, swelling, warmth | No |
| Arterial Thrombosis | Sudden limb pain, numbness, coldness | Yes |
| Pulmonary Embolism | Sudden shortness of breath, chest pain | Yes |
It’s important to recognize these signs and symptoms for timely treatment. If you or someone else has these emergency symptoms, get medical help right away.
Diagnosis and Assessment Protocols
Getting a correct diagnosis of thrombosis is key. It needs a mix of clinical checks, imaging, and lab tests. Spotting thrombotic disorders right away is the first step to treating them well.
Clinical Assessment and History Taking
First, we look at the patient’s medical history and do a physical check-up. Identifying risk factors like family history or recent surgery is important. Symptoms like pain or swelling in a limb might mean deep vein thrombosis (DVT).
For pulmonary embolism, we watch for chest pain and shortness of breath. We check the patient’s overall health for signs of thrombosis. This includes looking for swelling or tenderness in the affected area. A detailed history helps us figure out who’s at high risk and who needs more tests.
Imaging Techniques for Detecting Thrombosis
Imaging is a big help in finding thrombosis. Ultrasound is often used for DVT, showing the clot in the veins. For pulmonary embolism, CT pulmonary angiography (CTPA) is best, giving clear pictures of the lungs’ blood vessels.
Other tools like venography and MRI might be used too. The right imaging depends on the symptoms and where the clot might be.
Laboratory Tests for Thrombotic Disorders
Labs play a big role in diagnosing and managing thrombotic disorders. The D-dimer test checks for clots in the blood. But it’s not perfect and can be high in other conditions too.
We also do coagulation studies to see how blood clots. And a complete blood count (CBC) to look for other health issues that might lead to thrombosis. Sometimes, we test for genetic conditions that make blood clotting more likely.
Treatment Approaches for Thrombotic Disorders
Treating thrombotic disorders requires different methods, from medicines to surgery. The right treatment depends on the condition, its severity, and the patient’s health. We’ll look at treatments like medicines, clot-dissolving therapy, surgery, and new methods.
Anticoagulant Medications
Medicines that prevent clotting are key in treating thrombotic disorders. These drugs stop new clots from forming and growing. Common ones include warfarin, heparin, and newer drugs like rivaroxaban and apixaban. Anticoagulant therapy needs careful monitoring to avoid bleeding risks.
Thrombolytic Therapy
Thrombolytic therapy uses drugs to dissolve clots. It’s mainly for severe cases like stroke or massive pulmonary embolism. Drugs like alteplase activate the body’s clot-dissolving system. But, it can increase bleeding risk.
Surgical Interventions
Surgery is sometimes needed for thrombotic disorders. Procedures like removing clots or emboli can save lives. Surgical thrombectomy is considered for severe cases or when medicines don’t work.
Newer Treatment Modalities
New research has led to better treatments for thrombotic disorders. There are safer anticoagulants and fewer side effects of thrombolytics. Also, direct clot treatments via catheter are becoming more common.
As we learn more about thrombotic disorders, treatments will get better. Personalized medicine and new technologies will help manage these complex conditions better.
Prevention Strategies and Support Systems
To lower the risk of blood clots, we need to focus on prevention. This includes making lifestyle changes, taking medicines, and having strong support systems. By doing these things, we can greatly reduce the chance of blood clotting problems.
Lifestyle Modifications to Reduce Risk
Changing how we live is key to avoiding blood clots. Regular physical activity helps keep blood flowing well and lowers clot risk. We suggest doing at least 30 minutes of moderate exercise daily.
Eating right is also important. Keeping a healthy weight and eating foods like fruits, veggies, and whole grains helps your blood vessels stay healthy.
It’s also important to avoid sitting or standing for too long. On long trips, get up and move around often. People who sit or stand a lot for work should also move more to lower their risk.
- Drink lots of water to stay hydrated
- Try not to smoke and drink alcohol in moderation
- Use stress-reducing activities like meditation or deep breathing
Prophylactic Medications and Approaches
Medicines also play a big role in preventing blood clots, mainly for those at high risk. Anticoagulant medications help stop blood clots from forming. For some, antiplatelet therapy is used to prevent artery blockages.
Choosing the right medicine depends on the person’s risk factors, health history, and the type of clotting problem they face. It’s important to check and adjust these medicines regularly to keep them safe and effective.
| Medication Type | Use | Monitoring |
| Anticoagulants | Prevent blood clot formation | Regular blood tests to check clotting times |
| Antiplatelet agents | Prevent platelet aggregation | Periodic assessment of platelet function |
Patient Support Resources and Care Pathways
Helping patients is key to managing blood clotting problems. We teach them about their condition, treatment options, and the need to follow their treatment plans. We also offer help with lifestyle changes and dealing with the emotional side of blood-clotting issues.
We have care plans to make sure patients get the right care in different places. This means a team of doctors, specialists, and nurses works together to help patients get better.
By using lifestyle changes, medicines, and strong support, we can greatly lower the risk of blood clots. Our goal is to give each patient the care they need, tailored to their unique situation.
Conclusion: Advances in Thrombotic Research and Care
We’ve looked into the world of thrombotic disorders. This includes what they are, their types, risk factors, and how to treat them. New research advances have helped us understand these conditions better. This has led to better care for those with thrombotic issues.
Venous thromboembolism (VTE) is a big health problem worldwide. It affects 1 to 2 people per thousand each year. Researchers are working on new treatments to lower the risk of more blood clots and related problems like post-thrombotic syndrome (PTS) and chronic thromboembolic pulmonary hypertension (CTEPH).
As we learn more about treating thrombotic disorders, it’s key to find effective treatments. This will help improve the lives of those dealing with these conditions. By taking a complete approach to care, we can lessen the impact of these diseases and make life better for those affected.
FAQ
What is thrombosis?
Thrombosis is when a blood clot forms inside a blood vessel. This can block blood flow and cause serious health problems.
What is the difference between normal clotting and thrombosis?
Normal clotting helps stop bleeding when a blood vessel is injured. Thrombosis happens when a clot forms without injury or in the wrong place, blocking blood flow.
What are the risk factors for developing thrombotic conditions?
Risk factors include genetic conditions, certain diseases like cancer, and situations like surgery or immobility.
What are the symptoms of venous thrombosis?
Symptoms include swelling, pain, and tenderness in the affected limb. You might also see warmth or redness on the skin.
How is thrombosis diagnosed?
Doctors use clinical checks, imaging like ultrasound, and blood tests to diagnose thrombosis.
What are the treatment options for thrombotic disorders?
Treatments include anticoagulant drugs, thrombolytic therapy, surgery, and newer methods like catheter-directed thrombolysis.
Can thrombosis be prevented?
Yes, you can prevent or lower the risk of thrombosis with lifestyle changes. This includes regular exercise and avoiding long periods of sitting.
What is pulmonary thrombosis/embolism?
Pulmonary thrombosis/embolism is when a blood clot travels to the lungs. It can block blood flow and is very dangerous.
Are there different types of thrombotic disorders?
Yes, there are various types. These include venous thrombosis, arterial thrombosis, and pulmonary thrombosis/embolism. Each has its own risks and symptoms.
How common are thrombotic disorders?
Thrombotic disorders are a big health problem worldwide. Venous thromboembolism is a major cause of illness and death, affecting many people.
References:
- McLendon, K., & Willis, J. (2023). Deep venous thrombosis risk factors. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK470215/








