Last Updated on November 26, 2025 by Bilal Hasdemir

Receiving a cancer diagnosis and undergoing chemotherapy can be overwhelming. At Liv Hospital, we are committed to providing world-class healthcare with complete support for our international patie
nts. Understanding the typical number of chemotherapy cycles and treatment frequency can help you feel more in control.
The number of chemotherapy rounds can vary significantly based on several factors, including the type and stage of cancer, the specific chemotherapy regimen, and the patient’s overall health. Typically, the number of chemotherapy cycles ranges from four to eight per treatment course.
We are here to guide you through every step of your cancer treatment journey, providing you with the necessary support and care.
Key Takeaways
- The number of chemotherapy cycles varies based on cancer type and stage.
- Treatment frequency depends on the specific chemotherapy regimen.
- Understanding chemotherapy cycles can help patients feel more in control.
- Liv Hospital provides comprehensive support for international patients.
- The typical number of chemotherapy cycles ranges from four to eight.
Understanding Chemotherapy as a Cancer Treatment
As a systemic treatment, chemotherapy plays a vital role in fighting cancer by targeting rapidly dividing cells. Chemotherapy is a crucial component of cancer treatment, using powerful drugs to target and destroy cancer cells. We use chemotherapy to treat various types of cancer, either as a standalone treatment or in combination with other therapies such as surgery or radiation.
What Is Chemotherapy and How It Works
Chemotherapy is a medical treatment that employs potent drugs to kill cancer cells or slow their growth. These drugs work by targeting cells that are dividing rapidly, a characteristic of most cancer cells. By understanding how chemotherapy works, patients can better appreciate the rationale behind their treatment plan.
We administer chemotherapy in cycles, allowing for periods of treatment followed by periods of rest. This cyclical nature of chemotherapy enables the body to recover from the side effects of the treatment, helping to minimize damage to healthy cells.
The Goals of Chemotherapy Treatment
The primary goal of chemotherapy is to eliminate cancer cells, shrink tumors, and prevent the spread of cancer to other parts of the body. In some cases, chemotherapy is used to relieve symptoms or improve quality of life. We tailor the goals of chemotherapy to the individual patient’s needs and medical condition.
By understanding the goals of chemotherapy, patients can have a clearer understanding of what to expect from their treatment and how it fits into their overall care plan.
Defining Key Terminology in Chemotherapy Treatment

The language of chemotherapy can be confusing, but understanding its terms is essential for patients. Chemotherapy is a complex treatment that involves various cycles, rounds, and sessions, which can be overwhelming for those unfamiliar with the terminology.
What Is a Chemotherapy Cycle?
A chemotherapy cycle refers to the period from the start of one round of treatment to the start of the next. For example, a common regimen might involve a treatment every three weeks, known as a ’21-day chemo cycle.’ This cycle includes both the treatment days and the rest periods in between.
Understanding the length and structure of a chemotherapy cycle is crucial for patients to prepare for their treatment and manage their expectations.
Rounds vs. Cycles vs. Sessions: Understanding the Differences
The terms ’rounds,’ ‘cycles,’ and ‘sessions’ are often used interchangeably in chemotherapy, but they have distinct meanings. A chemotherapy round or cycle typically refers to the overall treatment period, while a session refers to a single day of treatment.
- A chemotherapy cycle encompasses the entire period between the start of one treatment and the beginning of the next.
- A session is a single instance of treatment administration.
Treatment Days vs. Rest Periods
Chemotherapy treatment involves both treatment days and rest periods. Treatment days are when chemotherapy drugs are administered, while rest periods allow the body to recover from the treatment’s effects.
During rest periods, the body repairs and rebuilds healthy cells damaged by chemotherapy. Understanding the balance between treatment days and rest periods is vital for patients to manage their treatment effectively.
How Many Rounds of Chemo Is Normal?
Chemotherapy treatment frequency is a common concern for patients, with the standard number of cycles ranging between four to eight. We understand that this information is crucial for patients to plan and prepare for their treatment journey.
The Standard Range of 4-8 Cycles
Generally, the typical number of chemotherapy cycles falls within the range of four to eight per treatment course. This range is considered standard because it allows for the effective treatment of cancer while minimizing the risk of severe side effects. The exact number of cycles within this range is determined by various factors, including the type and stage of cancer, as well as the patient’s overall health.
To illustrate the standard range, let’s consider the following table:
| Cancer Type | Typical Number of Cycles | Treatment Goals |
|---|---|---|
| Breast Cancer | 4-6 cycles | Reduce tumor size, prevent recurrence |
| Colorectal Cancer | 6-8 cycles | Control tumor growth, alleviate symptoms |
| Lymphoma | 4-8 cycles | Induce remission, manage disease progression |
Variations Based on Cancer Type and Stage
The number of chemotherapy rounds can vary significantly based on the type and stage of cancer. For instance, patients with early-stage cancer may require fewer cycles, while those with advanced cancer may need more extensive treatment. We consider these factors when determining the optimal treatment plan for each patient.
“The number of chemotherapy cycles is tailored to the individual patient’s needs, taking into account the specific characteristics of their cancer and overall health status.”
When Fewer or More Cycles May Be Recommended
In some cases, fewer chemotherapy cycles may be sufficient, especially if the cancer is highly responsive to treatment or if the patient is experiencing significant side effects. Conversely, more cycles may be recommended if the cancer is aggressive or if the treatment is not achieving the desired response. We closely monitor each patient’s progress and adjust their treatment plan accordingly.
As shown in the table above, the typical number of chemotherapy cycles can vary based on the cancer type. We also consider other factors, such as the patient’s age, overall health, and previous treatments, when determining the optimal number of cycles.
The Structure of a Typical Chemotherapy Cycle
A typical chemotherapy cycle involves a combination of treatment days and rest periods. This cycle is designed to allow the body to recover from the effects of chemotherapy while still effectively treating cancer.
What Happens During Treatment Days
During treatment days, patients receive their chemotherapy drugs, which can be administered intravenously or orally. The method of administration depends on the type of cancer, the chemotherapy drugs being used, and the individual patient’s needs.
The administration of chemotherapy is typically done in a controlled environment, such as a hospital or clinic, where medical professionals can monitor the patient’s response and manage any immediate side effects.
“Chemotherapy is a systemic treatment that can affect both cancer cells and healthy cells. Understanding what happens during treatment days can help patients prepare for the process.”
The Importance of Rest Periods
Rest periods are a crucial component of chemotherapy cycles. They allow the body to recover from the effects of the treatment, giving healthy cells a chance to regenerate and rebuild.
During rest periods, patients may still experience some side effects from the chemotherapy, but these typically begin to subside as the body recovers.
How Healthy Cells Recover Between Treatments
Between treatments, the body works to recover and rebuild healthy cells that have been affected by chemotherapy. This process is essential for maintaining the patient’s overall health and ability to continue with the treatment plan.
The recovery of healthy cells is facilitated by the body’s natural processes, and it is supported by the rest periods built into the chemotherapy cycle.
| Aspect | Treatment Days | Rest Periods |
|---|---|---|
| Purpose | Administer chemotherapy to target cancer cells | Allow the body to recover from treatment effects |
| Activities | Receive chemotherapy drugs, monitoring by medical staff | Rest, manage side effects, follow post-treatment care instructions |
| Impact | Targets cancer cells, may affect healthy cells | Healthy cells regenerate, patient recovers |
Chemotherapy cycles are tailored to the individual patient’s needs and the specific characteristics of their cancer. Understanding the structure of these cycles can help patients better navigate their treatment journey.
Common Chemotherapy Administration Schedules
Understanding chemotherapy administration schedules is crucial for patients undergoing cancer treatment. Chemotherapy schedules can vary significantly based on the type of cancer, the specific drugs used, and the patient’s overall health.
Weekly Chemotherapy Protocols
Weekly chemotherapy protocols involve administering chemotherapy drugs once a week. This schedule is often used for certain types of cancer, such as lymphoma or leukemia. The benefits of weekly protocols include maintaining a consistent level of chemotherapy in the body and potentially reducing the severity of side effects.
Biweekly (Every Two Weeks) Regimens
Biweekly chemotherapy regimens involve treatment every two weeks. This schedule allows for higher doses of chemotherapy to be administered, as the body has more time to recover between treatments. Biweekly regimens are commonly used for cancers such as breast cancer and colorectal cancer.
Three-Week Cycle Treatments
The three-week cycle, also known as the ’21-day chemo cycle,’ is a common schedule where patients receive treatment once every three weeks. This allows for a balance between effective treatment and recovery time. Many chemotherapy protocols, including those for breast cancer and lymphoma, follow this schedule.
Monthly and Other Less Common Schedules
Some chemotherapy regimens are administered on a monthly basis, while others may follow less common schedules tailored to the specific needs of the patient and the type of cancer being treated. These schedules are determined based on the chemotherapy drugs used and the patient’s response to treatment.
We understand that navigating chemotherapy administration schedules can be complex. Our team is dedicated to providing personalized care and support throughout your treatment journey.
Understanding the 21-Day Chemo Cycle
A 21-day chemo cycle means that chemotherapy is given once every three weeks, allowing healthy cells to recover between treatments. This schedule is commonly used in various cancer treatments, offering a balance between effective cancer cell destruction and the recovery of healthy cells.
What Is a 21-Day Chemo Cycle?
The 21-day chemotherapy cycle is a treatment schedule in which chemotherapy drugs are administered once every 21 days. This cycle is repeated for a number of rounds based on the patient’s treatment plan and response to the therapy. The 21-day gap between treatments allows the body, particularly the bone marrow, to recover from the side effects of chemotherapy.
During this cycle, the chemotherapy drugs target rapidly dividing cancer cells. The treatment’s effectiveness and the patient’s tolerance to the therapy are closely monitored by healthcare professionals.
Common Drugs Used in 21-Day Protocols
The specific chemotherapy drugs used in a 21-day protocol can vary widely depending on the type of cancer, the stage of the disease, and the patient’s overall health. Some common drugs used in 21-day cycles include:
- Docetaxel: Often used in treating breast cancer, prostate cancer, and non-small cell lung cancer.
- Doxorubicin: Used in treating various cancers, including breast cancer, lymphoma, and leukemia.
- Cyclophosphamide: Commonly used in treating breast cancer, lymphoma, and leukemia.
For more detailed information on chemotherapy drugs and their administration, you can visit our page on how many rounds of chemo is.
Cancer Types Typically Treated with 21-Day Cycles
The 21-day chemotherapy cycle is versatile and can be used to treat a variety of cancers. Some of the cancer types that are commonly treated with this cycle include:
| Cancer Type | Common Chemotherapy Drugs | Purpose of Treatment |
|---|---|---|
| Breast Cancer | Docetaxel, Doxorubicin, Cyclophosphamide | Adjuvant or neoadjuvant therapy to reduce recurrence risk |
| Colorectal Cancer | 5-Fluorouracil, Oxaliplatin | Adjuvant therapy after surgery or palliative care |
| Lymphoma | Doxorubicin, Cyclophosphamide, Vincristine | Curative or palliative treatment depending on lymphoma type and stage |
Understanding the specifics of your chemotherapy treatment, including the drugs used and the treatment schedule, is crucial for managing expectations and side effects. Always consult with your healthcare provider for personalized information and guidance.
Total Duration of Chemotherapy Treatment
Understanding the total duration of chemotherapy is essential for patients to prepare for their treatment journey. Chemotherapy is a complex treatment that can vary significantly in duration depending on several factors.
We recognize that the length of chemotherapy can be a significant concern for patients. The total duration of chemotherapy treatment varies widely among patients, and it’s crucial to understand the factors that influence this duration.
Standard 3-6 Month Treatment Courses
In many cases, chemotherapy treatment courses last between three to six months. This is a common duration for various types of cancer, where the goal is to achieve significant tumor reduction or remission.
For instance, in cases of early-stage breast cancer, chemotherapy may be administered every two or three weeks for four to six cycles, spanning approximately 3-6 months.
Extended Treatment Protocols (Up to 2 Years)
Some patients may require extended treatment protocols that can last up to two years or more. This is often the case for cancers that are more aggressive or have spread to other parts of the body.
For example, certain types of lymphoma or leukemia may require prolonged chemotherapy treatment, sometimes extending up to 24 months.
Factors That Influence Total Treatment Duration
Several factors can influence the total duration of chemotherapy treatment. These include:
- The type and stage of cancer
- The patient’s overall health and response to treatment
- The specific chemotherapy regimen and its effectiveness
- Whether chemotherapy is used alone or in combination with other treatments like surgery or radiation therapy
To illustrate how these factors can impact treatment duration, let’s consider the following table:
| Cancer Type | Typical Treatment Duration | Factors Influencing Duration |
|---|---|---|
| Early-stage breast cancer | 3-6 months | Tumor size, response to treatment |
| Advanced colorectal cancer | 6-12 months | Extent of spread, response to chemotherapy |
| Lymphoma | Up to 2 years | Type of lymphoma, patient’s overall health |
As shown in the table, the total duration of chemotherapy can vary significantly based on the cancer type and other factors.
We understand that undergoing chemotherapy can be challenging, and knowing what to expect can help patients prepare for their journey. By understanding the factors that influence treatment duration, patients can better plan and cope with their chemotherapy treatment.
Factors That Determine Your Chemotherapy Plan
Determining the right chemotherapy plan involves considering multiple aspects of a patient’s condition and medical history. We understand that every individual’s situation is unique, and several factors come into play when designing an effective treatment strategy.
Cancer Type, Stage, and Characteristics
The type, stage, and characteristics of cancer are crucial in determining the chemotherapy plan. Different cancers respond differently to various chemotherapy agents. For instance, certain drugs are more effective against specific tumor types. The stage of cancer also plays a significant role, as more advanced cancers may require more aggressive treatment. Additionally, the characteristics of the cancer, such as genetic mutations or hormone receptor status, can influence the choice of chemotherapy drugs.
Your Overall Health and Medical History
A patient’s overall health and medical history are also vital considerations. We assess factors such as age, general well-being, and any pre-existing medical conditions. Patients with certain health issues may require adjustments to their chemotherapy regimen to minimize potential side effects. For example, individuals with kidney or liver problems may need dose adjustments or alternative medications.
Previous Treatments and Response
Previous treatments and the patient’s response to them are important factors in determining the chemotherapy plan. If a patient has undergone chemotherapy before, we consider how they tolerated the treatment and how their cancer responded. This information helps us decide whether to continue with the same regimen or switch to a different one. In cases where the cancer has recurred or become resistant to previous treatments, alternative chemotherapy options may be explored.
Treatment Goals and Quality of Life Considerations
Treatment goals and quality of life considerations are also essential in shaping the chemotherapy plan. We work closely with patients to understand their goals, whether it’s to cure the cancer, control its growth, or alleviate symptoms. Balancing the potential benefits of chemotherapy with the potential side effects is crucial. We strive to create a treatment plan that not only effectively targets the cancer but also maintains the patient’s quality of life as much as possible.
By carefully considering these factors, we can develop a personalized chemotherapy plan that addresses the unique needs and circumstances of each patient.
How Doctors Monitor and Adjust Chemotherapy Cycles
We closely monitor patients undergoing chemotherapy to ensure the treatment’s efficacy. This ongoing monitoring is crucial for adjusting the treatment plan as needed to achieve the best possible outcomes.
Blood Tests and Monitoring During Treatment
Blood tests are a critical component of monitoring during chemotherapy. These tests help us assess how the treatment is affecting the patient’s blood cell counts, liver function, and overall health. Regular blood tests enable us to identify potential issues early and make necessary adjustments to the treatment plan.
Key blood tests during chemotherapy include:
- Complete Blood Count (CBC) to monitor blood cell counts
- Liver function tests to assess the liver’s health
- Kidney function tests to evaluate kidney health
Imaging and Response Assessment
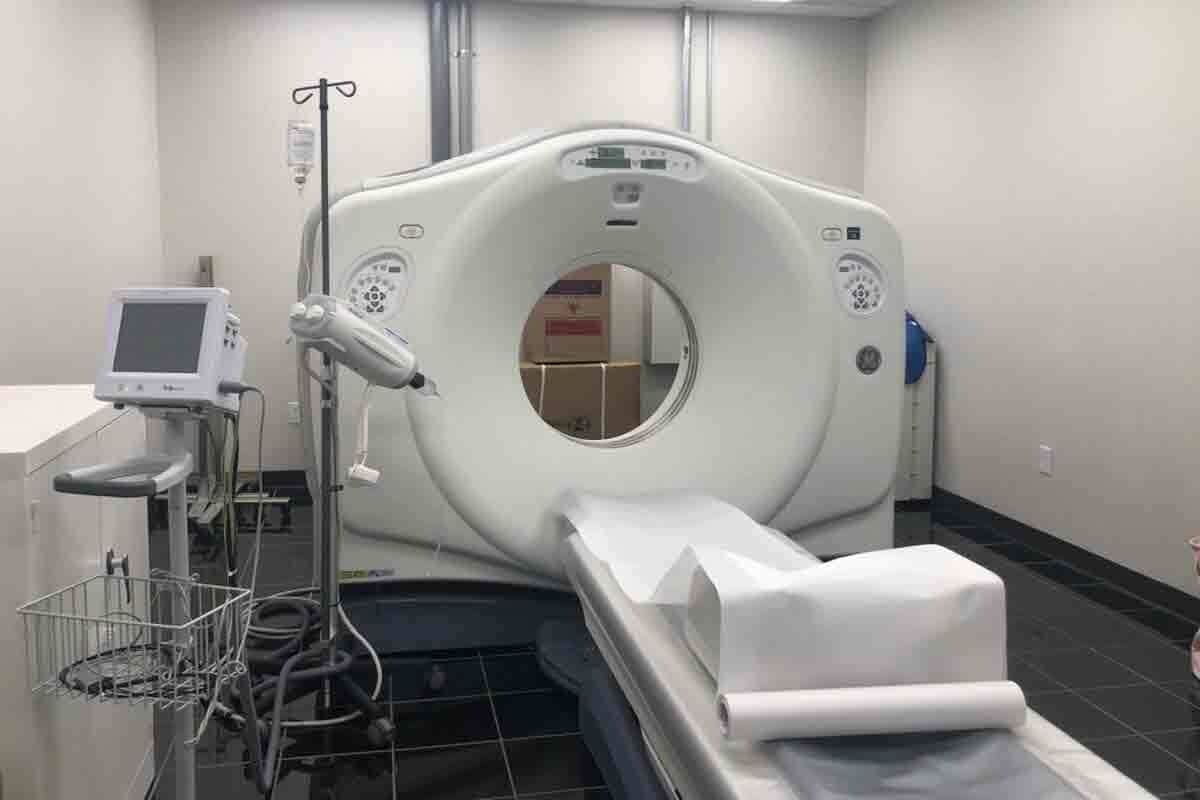
Imaging studies, such as CT scans, MRI, or PET scans, are used to assess how well the cancer is responding to chemotherapy. These imaging tests provide valuable information about the size and spread of tumors, helping us determine if the treatment is effective.
Response assessment categories include:
- Complete response: The cancer is no longer detectable
- Partial response: The cancer has decreased in size
- Stable disease: The cancer has not changed significantly
- Progressive disease: The cancer has grown or spread
When Doctors May Modify Your Treatment Plan
Based on the results of blood tests, imaging studies, and overall health assessments, we may need to modify the chemotherapy treatment plan. Modifications can include changing the dosage, switching to a different chemotherapy regimen, or adding other treatments to enhance effectiveness.
Reasons for modifying a treatment plan include:
- Severe side effects
- Inadequate response to treatment
- Changes in the patient’s overall health
Managing Side Effects Throughout Multiple Chemo Cycles
Effective management of side effects is crucial for patients undergoing multiple cycles of chemotherapy. As treatment progresses, the cumulative effect of chemotherapy can lead to a range of side effects that impact a patient’s quality of life. We understand the importance of managing these side effects to ensure that patients can continue their treatment as planned.
Common Cumulative Side Effects
Cumulative side effects are those that worsen or become more pronounced over the course of multiple chemotherapy cycles. Common examples include:
- Fatigue: a persistent feeling of tiredness that can interfere with daily activities.
- Neuropathy: nerve damage that can cause pain, numbness, or tingling in the hands and feet.
- Cardiac toxicity: potential damage to the heart muscle, which can be a concern with certain chemotherapy drugs.
- Nausea and vomiting: while often associated with individual treatment sessions, these can become more challenging to manage over multiple cycles.
Strategies for Side Effect Management
Managing side effects effectively requires a multi-faceted approach. Some strategies include:
- Medication: using drugs to prevent or alleviate specific side effects, such as anti-nausea medication.
- Lifestyle adjustments: changes to diet, exercise, and daily routines to help mitigate side effects.
- Supportive care measures: additional treatments or therapies that support the patient’s overall health and well-being.
We work closely with patients to develop a personalized plan for managing side effects, ensuring that they receive the support they need throughout their treatment.
When Side Effects May Necessitate Treatment Changes
In some cases, severe or persistent side effects may require adjustments to the chemotherapy treatment plan. This can include:
- Dose reduction: lowering the dose of chemotherapy to reduce the severity of side effects.
- Schedule changes: altering the frequency or timing of treatment sessions to allow for better recovery.
- Alternative treatments: considering different chemotherapy drugs or entirely different treatment modalities.
Our medical team closely monitors patients throughout their treatment, making adjustments as needed to balance the effectiveness of treatment with the management of side effects.
Chemotherapy Protocols for Different Cancer Types
Chemotherapy protocols vary significantly across different cancer types, requiring tailored approaches for effective treatment. We understand that each cancer type has its unique characteristics, necessitating specific chemotherapy regimens.
Breast Cancer Chemotherapy Regimens
For breast cancer, chemotherapy is often used in conjunction with other treatments like surgery and radiation therapy. Common chemotherapy regimens for breast cancer include AC-T (doxorubicin, cyclophosphamide followed by paclitaxel) and TAC (docetaxel, doxorubicin, cyclophosphamide). The choice of regimen depends on factors such as the stage of cancer, hormone receptor status, and HER2 status.
Colorectal Cancer Treatment Schedules
Colorectal cancer treatment often involves chemotherapy combined with surgery. FOLFOX (fluorouracil, leucovorin, oxaliplatin) and FOLFIRI (fluorouracil, leucovorin, irinotecan) are common chemotherapy regimens used. The choice between these regimens depends on the stage and location of the tumor, as well as the patient’s overall health.
Lymphoma and Leukemia Protocols
Lymphoma and leukemia are blood cancers that require specific chemotherapy protocols. For lymphoma, R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) is a common regimen, while leukemia treatment may involve protocols like Hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone). These treatments are often intensive and require careful monitoring.
Lung Cancer Chemotherapy Approaches
Lung cancer chemotherapy varies depending on the type (non-small cell lung cancer vs. small cell lung cancer) and stage. Common regimens include cisplatin or carboplatin-based combinations with drugs like paclitaxel or gemcitabine. For non-small cell lung cancer, targeted therapies may also be used, depending on the presence of specific genetic mutations.
We recognize that understanding these different chemotherapy protocols is essential for providing effective care and optimizing treatment outcomes for patients with various types of cancer.
Conclusion
Navigating cancer treatment can be a complex and challenging experience. At Liv Hospital, we are dedicated to providing comprehensive care and support to our international patients. Understanding chemotherapy cycles and treatment frequency is vital for patients embarking on their cancer treatment journey.
By grasping the typical number of chemotherapy cycles, treatment schedules, and factors influencing treatment plans, patients can better face their cancer treatment with confidence. Our commitment is to implement up-to-date academic protocols and care pathways, ensuring that our patients receive the best possible care.
As you move forward with your treatment, it’s essential to stay informed and engaged in your care. We encourage you to discuss any questions or concerns with your healthcare team. By working together, we can tailor a treatment plan that meets your unique needs and supports you throughout your cancer treatment journey.
FAQ
How many rounds of chemotherapy is normal?
The standard range is typically between 4 to 8 cycles, but this can vary based on the type and stage of cancer, as well as individual patient factors.
What is a chemotherapy cycle?
A chemotherapy cycle refers to the period of treatment followed by a rest period, allowing the body to recover. For example, a 21-day cycle includes treatment days and 17-20 days of rest.
How often do you receive chemotherapy?
The frequency of chemotherapy administration varies. Common schedules include weekly, biweekly, every three weeks, or monthly treatments, depending on the specific protocol.
What is a 21-day chemo cycle?
A 21-day chemo cycle is a treatment schedule where chemotherapy is administered on one or more days, followed by a rest period of approximately 18-20 days, making a total cycle length of 21 days.
How many chemo treatments will I need?
The total number of chemotherapy treatments, or cycles, depends on the cancer type, stage, and how well the treatment is working. Typically, treatment courses last between 3 to 6 months, but can be longer.
Can I have more than 8 cycles of chemotherapy?
While 4-8 cycles are standard, some patients may require more or fewer cycles based on their response to treatment and the specific cancer characteristics.
How do doctors determine the number of chemotherapy cycles?
The decision is based on factors including cancer type and stage, overall health, previous treatments, and how well the cancer responds to chemotherapy.
What happens during rest periods between chemotherapy cycles?
During rest periods, the body recovers from the side effects of chemotherapy, and healthy cells are allowed to regenerate.
How is the effectiveness of chemotherapy monitored?
Doctors monitor the effectiveness through regular blood tests, imaging studies, and physical examinations to assess how well the cancer is responding to treatment.
Can chemotherapy treatment plans be adjusted?
Yes, treatment plans can be modified based on the patient’s response, side effects, and changes in overall health.
Are there different chemotherapy protocols for different cancers?
Yes, chemotherapy protocols vary significantly depending on the type of cancer, its stage, and other individual factors.
How long does chemotherapy treatment typically last?
The duration of chemotherapy treatment can range from a few months to a couple of years, depending on the cancer type and treatment goals.