Last Updated on November 26, 2025 by Bilal Hasdemir
At Liv Hospital, we know how complex diffuse large B-cell lymphoma (DLBCL) is. It’s the most common non-Hodgkin lymphoma, making up about 30-40% of cases worldwide. We take it seriously because it’s aggressive.
DLBCL needs quick and expert care. We aim to give the best diagnosis and treatment. Our team is here to help, providing care and support every step of the way.
Key Takeaways
- DLBCL is an aggressive form of non-Hodgkin lymphoma that requires prompt medical attention.
- At Liv Hospital, patients receive international standards of diagnosis and treatment.
- Our team is committed to delivering compassionate care and providing support.
- Understanding DLBCL is key to managing and treating it effectively.
- Getting expert care can greatly improve treatment results.
Understanding Diffuse Large B Cell Lymphoma (DLBCL)
It’s important for patients and doctors to know about Diffuse Large B Cell Lymphoma (DLBCL). It’s a common type of non-Hodgkin lymphoma.
Definition and Medical Terminology
DLBCL is when B lymphocytes grow fast. These are white blood cells that help fight off infections. The term “diffuse” means the cancer spreads out in the lymph nodes, not just in one spot.
Doctors use terms like “B cell lymphoma,” “non-Hodgkin lymphoma (NHL),” and “aggressive lymphoma” to talk about DLBCL. Knowing these terms helps understand what DLBCL is and how it affects treatment.
Prevalence and Epidemiology
DLBCL is found in about 30-40% of non-Hodgkin lymphoma cases. It’s the most common type of NHL worldwide. The number of cases can vary depending on where you are and who you are.
| Region | Incidence Rate |
|---|---|
| North America | 7-8 cases per 100,000 people per year |
| Europe | 5-6 cases per 100,000 people per year |
| Asia | 3-4 cases per 100,000 people per year |
Studies have found that age, gender, and infections can increase the risk of getting DLBCL.
DLBCL Medical Abbreviation and Related Terms
“DLBCL” means Diffuse Large B Cell Lymphoma. Other terms include “NHL” for non-Hodgkin lymphoma and “ABC-DLBCL” for a specific type of DLBCL.
Knowing these terms helps doctors and patients talk clearly. It makes sure patients get the right diagnosis and treatment.
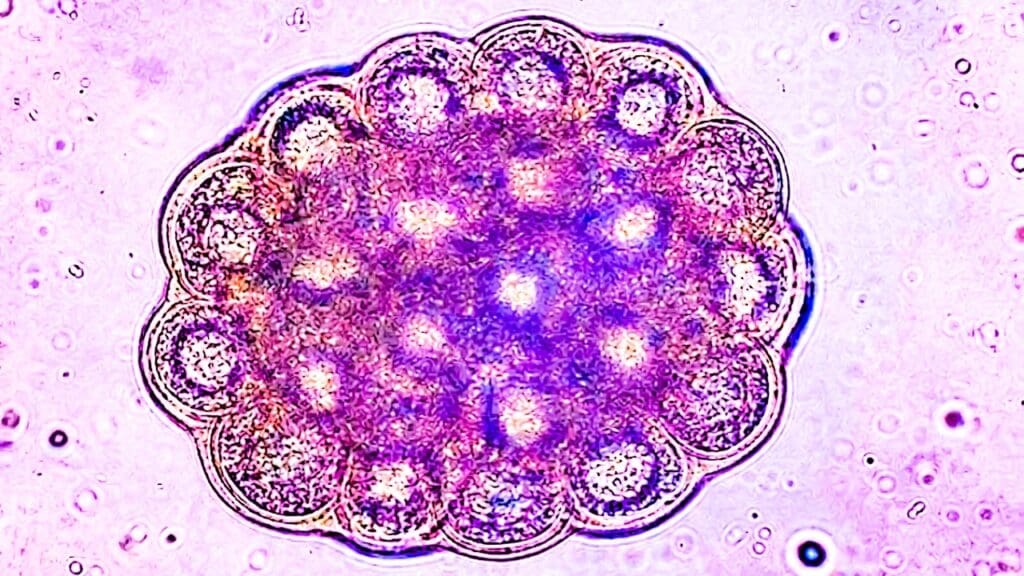
The Biology of Non-Hodgkin DLBCL

Non-Hodgkin DLBCL’s biology is complex. It involves B lymphocytes turning malignant. Knowing this is key to finding good treatments.
B Lymphocytes and Their Normal Function
B lymphocytes, or B cells, are vital to our immune system. They make antibodies to fight off infections. B cells grow in the bone marrow and then move through the blood and lymphatic system.
Malignant Transformation Process
The transformation of B cells into DLBCL happens through genetic changes. These changes cause cells to grow out of control and not die when they should. This can be due to genetics or environmental factors. For more on how lymphoma affects the body, visit Liv Hospital.
Diffuse Growth Pattern Characteristics
DLBCL grows in a way that destroys the lymph node’s structure. This is a key feature of the disease. It makes DLBCL very aggressive.
| Aspect | Description |
|---|---|
| B Lymphocytes | Produce antibodies to fight infections |
| Malignant Transformation | Involves genetic mutations leading to uncontrolled cell growth |
| Diffuse Growth Pattern | Cancer cells infiltrate and destroy normal lymph node architecture |
Types and Subtypes of Large B Cell Non-Hodgkin Lymphoma
Knowing the different types of DLBCL is key to better treatment and outcomes. DLBCL is a complex disease with many subtypes. Each subtype has its own biology and impact on treatment.
Germinal Center B-cell-like (GCB) DLBCL
GCB DLBCL comes from germinal center B cells. It usually has a better outlook than other types, responding well to treatment. Its genes act like those of normal germinal center B cells.
“The distinction between GCB and other subtypes of DLBCL has significant clinical implications, guiding treatment decisions and prognostication.”
Activated B-cell-like (ABC) DLBCL
ABC DLBCL is more aggressive and has a worse outlook. It starts from activated B cells and is often linked to chronic inflammation. Its genes show a unique pattern, linked to its aggressive nature.
Double-Hit and Triple-Hit Lymphomas
Double-hit lymphomas have two genetic changes, often in MYC and BCL2. Triple-hit lymphomas have three. Both are very aggressive and need strong treatments.
Primary Mediastinal B-cell Lymphoma
PMBCL is a special type of DLBCL found in the chest. It often affects young adults, mostly women. It shares traits with Hodgkin lymphoma and is treated with a mix of immunotherapy and chemotherapy.
| Subtype | Characteristics | Prognosis |
|---|---|---|
| GCB DLBCL | Originates from germinal center B cells, favorable gene expression profile | Better prognosis |
| ABC DLBCL | Arises from activated B cells, aggressive clinical course | Poorer prognosis |
| Double/Triple-Hit Lymphomas | Presence of multiple genetic rearrangements | Highly aggressive, poor prognosis |
| Primary Mediastinal B-cell Lymphoma | Occurs in the mediastinum, often in young adults | Varies, often treated intensively |
Each DLBCL subtype is unique, needing a personalized treatment plan. Understanding these differences helps doctors provide better care for patients.
Signs and Symptoms of DLBCL
Knowing the signs and symptoms of DLBCL is key to better patient care. DLBCL often shows up with swollen lymph nodes, general body symptoms, and can affect other parts of the body too.
Rapidly Growing Lymph Node Swellings
DLBCL is known for its fast-growing lymph node swellings. These can be painless or painful. They usually appear in the neck, armpits, or groin. Many patients notice these changes before they see a doctor.
Extranodal Manifestations
DLBCL can also show up outside the lymph nodes. It can affect the stomach, intestines, or even the brain. Symptoms can include stomach pain, bowel issues, or brain problems.
B Symptoms: Fever, Night Sweats, and Weight Loss
B symptoms are common in DLBCL patients. These include fever, night sweats, and losing weight without trying. For more on DLBCL, check out Apollo247 for a detailed guide.
Organ-Specific Symptoms
The symptoms of DLBCL depend on the affected organs. For example, if the lymphoma hits the stomach, patients might feel nauseous, vomit, or have bowel changes.
| Symptom Category | Common Symptoms |
|---|---|
| Lymph Node Swellings | Painless or painful enlargements in neck, armpits, or groin |
| Extranodal Manifestations | Abdominal pain, gastrointestinal disturbances, neurological deficits |
| B Symptoms | Fever, night sweats, unintentional weight loss |
| Organ-Specific Symptoms | Nausea, vomiting, changes in bowel habits (depending on the organ involved) |
Risk Factors and Causes of D Cell Lymphoma Cancer
The exact causes of DLBCL are not fully known. But, research has found several risk factors that can increase the chance of getting this cancer. Knowing these factors is key for catching it early and possibly preventing it.
Genetic Predisposition
Genetics play a big role in DLBCL. People with a family history of lymphoma or other cancers might be at higher risk. Certain genetic changes, like in the MYC, BCL2, and BCL6 genes, also raise the risk.
Environmental Factors
Some environmental factors can also raise the risk of DLBCL. These include:
- Pesticide exposure: People exposed to pesticides, like those used in farming, have a higher risk.
- Chemical exposure: Being exposed to chemicals like solvents and dyes can also increase the risk.
- Ionizing radiation: Exposure to ionizing radiation, from things like radiation therapy or nuclear accidents, can raise the risk too.
Immune System Dysfunction
Another big risk factor is a weak immune system. Conditions like HIV/AIDS or autoimmune diseases can increase the risk. People who have had organ transplants and are on long-term immunosuppressive therapy are also at higher risk.
Prior Lymphoma or Cancer History
Having had lymphoma or other cancers before can also raise the risk of DLBCL. This might be because of shared risk factors or the effects of past treatments.
In summary, while we don’t know all the causes of DLBCL, knowing the risk factors helps with early detection. It also helps in finding ways to prevent and manage the disease.
Comprehensive Diagnosis of Non-Hodgkin DLBCL
Diagnosing Non-Hodgkin DLBCL is a detailed process. It includes an initial check, biopsy, imaging, and molecular tests. We’ll walk you through this journey, showing why a detailed approach is key.
Initial Assessment and Physical Examination
The first step is a detailed medical history and physical check. We look for signs like swollen lymph nodes, fever, and weight loss. This helps us find any issues that need more looking into.
Key components of the initial assessment include:
- Medical history to identify risk factors and previous conditions
- Physical examination to detect lymphadenopathy and other signs
- Laboratory tests to evaluate blood counts and biochemical markers
Biopsy and Pathological Evaluation
A biopsy is essential for diagnosing DLBCL. We take tissue samples from affected areas for examination. The samples are then checked for lymphoma cells and their characteristics.
The pathological evaluation involves:
- Histological examination to identify the lymphoma subtype
- Immunohistochemistry to characterize the cell surface markers
- Molecular studies to detect genetic abnormalities
Experts say, “The diagnosis of DLBCL relies heavily on the integration of morphological, immunophenotypic, and genetic features.”
“Accurate diagnosis is critical for selecting the appropriate treatment strategy and improving patient outcomes.”
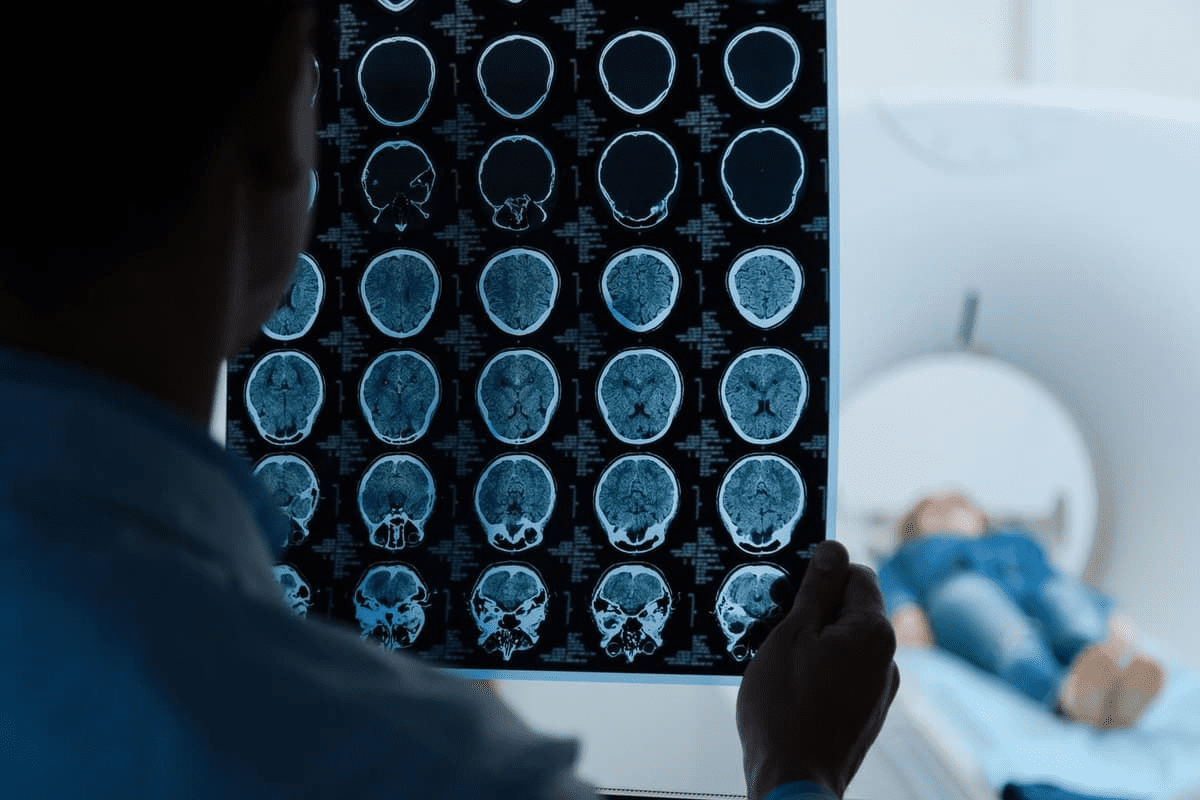
Advanced Imaging Studies
Advanced imaging like CT scans, PET scans, and MRI are key. They help us see how far the disease has spread. This helps us understand the extent of the disease.
| Imaging Modality | Role in DLBCL Diagnosis |
|---|---|
| CT Scan | Assesses lymph node involvement and extranodal disease |
| PET Scan | Evaluates metabolic activity of lymphoma cells |
| MRI | Provides detailed images of soft tissue involvement |
Molecular Profiling and Genetic Testing
Molecular profiling and genetic testing are vital. They help us understand the genetic makeup of DLBCL. This information guides treatment choices and helps predict outcomes.
Key aspects of molecular profiling include:
- Gene expression profiling to classify DLBCL subtypes
- Next-generation sequencing to detect genetic mutations
- FISH analysis to identify chromosomal rearrangements
By combining the results from initial checks, biopsy, imaging, and molecular tests, we can accurately diagnose and subtype DLBCL. This sets the stage for personalized treatment plans.
Staging and Prognostic Factors for DLBC Cancer
Accurate staging and understanding prognostic factors are key to managing DLBCL well. We use these to tailor treatments to each patient’s needs.
Ann Arbor Staging System
The Ann Arbor Staging System is a common method for staging lymphomas, including DLBCL. It divides the disease into four stages. These stages are based on how many lymph nodes are involved and if there are systemic symptoms.
- Stage I: Involvement of a single lymph node group or lymphoid structure.
- Stage II: Involvement of two or more lymph node groups on the same side of the diaphragm.
- Stage III: Involvement of lymph node groups on both sides of the diaphragm.
- Stage IV: Diffuse or disseminated involvement of one or more extralymphatic organs.
International Prognostic Index (IPI)
The International Prognostic Index (IPI) predicts the outcome of DLBCL patients. It considers several factors:
- Age of the patient
- Performance status
- Stage of the disease
- Number of extranodal sites involved
- Lactate dehydrogenase (LDH) levels
These factors help sort patients into different risk groups. This guides treatment decisions.
Cell of Origin Classification
The cell of origin classification is a key prognostic factor in DLBCL. It divides the lymphoma into:
- Germinal Center B-cell-like (GCB) DLBCL: Generally associated with a better prognosis.
- Activated B-cell-like (ABC) DLBCL: Often associated with a poorer prognosis.
Knowing the cell of origin helps choose the best treatment approach.
Genetic Markers and Their Significance
Genetic markers are vital in DLBCL prognosis. Certain genetic abnormalities, like MYC and BCL2 rearrangements, greatly affect disease outcome. Patients with “double-hit” or “triple-hit” lymphomas often face a worse prognosis.
Understanding these staging systems and prognostic factors helps manage DLBCL better. It’s essential to include this information in a detailed treatment plan.
Treatment Approaches for B Cell Diffuse Lymphoma
We are seeing big changes in how we treat DLBCL. Now, we focus on treatments that are more effective and targeted. There are many options, from standard treatments to new ones like CAR T-cell therapy.
Standard First-Line Immunochemotherapy
The usual treatment for DLBCL is a mix of chemotherapy and immunotherapy, called immunochemotherapy. The most common mix is R-CHOP. It includes rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone. This mix has greatly improved patient outcomes.
Rituximab targets the CD20 protein on B cells, helping to destroy them. Adding rituximab to CHOP has led to better survival rates.
Treatment for Refractory or Relapsed DLBCL
For patients with refractory or relapsed DLBCL, treatments are more challenging. Second-line treatments might include salvage chemotherapy and stem cell transplantation for eligible patients.
Those who don’t respond to initial treatment or relapse early face a tougher road. They might benefit from clinical trials or new therapies.
Stem Cell Transplantation Options
Stem cell transplantation, like autologous stem cell transplantation (ASCT), is a possible cure for relapsed or refractory DLBCL. ASCT uses the patient’s own stem cells, collected before high-dose chemotherapy.
CAR T-Cell Therapy and Emerging Treatments
CAR T-cell therapy is a big step forward in treating DLBCL. It modifies T cells to attack cancer cells. Several CAR T-cell products have been approved for relapsed or refractory DLBCL, giving new hope to those who’ve tried other treatments.
New treatments, like bispecific antibodies and checkpoint inhibitors, are being tested in trials. They aim to improve outcomes for DLBCL patients even more.
The future of DLBCL treatment will likely be more personalized. Therapies will be tailored to each patient’s cancer.
Managing Side Effects and Supportive Care During Treatment
Supportive care is key to improving life quality for DLBCL patients. It’s vital to tackle treatment side effects and offer full care. This is true for managing Diffuse Large B Cell Lymphoma.
Common Treatment Side Effects
DLBCL treatment can cause side effects, from mild to severe. These include fatigue, nausea, hair loss, and a higher risk of infections. We’ll help patients manage these side effects well.
| Side Effect | Management Strategy |
|---|---|
| Fatigue | Rest, gentle exercise, and nutritional support |
| Nausea | Anti-nausea medication, dietary adjustments |
| Hair Loss | Counseling, scalp cooling techniques |
Supportive Medications
Supportive meds are key in handling side effects. For example, anti-emetics fight nausea. Growth factors help by boosting white blood cells and lowering infection risk.
Nutrition and Lifestyle Considerations
Nutrition is vital for DLBCL patients. A balanced diet helps manage side effects and aids recovery. We suggest talking to a nutritionist for a tailored diet plan.
- Eat small, frequent meals to manage nausea
- Stay hydrated by drinking plenty of fluids
- Include a variety of fruits and vegetables in your diet
Psychological Support Resources
DLBCL diagnosis and treatment can be tough emotionally. We offer psychological support, like counseling and support groups. This helps patients deal with emotional challenges.
By focusing on physical, nutritional, and mental health, we can greatly enhance DLBCL patients’ quality of life. Our all-encompassing care ensures patients get the support they need to manage their treatment journey.
Conclusion: Prognosis, Survivorship, and Future Directions
Knowing about DLBCL is key for those diagnosed with this type of non-Hodgkin lymphoma (NHL DLBCL). DLBCL is a serious and aggressive lymphoma that needs quick and effective treatment. Thanks to new treatments, the outlook for patients with D cell lymphoma cancer has gotten much better.
Surviving DLBCL is a big part of its care. Patients need ongoing support and checks to deal with treatment side effects and stop the cancer from coming back. As research keeps moving forward, we’ll see new ways to fight NHL DLBCL, like targeted therapies and CAR T-cell treatments.
The importance of knowledge and new ideas in fighting DLBCL can’t be overstated. Just like money makes trade easier, using the best treatments and practices can greatly help patients. We’re excited for the future of DLBCL research and care, which will keep making life better for those with this disease.
FAQ
What is Diffuse Large B Cell Lymphoma (DLBCL)?
DLBCL is a fast-growing type of non-Hodgkin lymphoma. It grows in large B cells. It’s a serious cancer that affects the immune system and needs quick medical help.
What are the symptoms of DLBCL?
Symptoms include fast-growing lymph node swellings and B symptoms like fever and weight loss. The lymphoma can also affect other parts of the body.
How is DLBCL diagnosed?
Doctors use a detailed process to diagnose DLBCL. This includes a physical exam, biopsy, and advanced imaging. They also do molecular profiling.
What are the subtypes of DLBCL?
DLBCL has several subtypes. These include Germinal Center B-cell-like (GCB) and Activated B-cell-like (ABC) DLBCL. There are also Double-Hit and Triple-Hit Lymphomas and Primary Mediastinal B-cell Lymphoma.
What are the risk factors for developing DLBCL?
Risk factors include genetic predisposition and environmental factors. Immune system issues and a history of lymphoma or cancer also increase risk.
How is DLBCL staged?
DLBCL is staged using the Ann Arbor Staging System. This helps doctors understand how far the disease has spread. The International Prognostic Index (IPI) and cell of origin classification are also important.
What are the treatment options for DLBCL?
Treatments include first-line immunochemotherapy and options for refractory or relapsed DLBCL. Stem cell transplantation and CAR T-cell therapy are also available.
What is the importance of supportive care during DLBCL treatment?
Supportive care is key for managing side effects. It includes using supportive medications and focusing on nutrition and lifestyle. Psychological support is also important.
What does the future hold for DLBCL treatment and research?
Research and new treatments, like immunotherapy and targeted therapies, are improving DLBCL outcomes. These advancements are promising for the future.
How can patients with DLBCL manage their condition effectively?
Effective management involves understanding the disease and following treatment plans. A healthy lifestyle and support from healthcare providers and groups are also important.
Reference
FAQ
What is Diffuse Large B Cell Lymphoma (DLBCL)?
DLBCL is a fast-growing type of non-Hodgkin lymphoma. It grows in large B cells. It’s a serious cancer that affects the immune system and needs quick medical help.
What are the symptoms of DLBCL?
Symptoms include fast-growing lymph node swellings and B symptoms like fever and weight loss. The lymphoma can also affect other parts of the body.
How is DLBCL diagnosed?
Doctors use a detailed process to diagnose DLBCL. This includes a physical exam, biopsy, and advanced imaging. They also do molecular profiling.
What are the subtypes of DLBCL?
DLBCL has several subtypes. These include Germinal Center B-cell-like (GCB) and Activated B-cell-like (ABC) DLBCL. There are also Double-Hit and Triple-Hit Lymphomas and Primary Mediastinal B-cell Lymphoma.
What are the risk factors for developing DLBCL?
Risk factors include genetic predisposition and environmental factors. Immune system issues and a history of lymphoma or cancer also increase risk.
How is DLBCL staged?
DLBCL is staged using the Ann Arbor Staging System. This helps doctors understand how far the disease has spread. The International Prognostic Index (IPI) and cell of origin classification are also important.
What are the treatment options for DLBCL?
Treatments include first-line immunochemotherapy and options for refractory or relapsed DLBCL. Stem cell transplantation and CAR T-cell therapy are also available.
What is the importance of supportive care during DLBCL treatment?
Supportive care is key for managing side effects. It includes using supportive medications and focusing on nutrition and lifestyle. Psychological support is also important.
What does the future hold for DLBCL treatment and research?
Research and new treatments, like immunotherapy and targeted therapies, are improving DLBCL outcomes. These advancements are promising for the future.
How can patients with DLBCL manage their condition effectively?
Effective management involves understanding the disease and following treatment plans. A healthy lifestyle and support from healthcare providers and groups are also important.